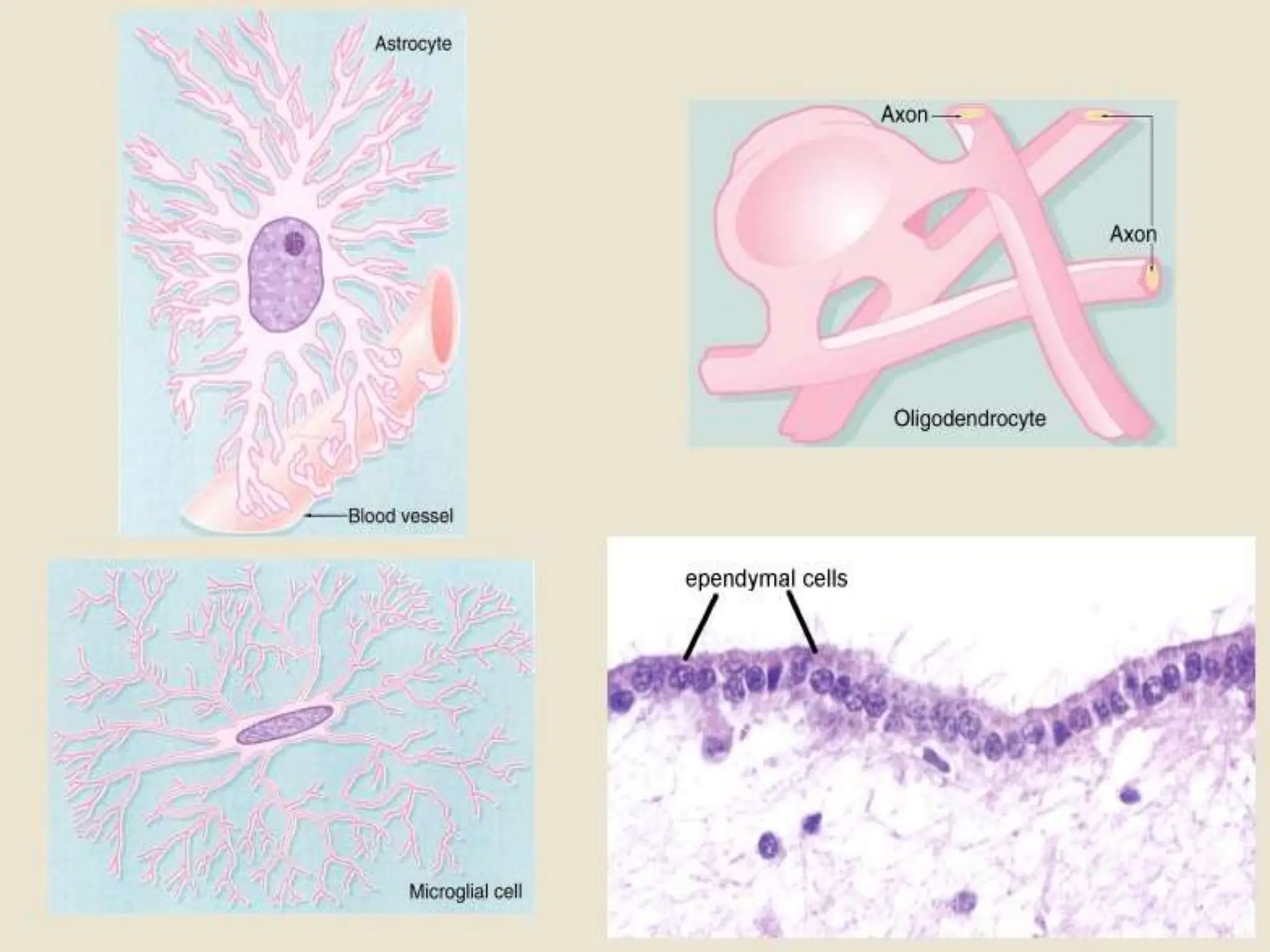
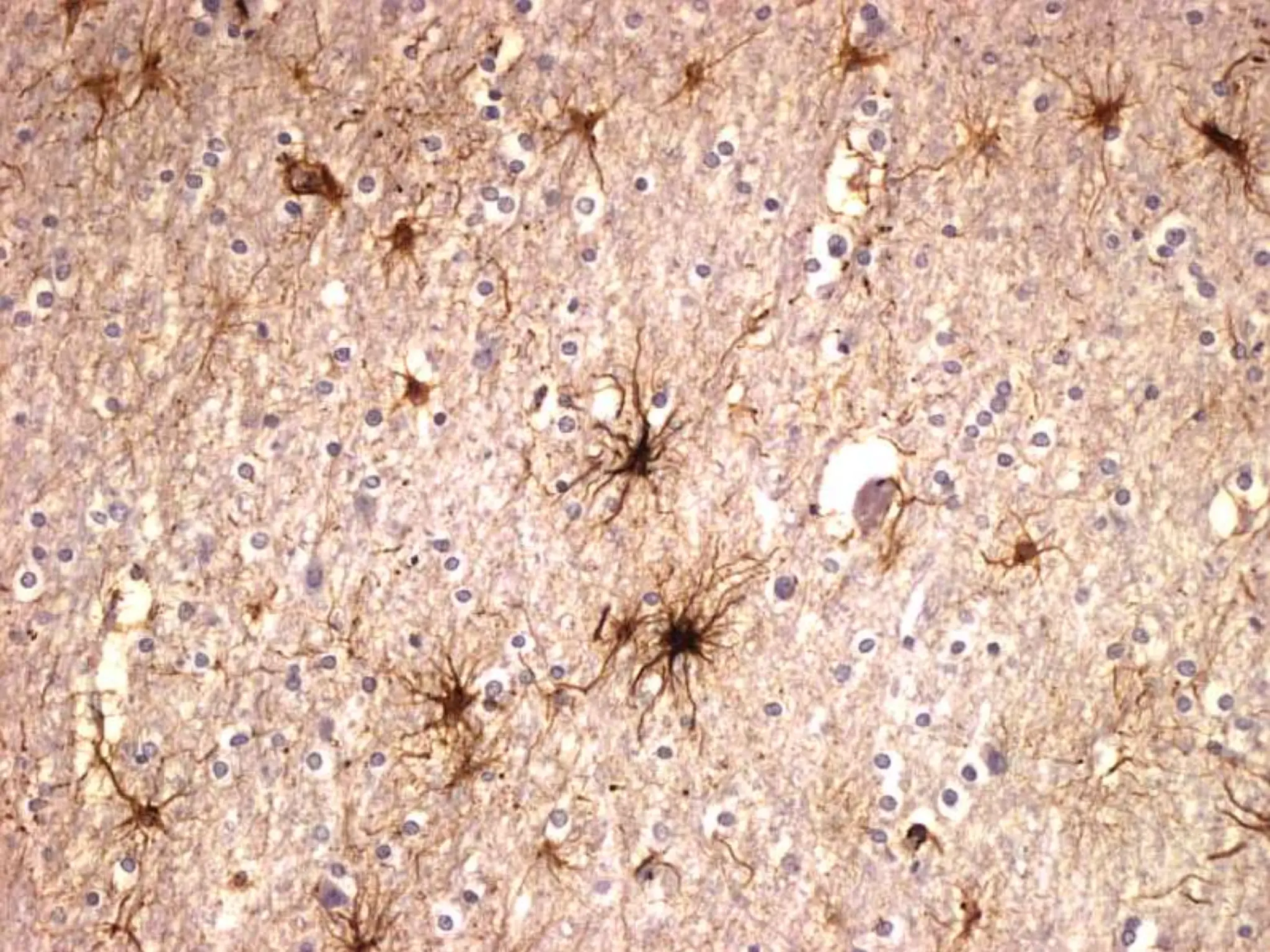
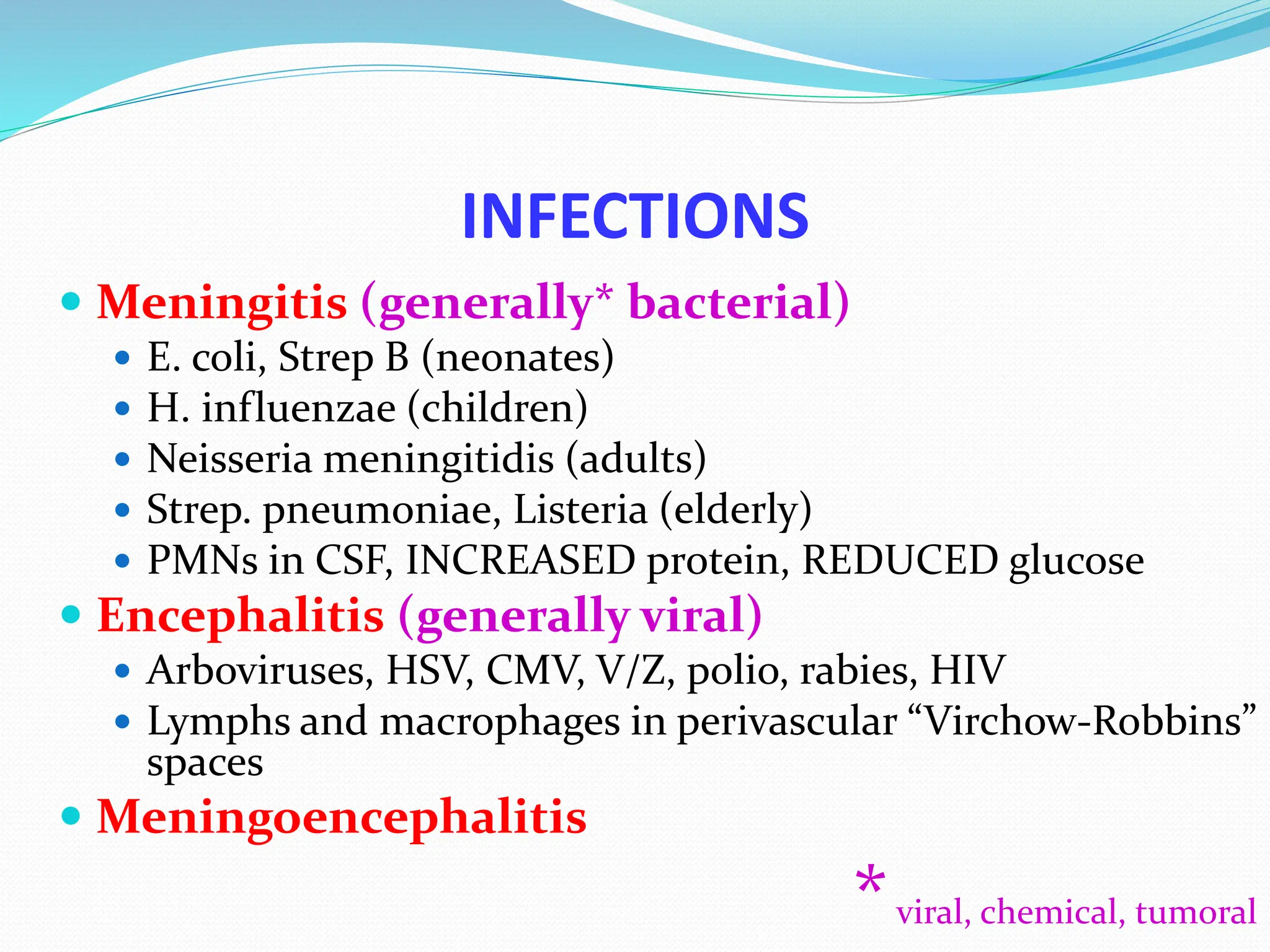
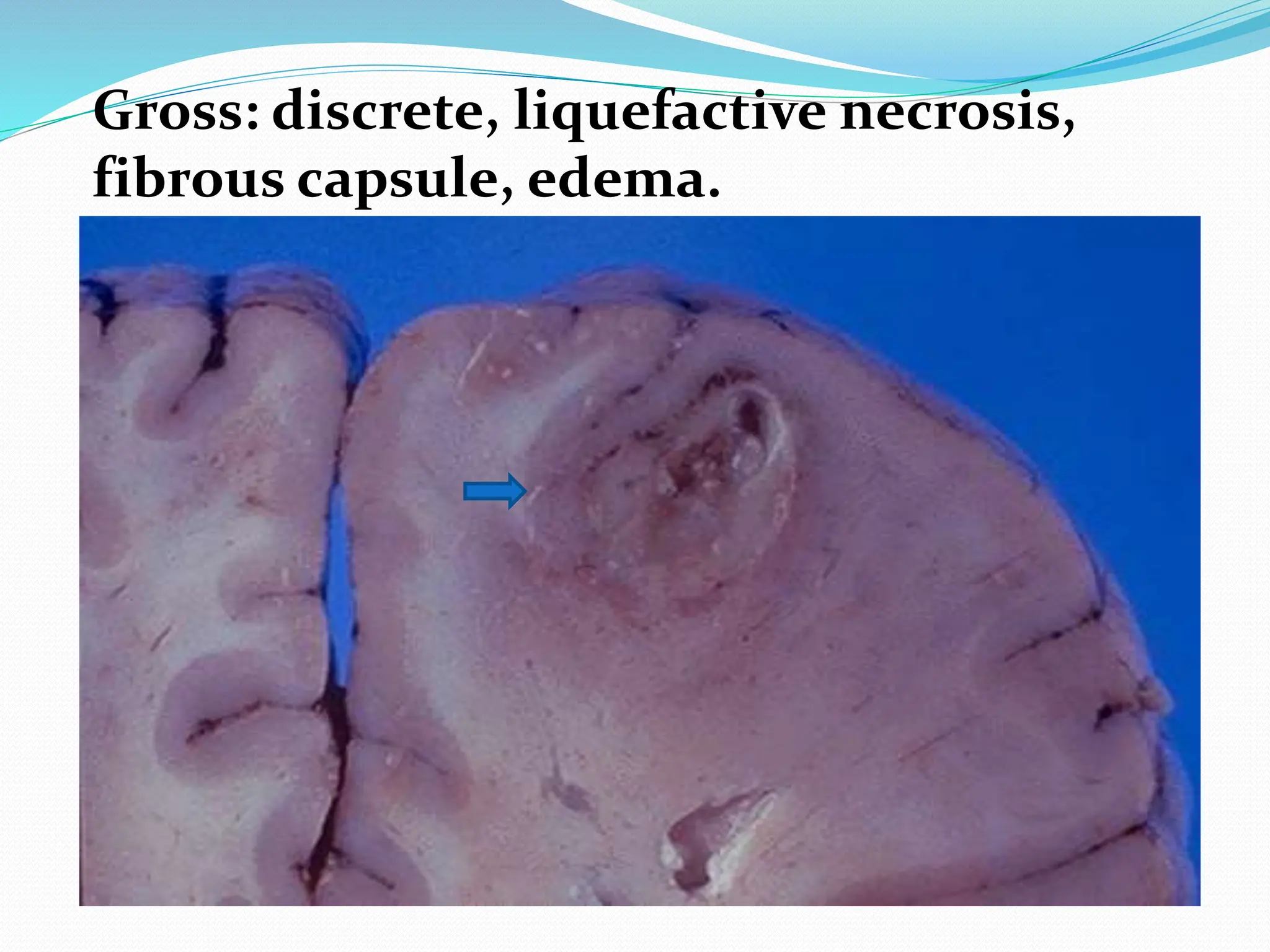
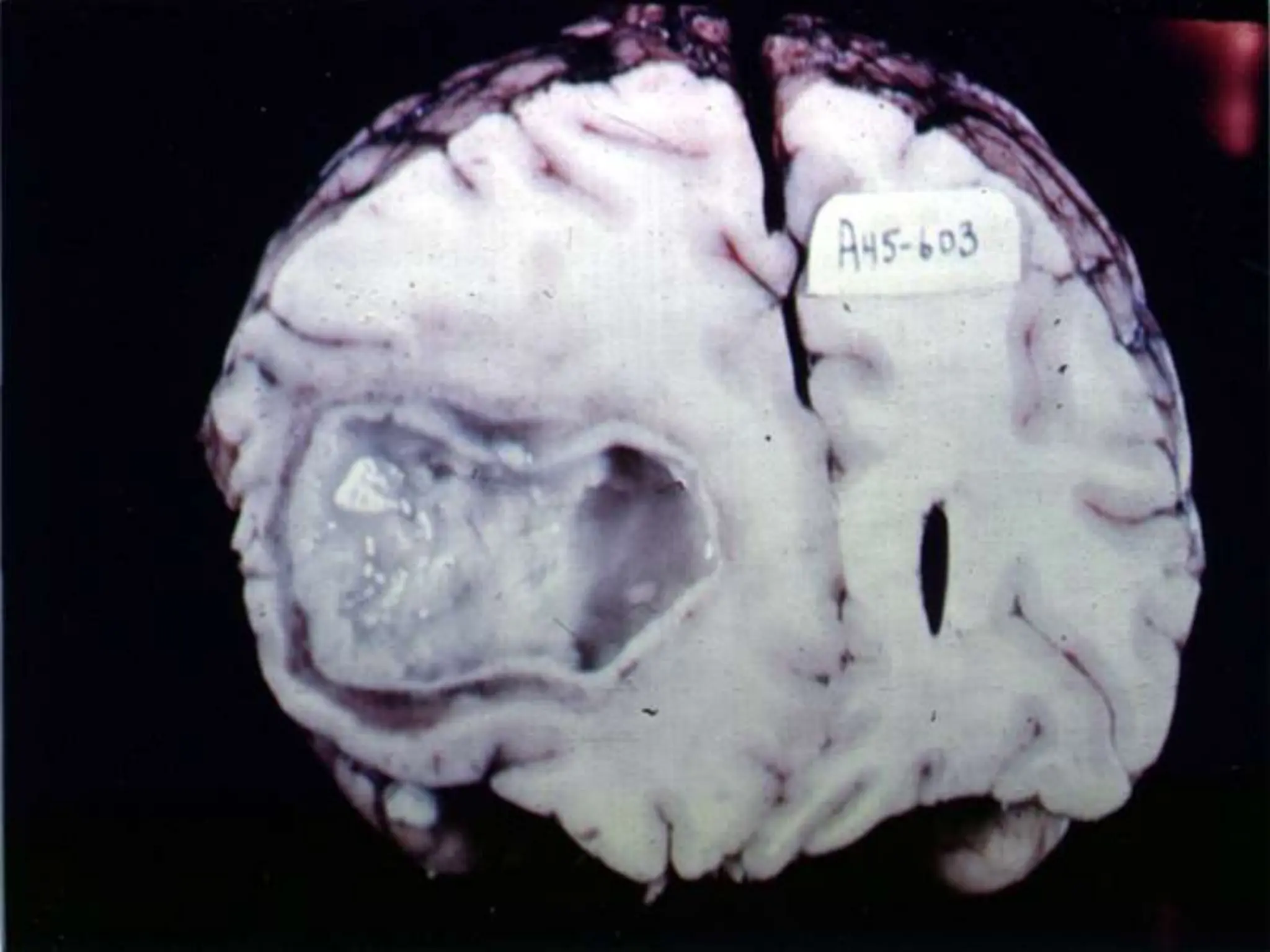
