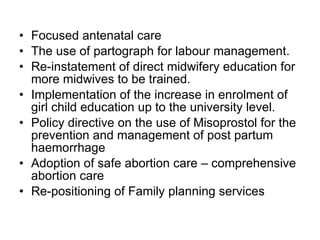
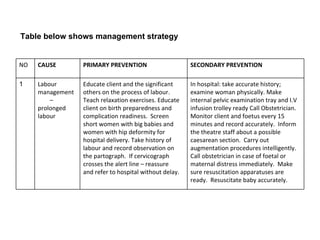
The document discusses the role of midwives and public health nurses in reducing maternal, newborn and child mortality in Ghana. It provides background on Ghana and defines key terms like maternal mortality rate. It describes the causes of maternal deaths as the three delays - delays in seeking care, reaching care, and receiving adequate care. The document outlines Ghana's policies and efforts to improve maternal health, including the Millennium Development Goals. It discusses the midwife's role in antenatal care, labor/delivery care, and postpartum care. Strategies have been implemented before and after 2000 to strengthen the midwife's role in reducing mortality.