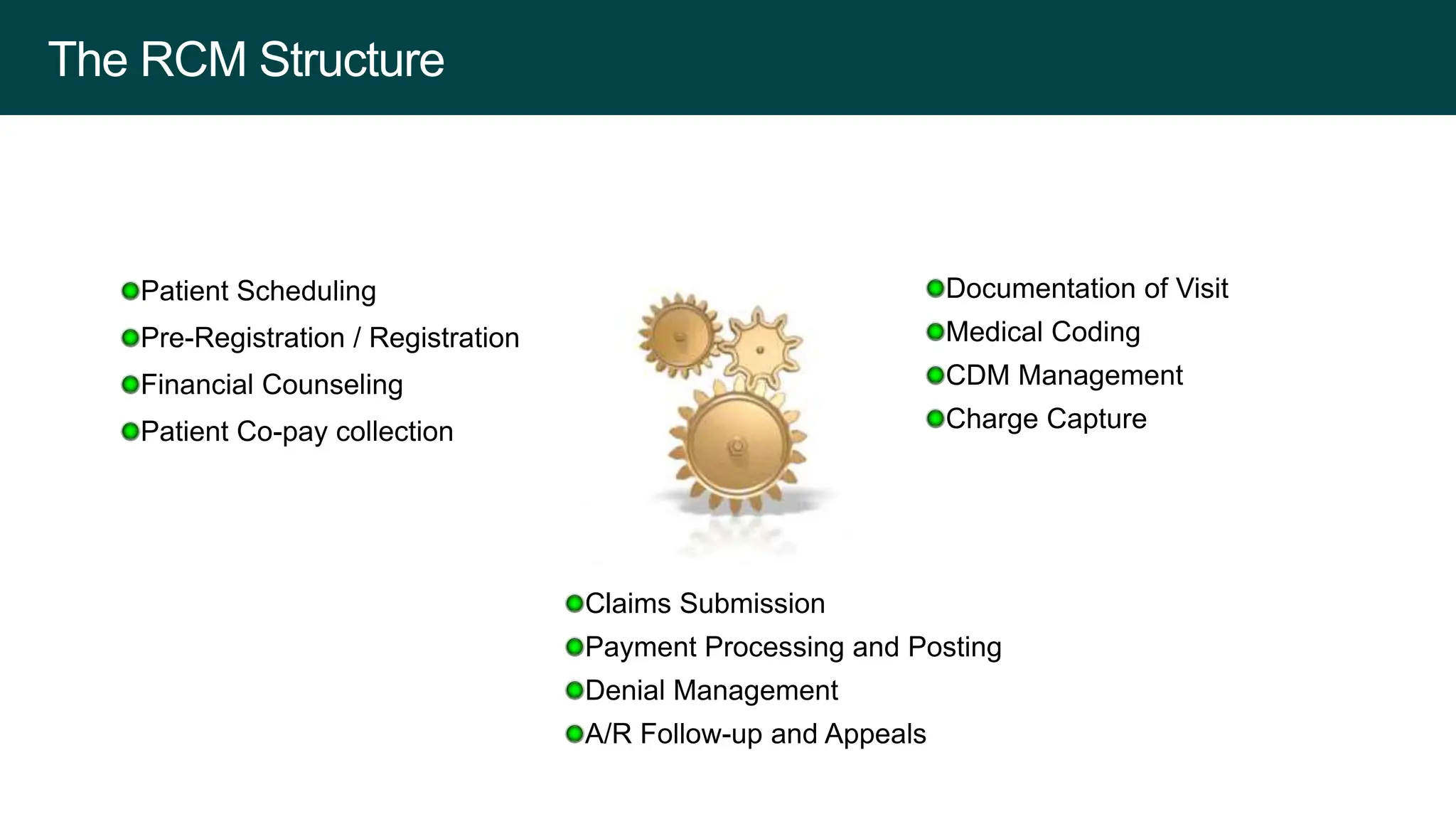
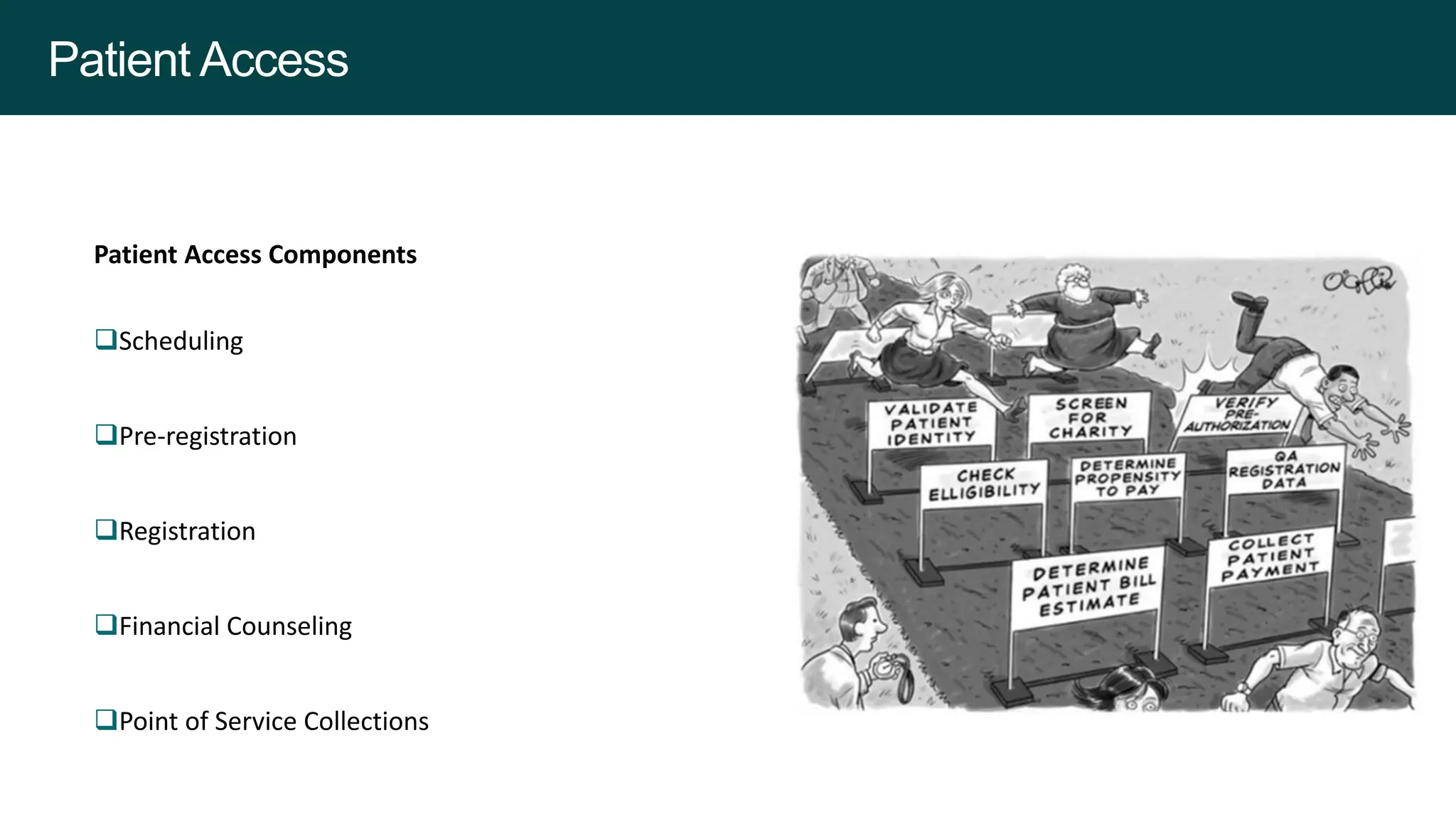
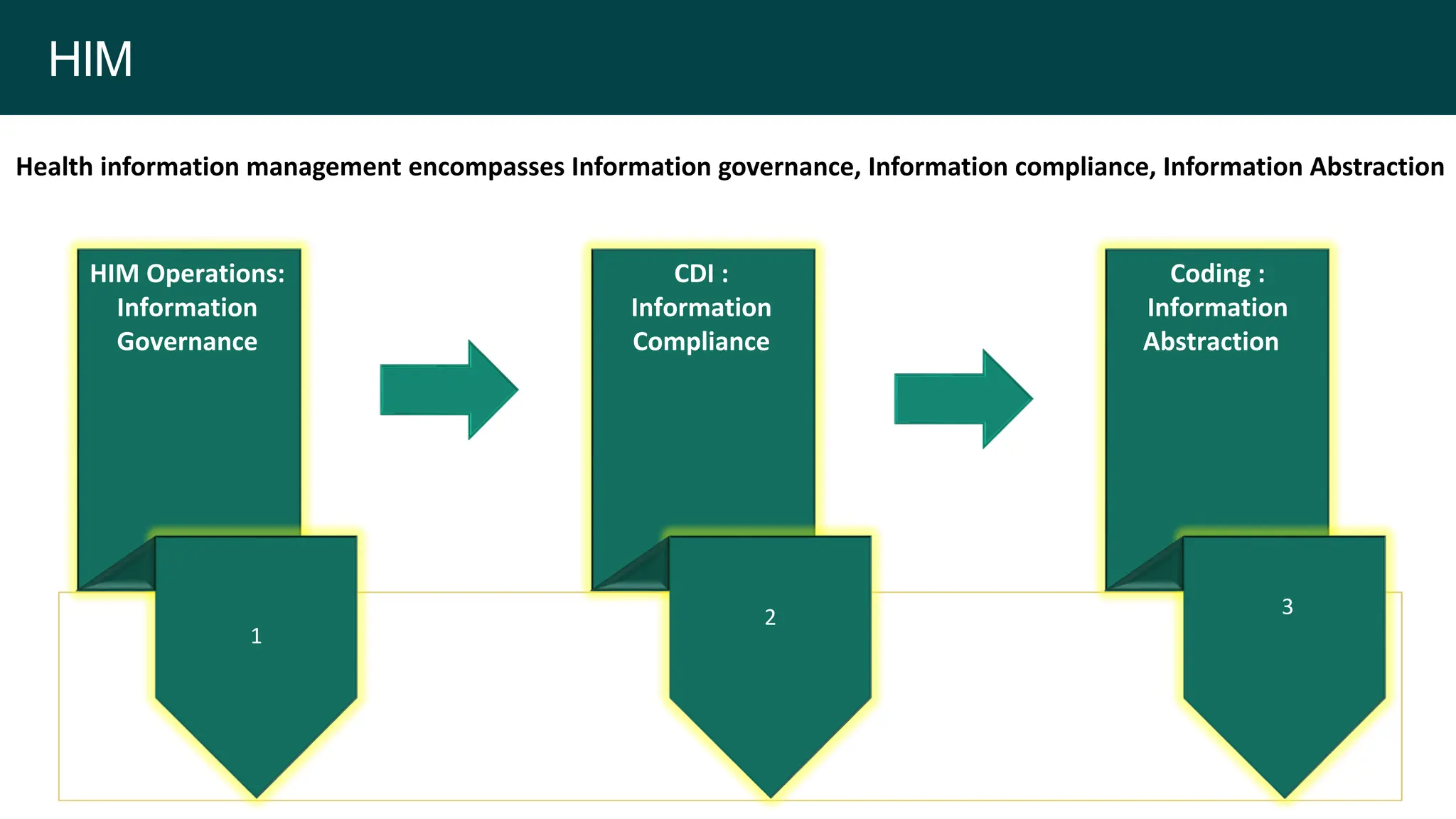
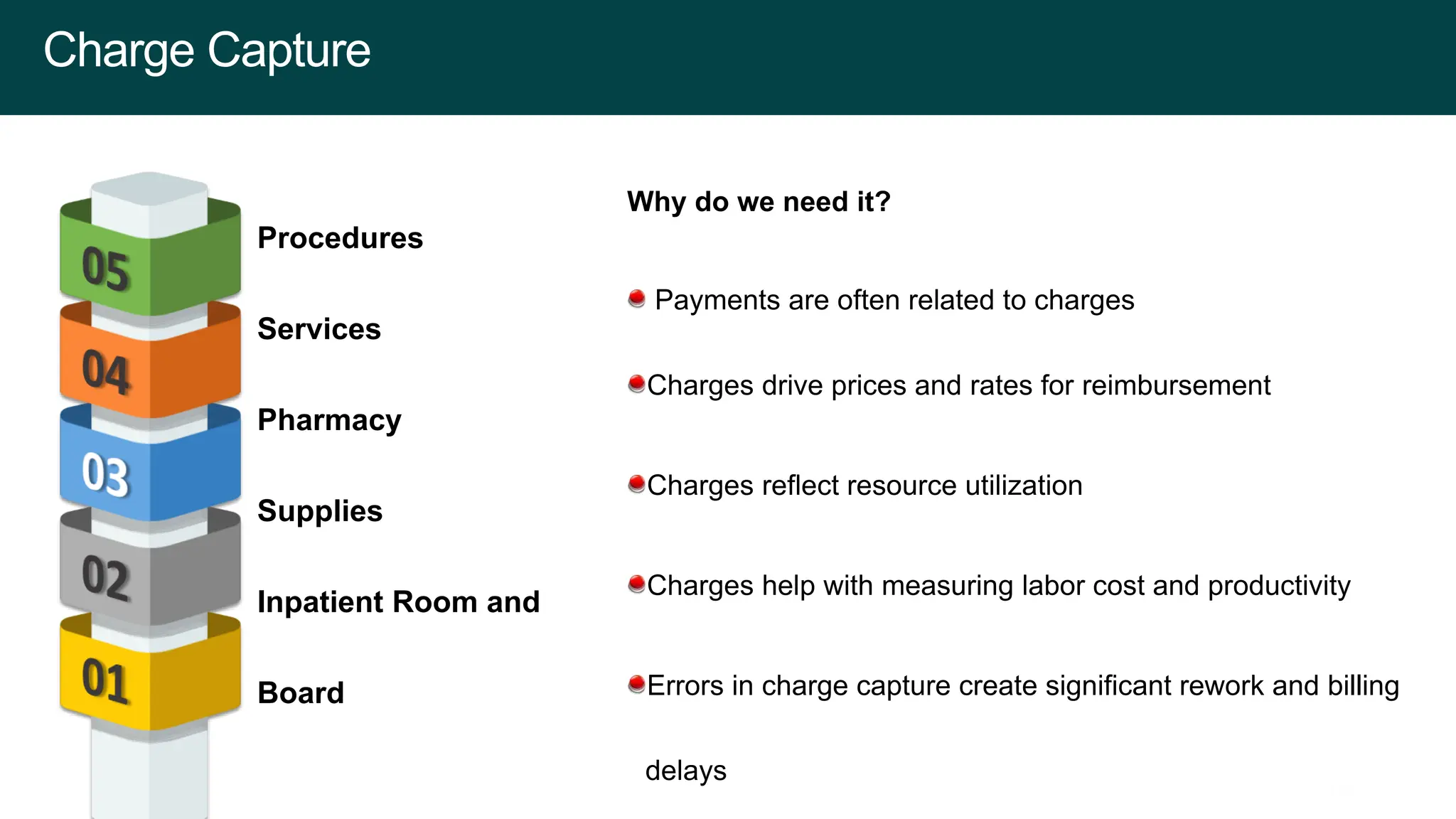
The document outlines the structure and challenges of Revenue Cycle Management (RCM), including elements such as charge capture, claims submission, denial management, and financial counseling. It emphasizes the importance of documenting physician practices, maintaining an accurate Charge Description Master (CDM), and managing accounts receivable effectively to improve financial stability. It also addresses the role of analytics in assessing performance and highlights the need for quality improvement and staff training to address common challenges in health information management.