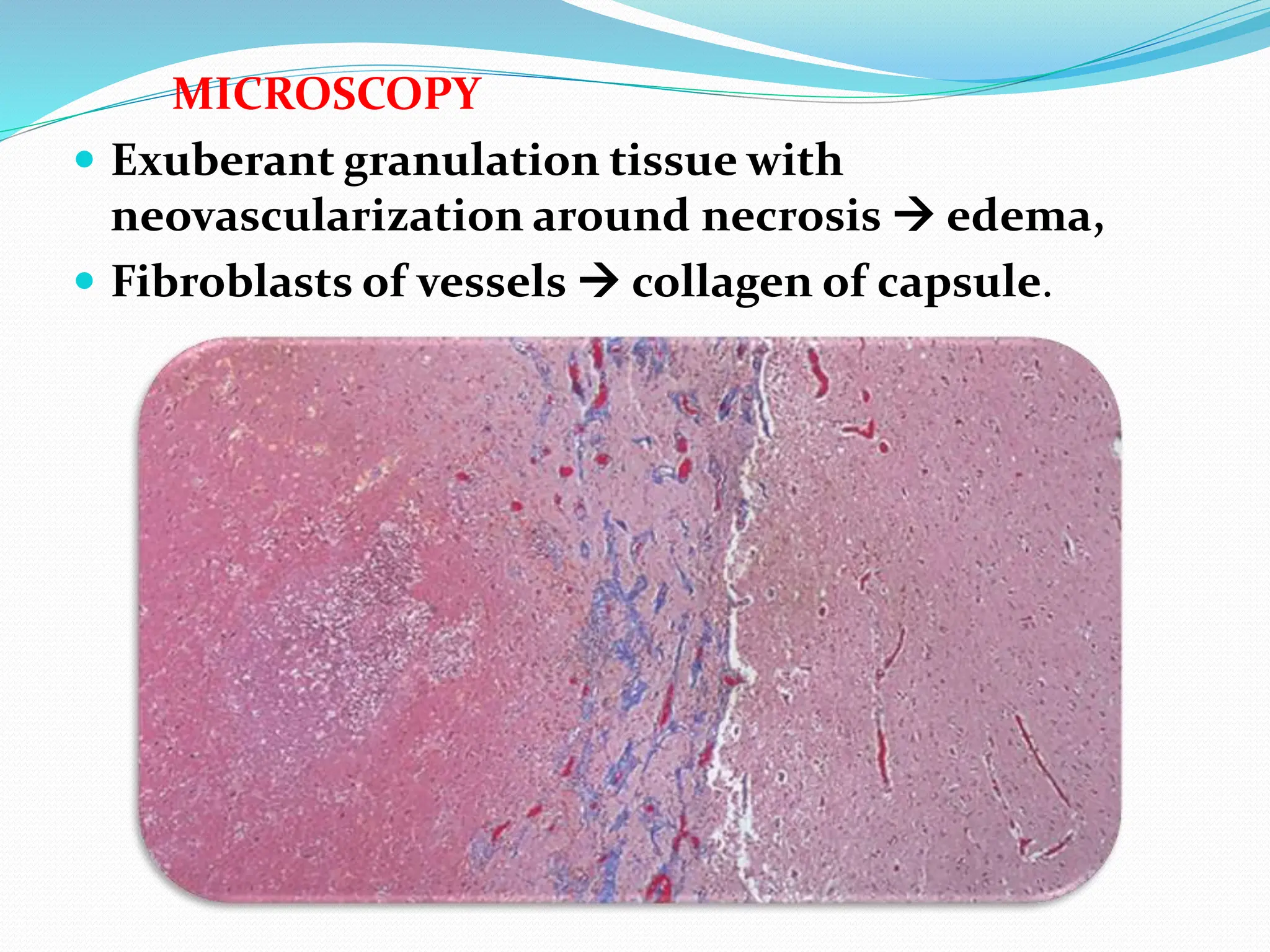
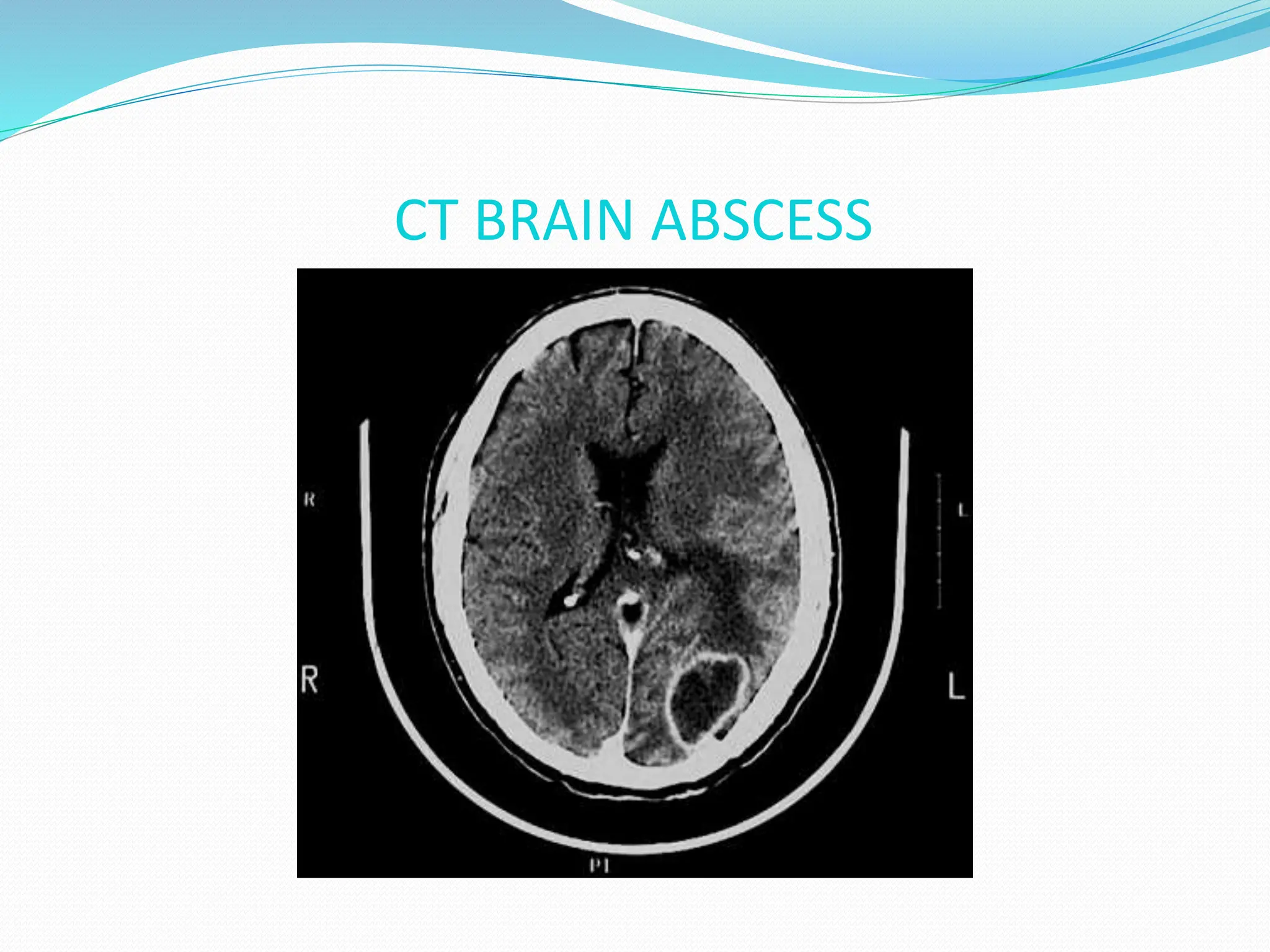
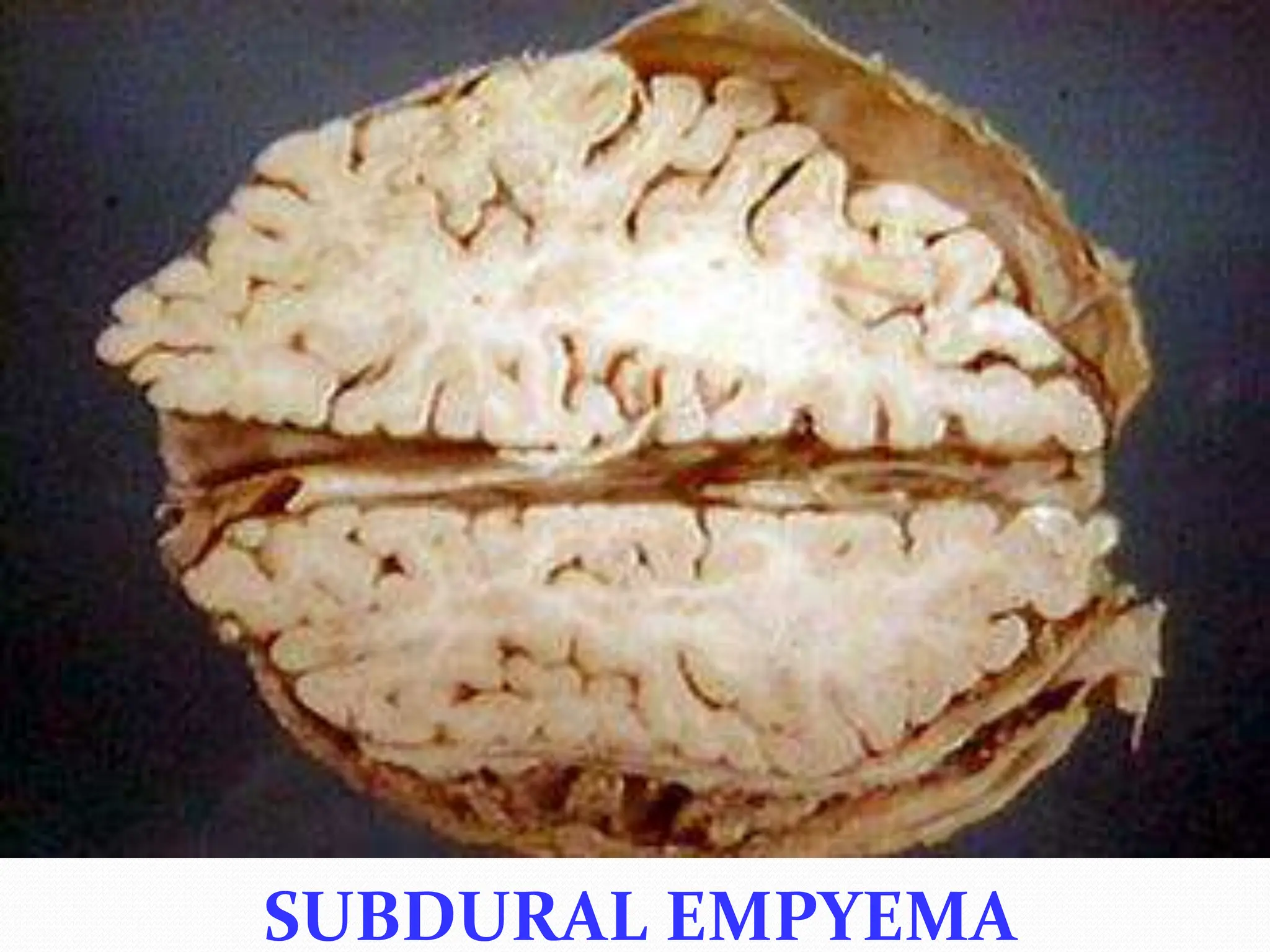
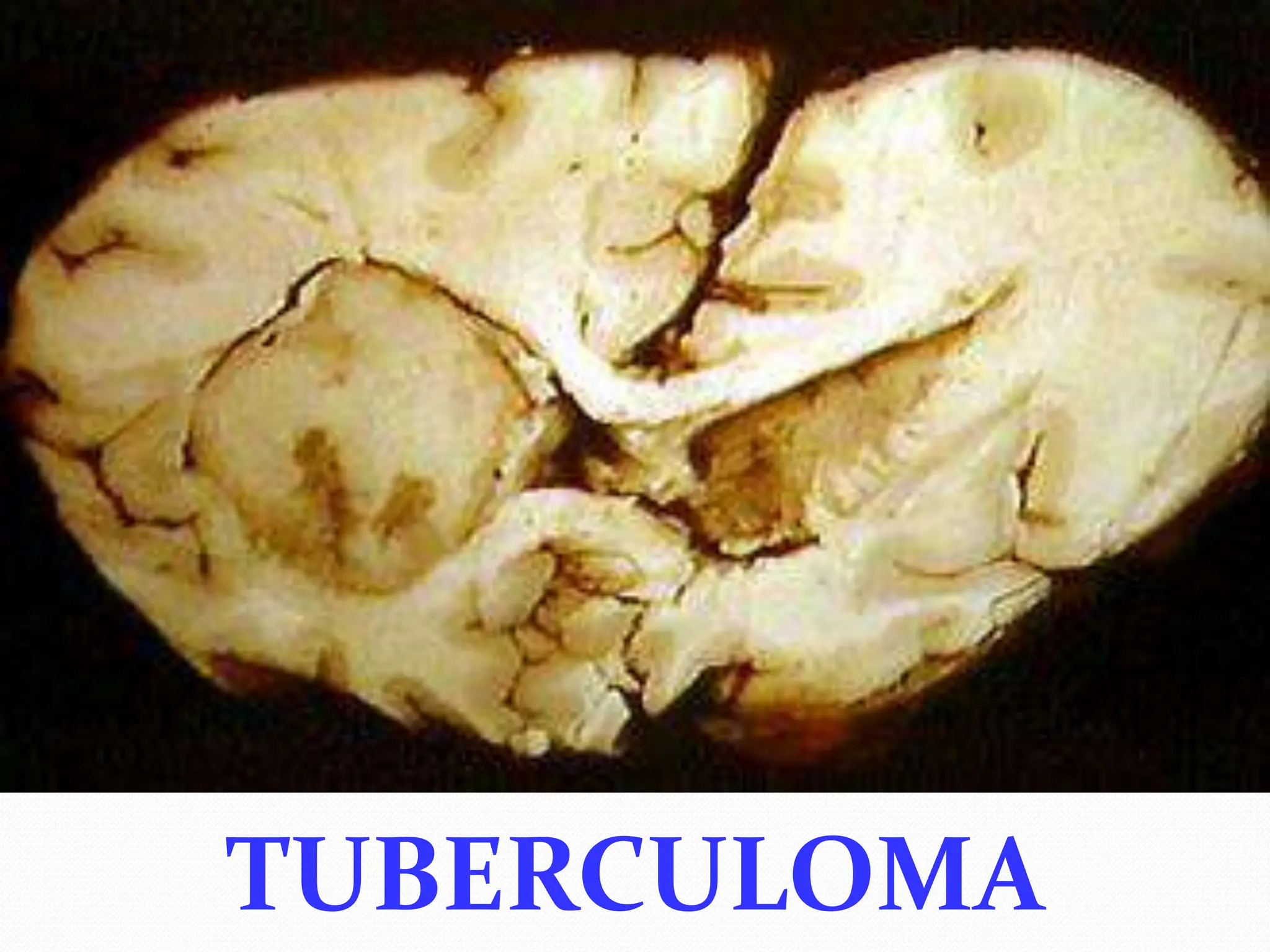
