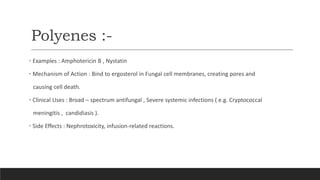
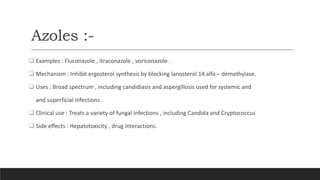
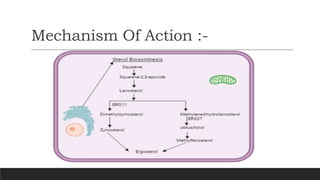
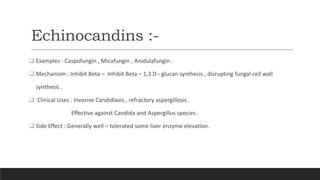
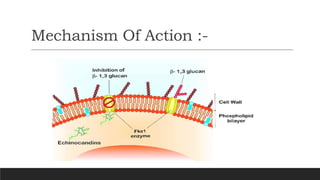
The document provides an overview of antifungal agents, including their classification, mechanisms of action, resistance mechanisms, clinical considerations, side effects, and recent advances in treatment. It highlights the importance of antifungals in managing fungal infections, particularly in immunocompromised patients, and presents a case study illustrating the successful use of fluconazole for treating invasive pulmonary aspergillosis. The document emphasizes the necessity for individualized treatment plans and vigilant monitoring to ensure patient safety and therapeutic effectiveness.


![References :-
Science Direct References :
Debra J. Lugo, William J. Steinbach, in Principles and Practice of Pediatric Infectious Diseases (Sixth
Edition), 2023
William J. Steinbach, Christopher C. Dvorak, in Principles and Practice of Pediatric Infectious Disease (Third
Edition), 2008
Shmuel Shoham, ... Thomas J Walsh, in Infectious Diseases (Third Edition), 2010 .
Casadevall A, Scharff MD. Return to the past: The case for antibody-based therapies in infectious diseases. Clin Infect
Dis. 1995;21:150–61. [PMC free article] [PubMed]
Como JA, Dismukes WE. Oral azole drugs as systemic antifungal therapy. New Engl J Med. 1994;330:263–
272. [PubMed]](https://image.slidesharecdn.com/advancephamacology-240601162712-72e3df3d/85/Brief-insight-on-antifungal-agents-with-case-study-28-320.jpg)
