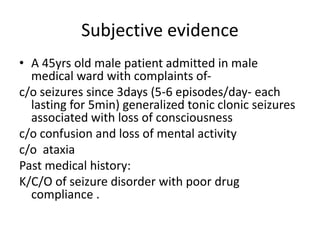
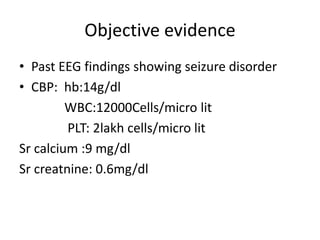
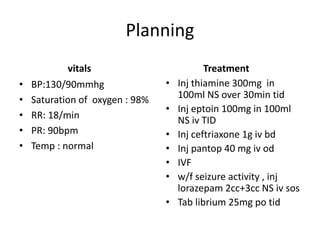
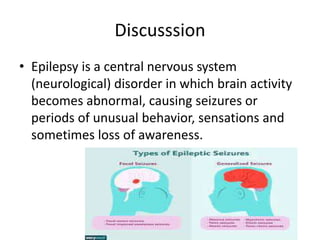
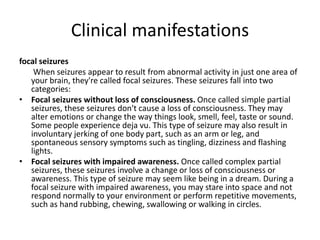
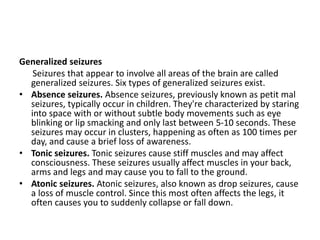
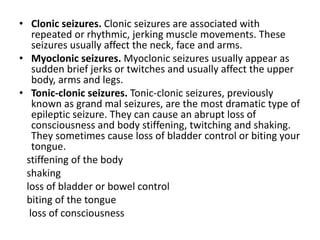
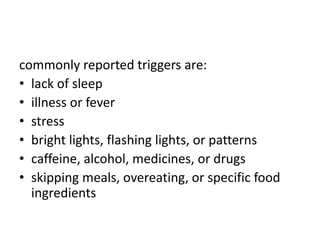
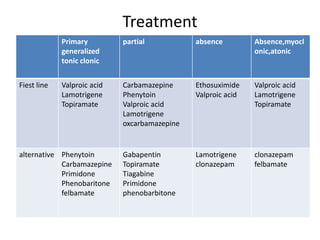
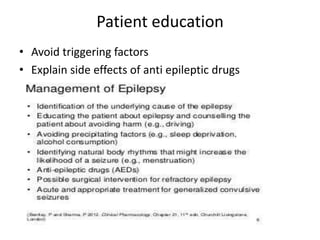
A 45-year-old male was admitted to the hospital with a history of seizures. He reported having 5-6 generalized tonic-clonic seizures per day for the past 3 days with loss of consciousness. His past medical history included epilepsy with poor drug compliance. On examination, his vitals were stable. Laboratory tests showed abnormal calcium and creatinine levels. He was diagnosed with epilepsy and started on intravenous anti-seizure medications, vitamins, and antibiotics to treat any underlying infection. The patient was educated on avoiding seizure triggers and the side effects of his medication regimen.