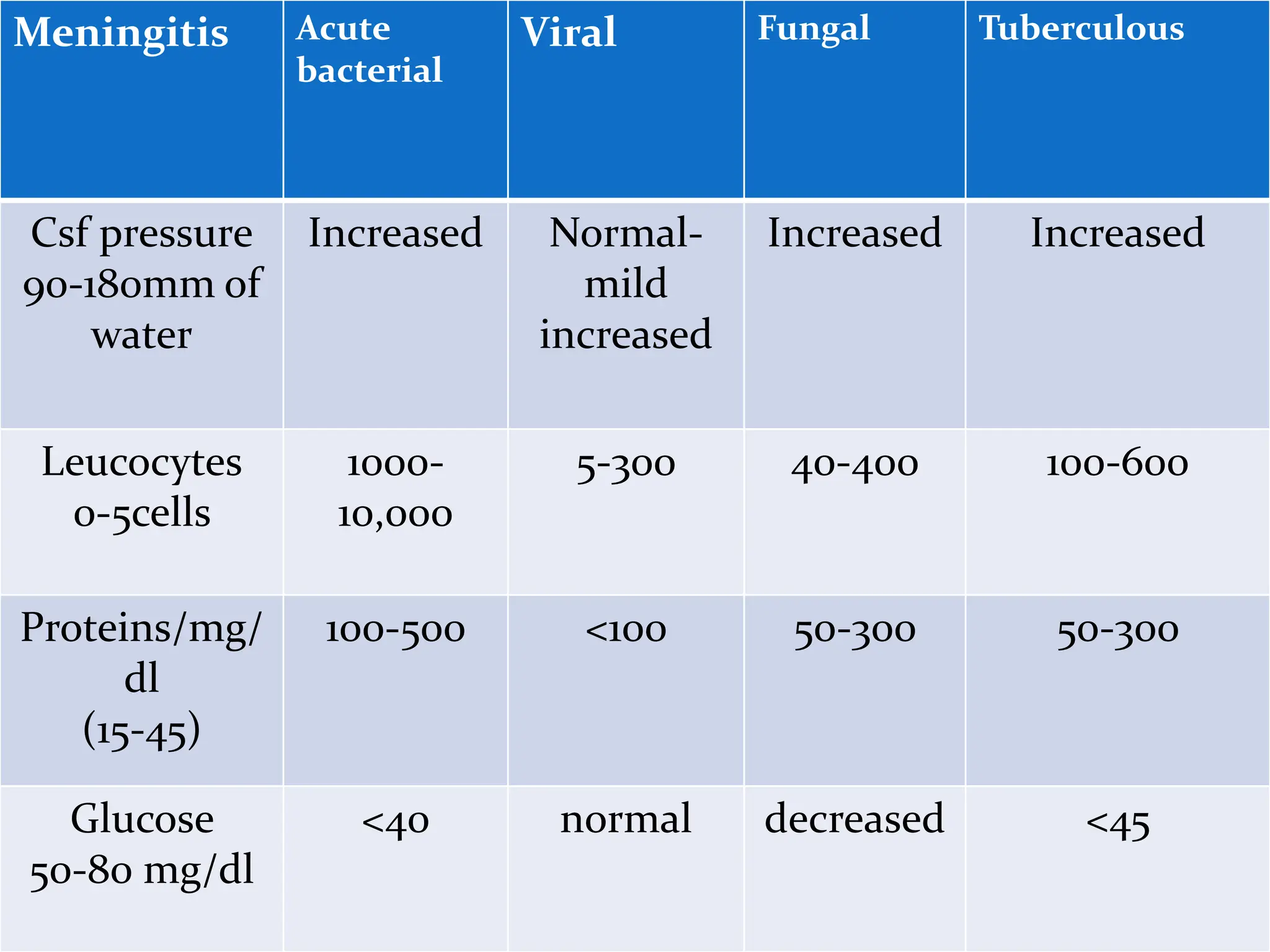
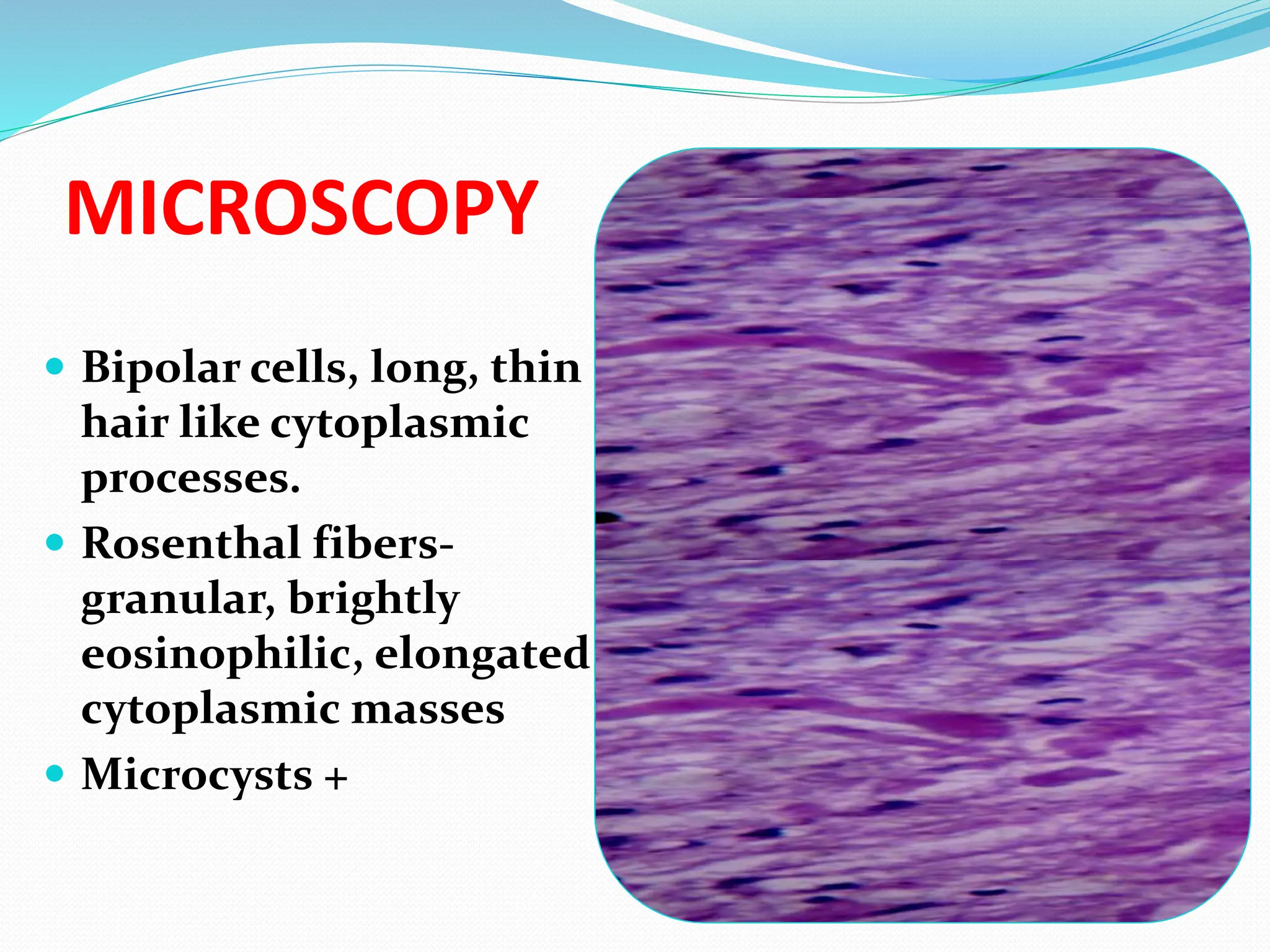
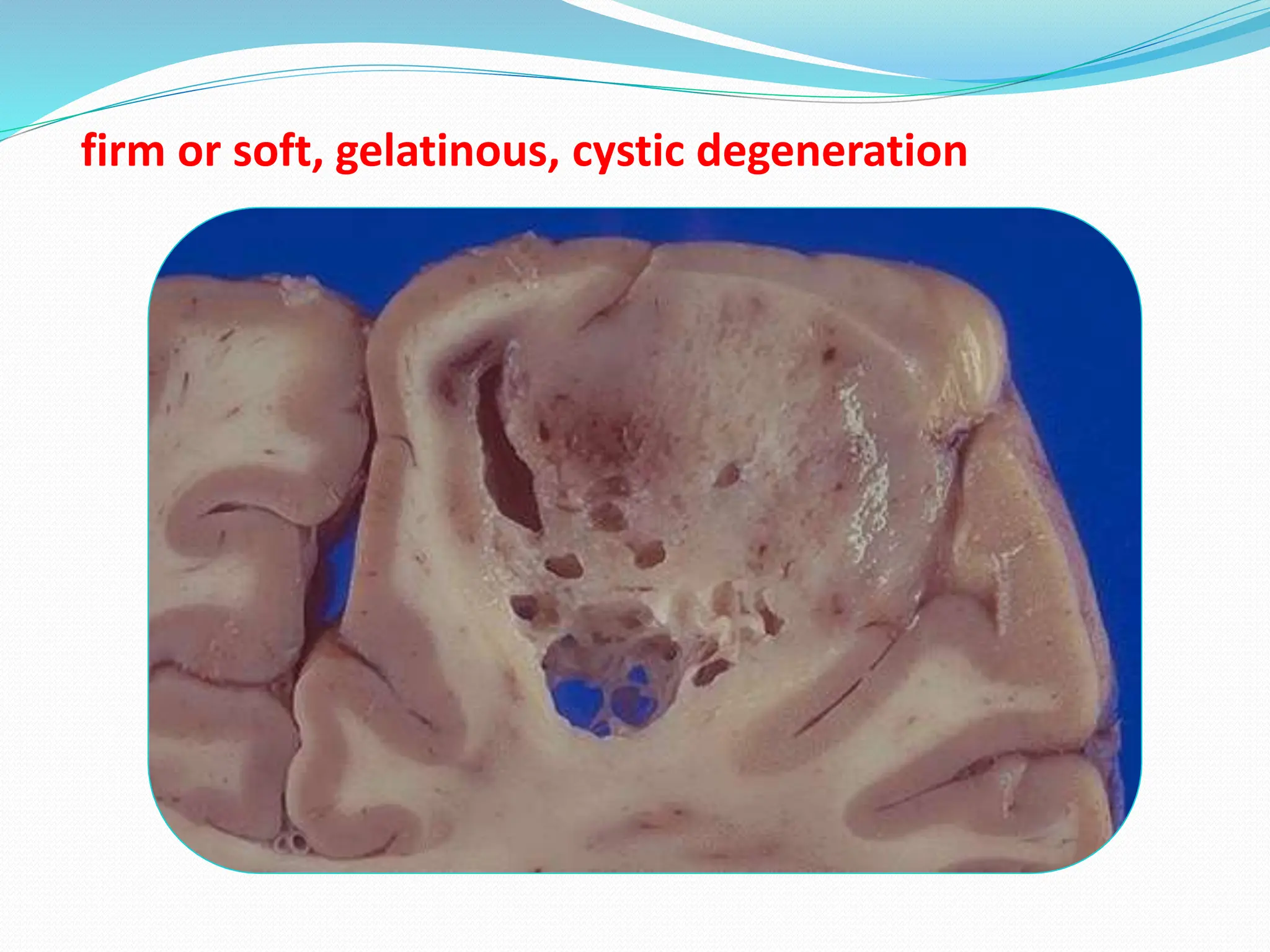
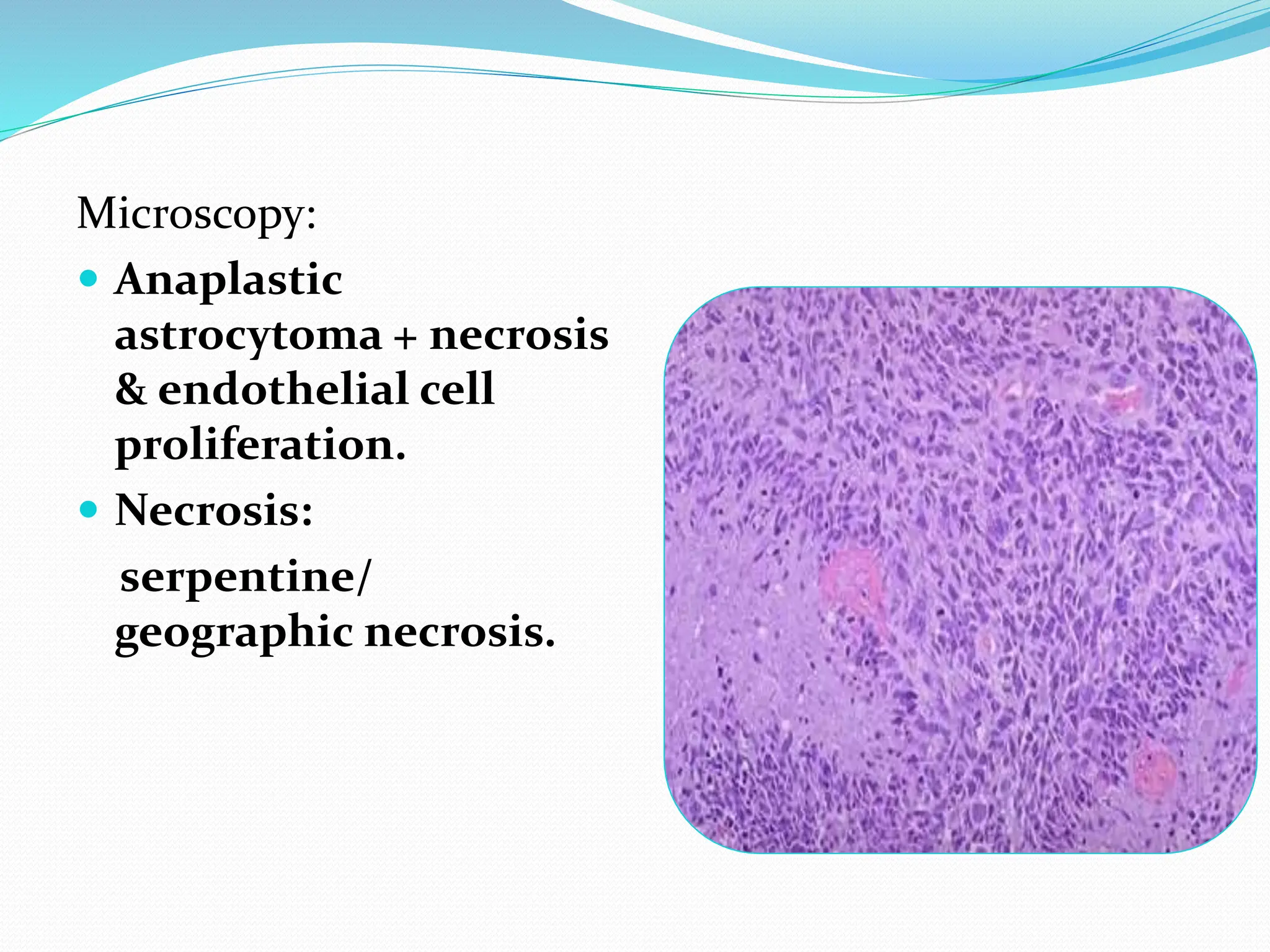
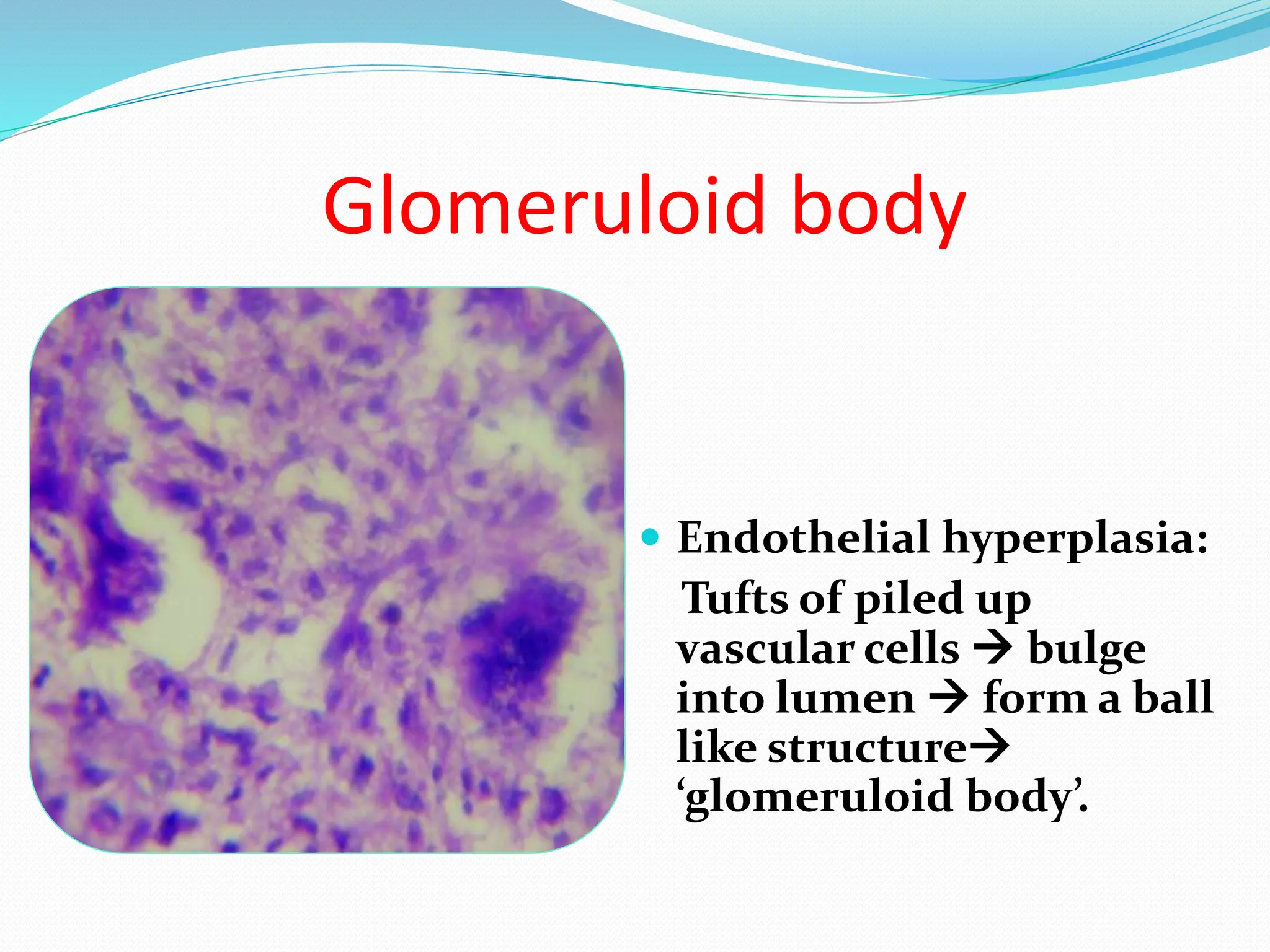
