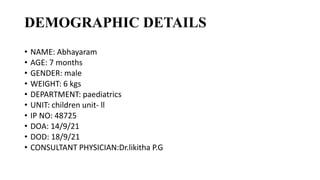
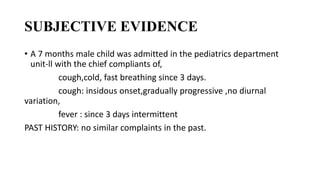
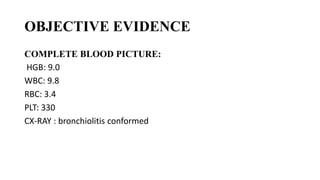
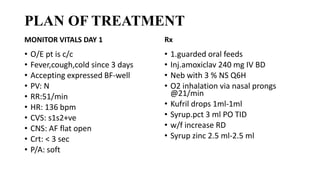
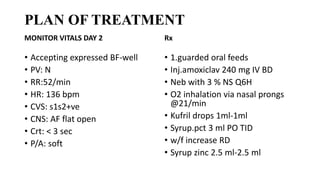
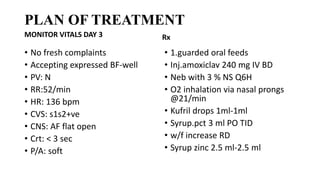
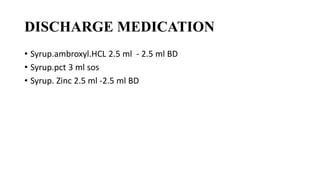
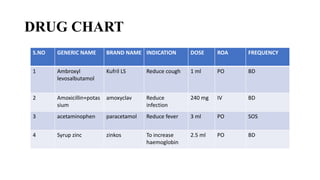
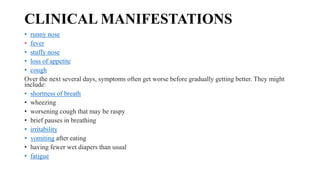
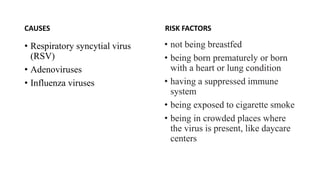
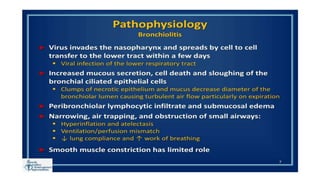
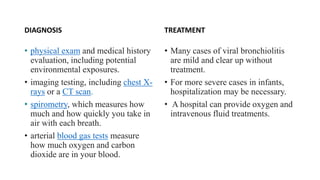
A 7 month old male child presented with cough, cold and fast breathing for 3 days. Examination and investigations confirmed acute bronchiolitis. He was treated with amoxicillin, nebulization, oxygen and supportive medications. His symptoms improved over 3 days and he was discharged on medications including levosalbutamol and zinc supplements. Bronchiolitis is a common viral infection in infants caused mainly by RSV that leads to airway inflammation and obstruction.