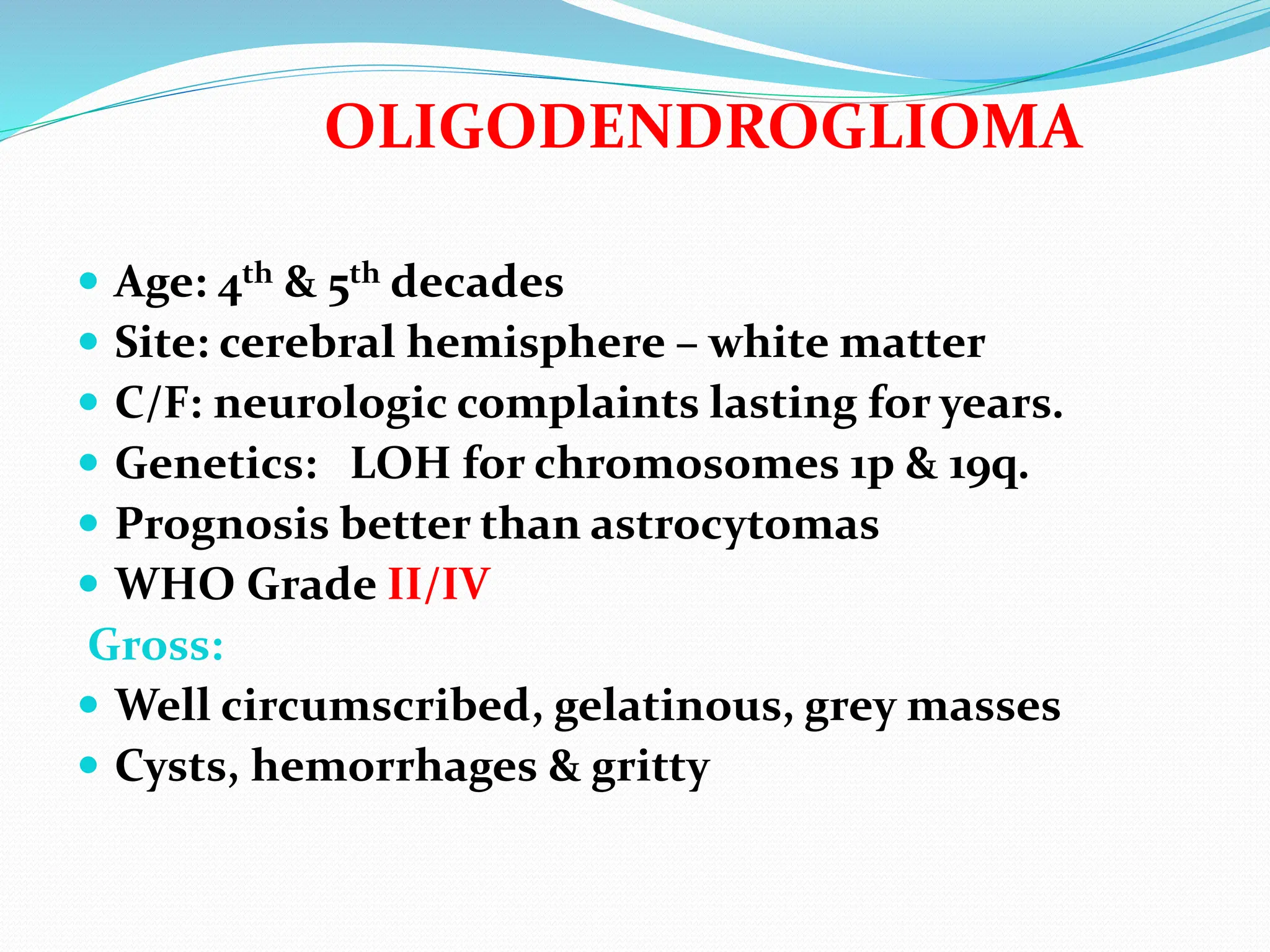
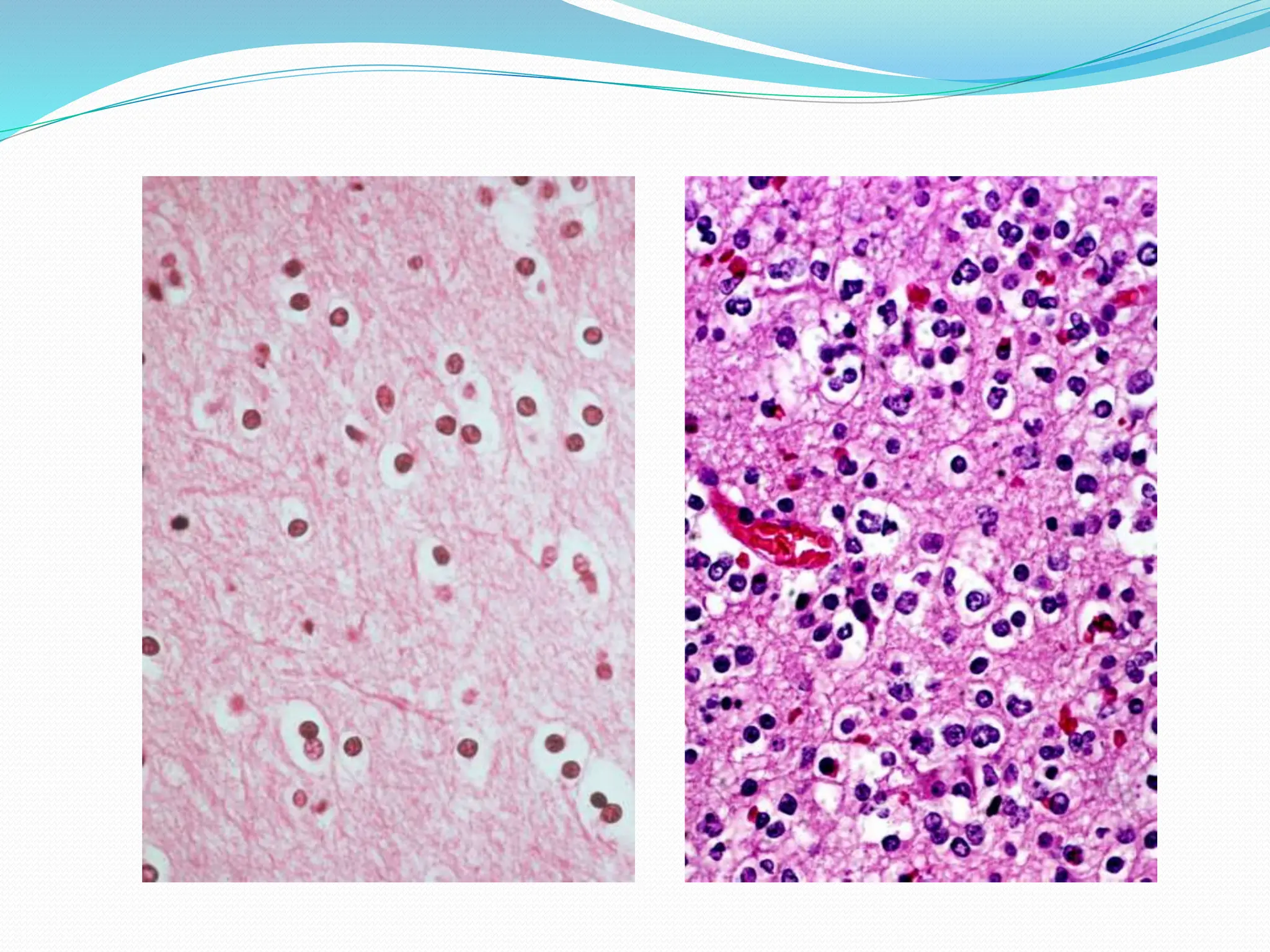
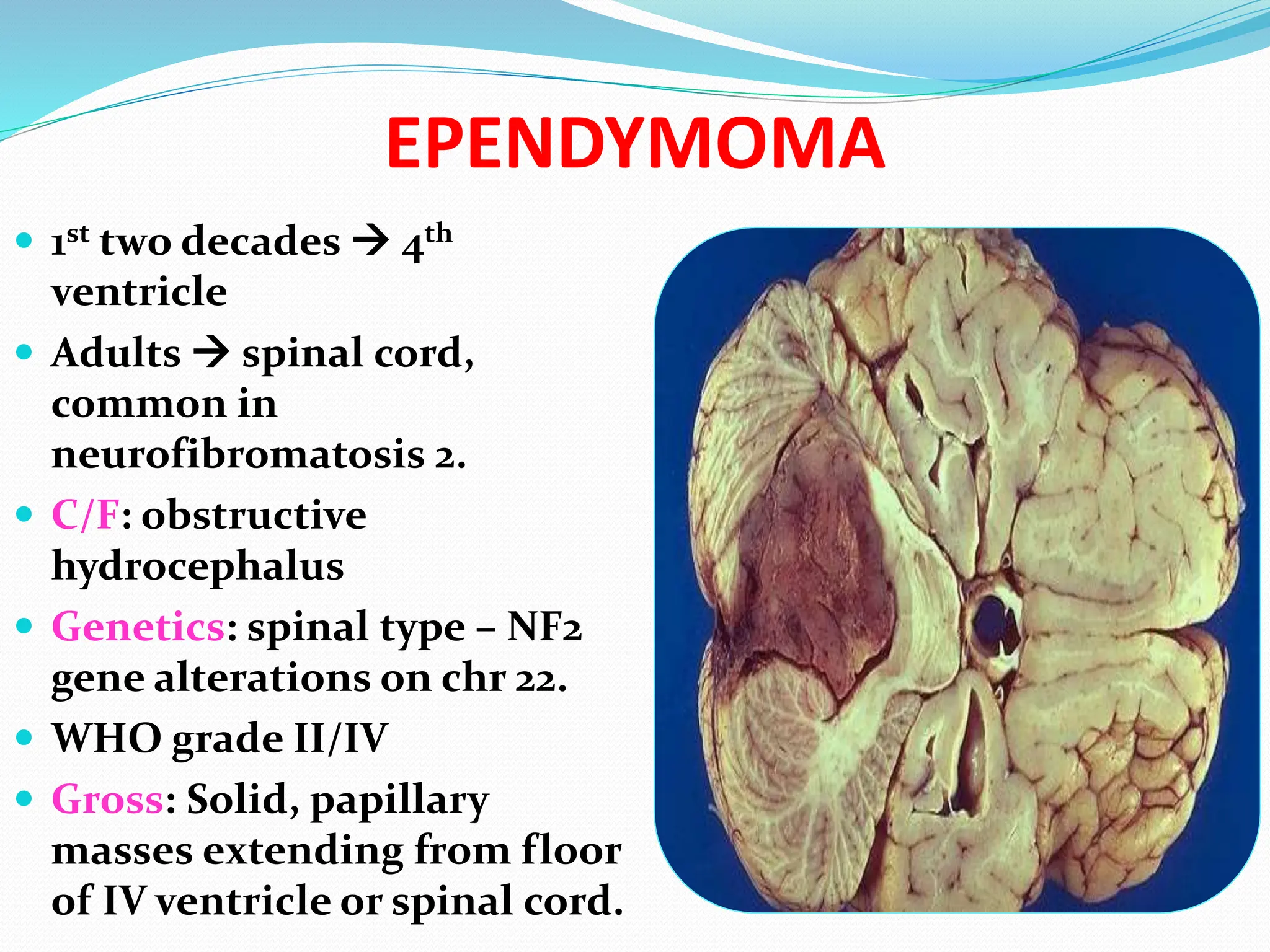
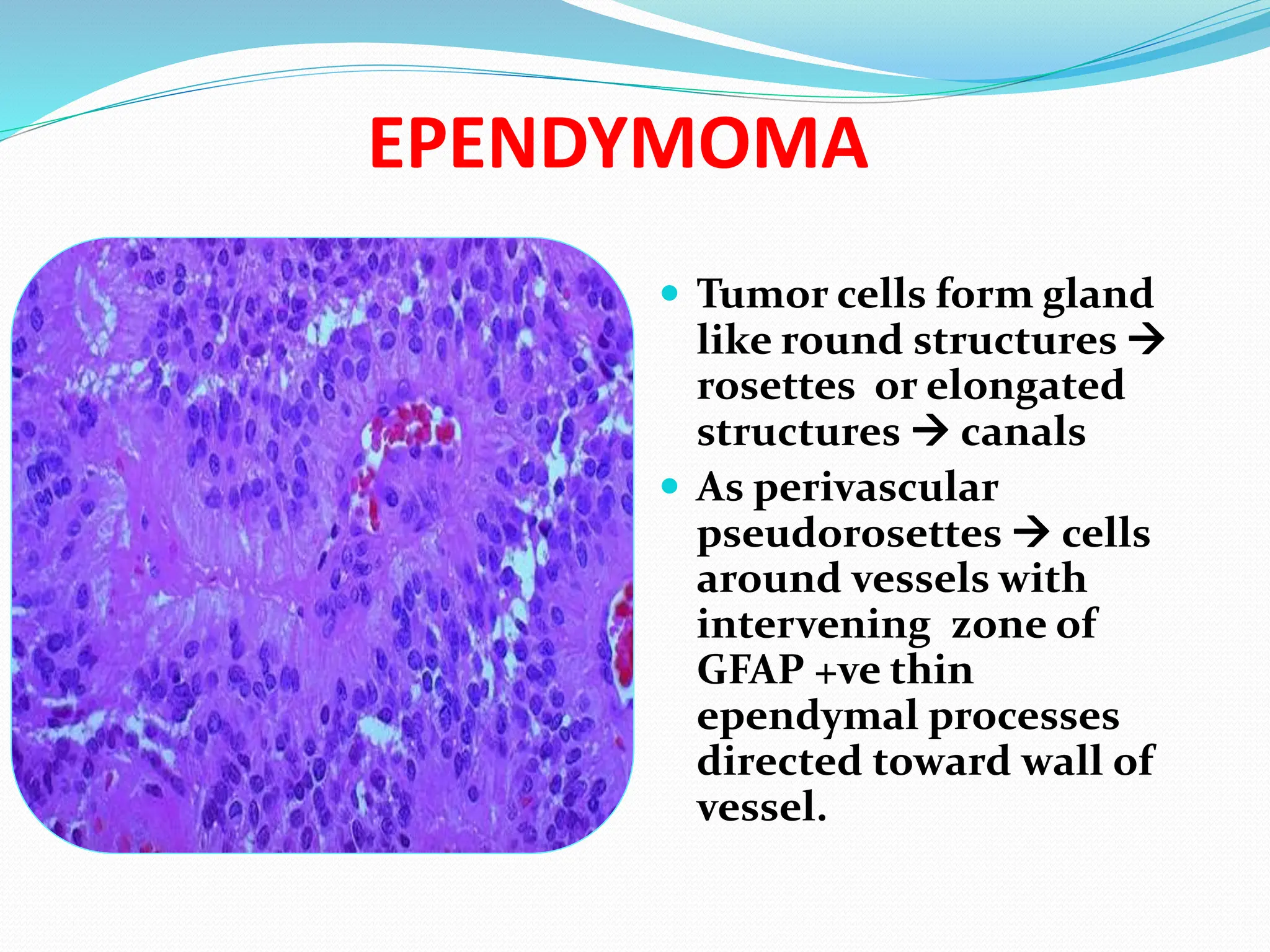
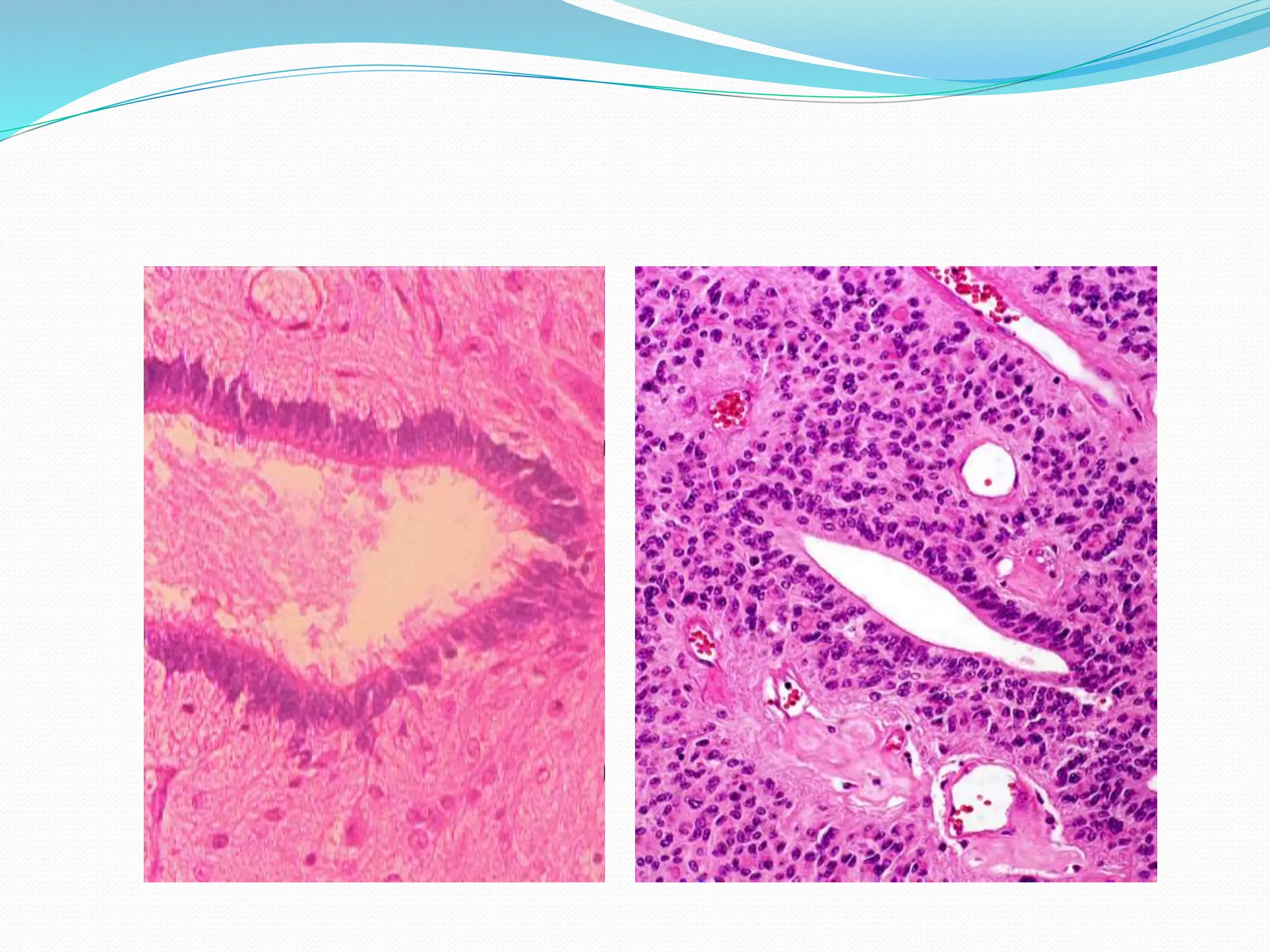
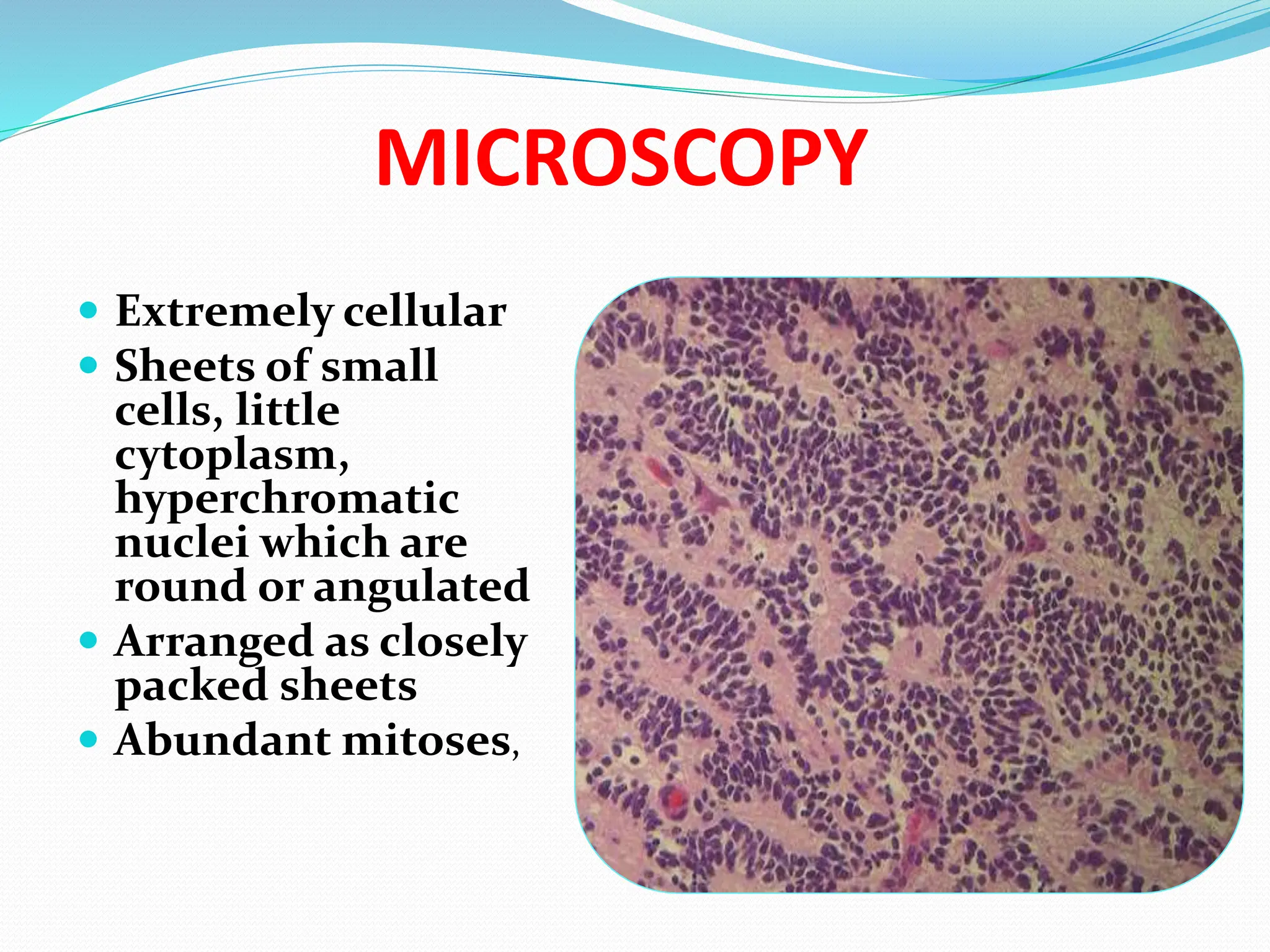
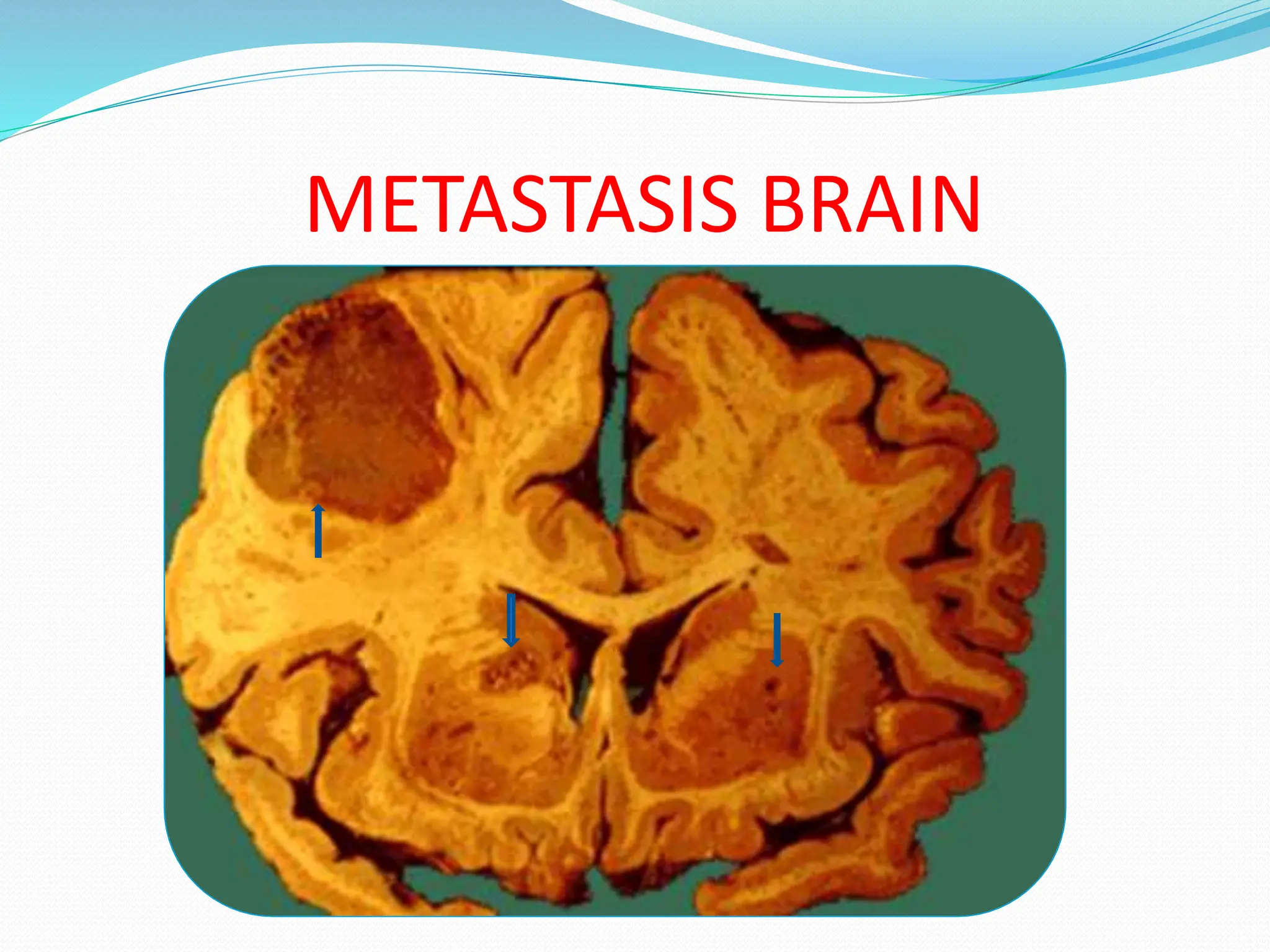
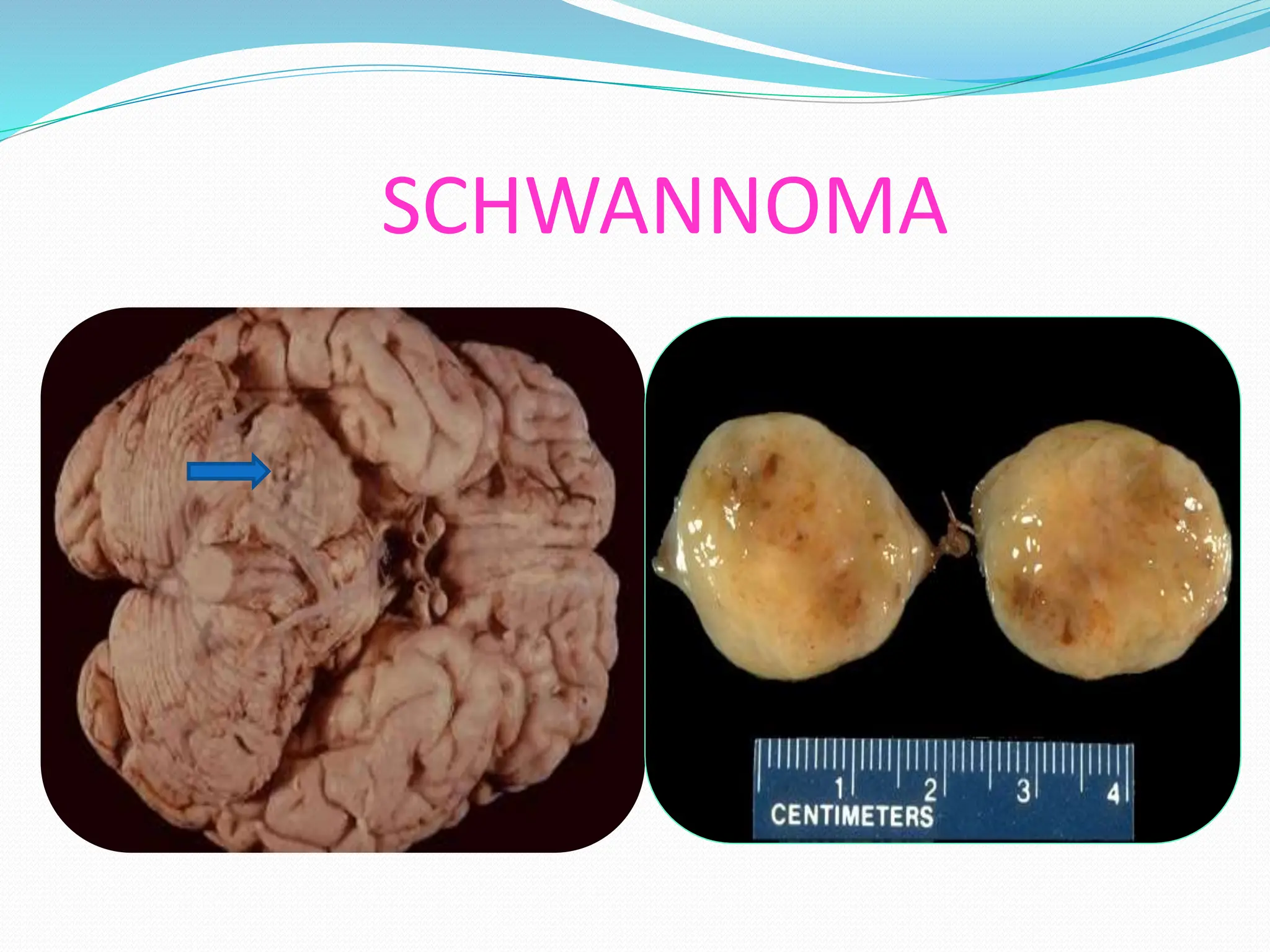
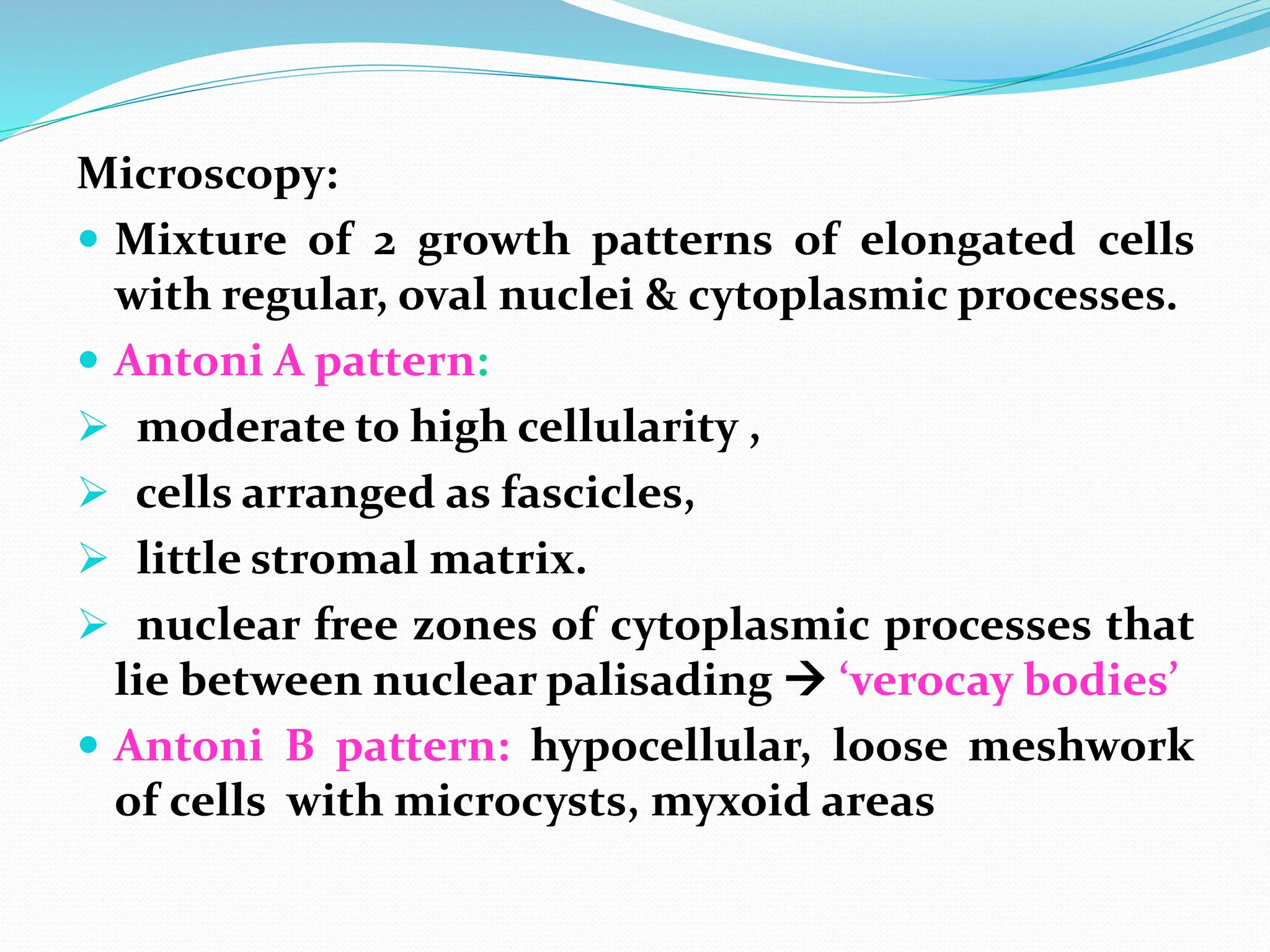
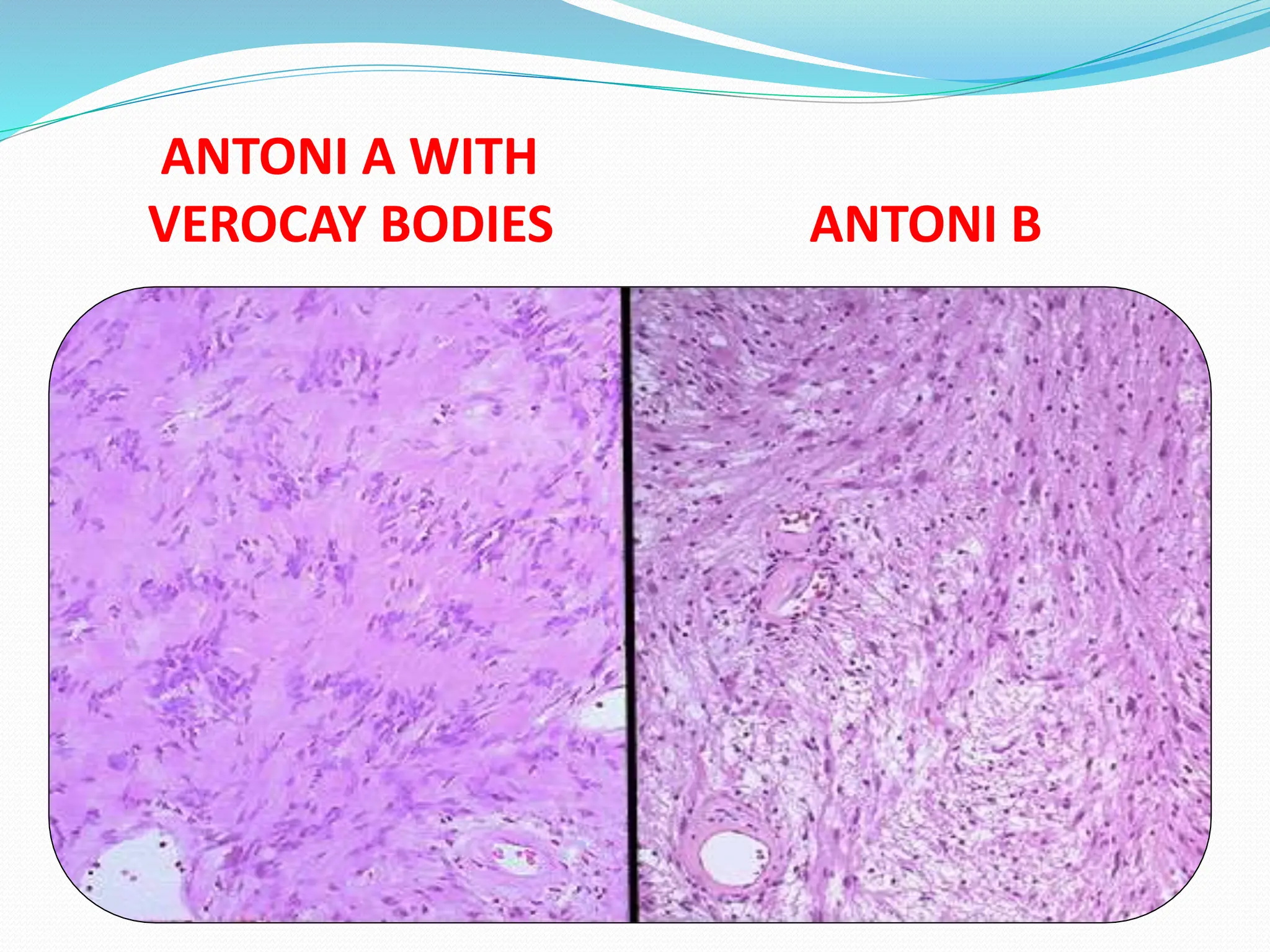
The document provides an overview of central nervous system infections and tumors, detailing types of infections such as meningitis and encephalitis, and their clinical features and diagnosis. It also explains various brain tumor types, including gliomas, neuronal tumors, meningiomas, and peripheral nerve sheath tumors, with a focus on their characteristics, symptoms, and genetic aspects. Additionally, it discusses familial tumor syndromes like neurofibromatosis and tuberous sclerosis, summarizing their clinical implications.