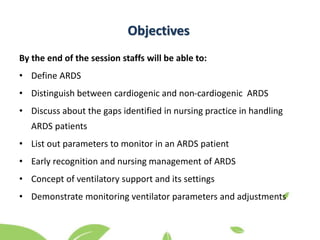
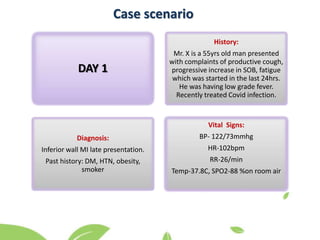
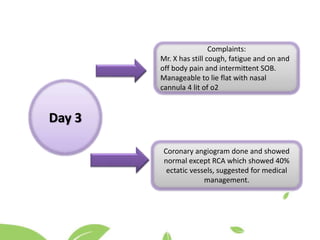
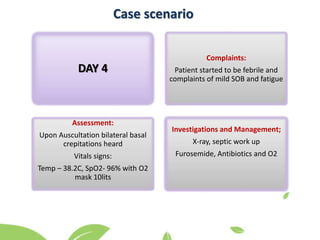
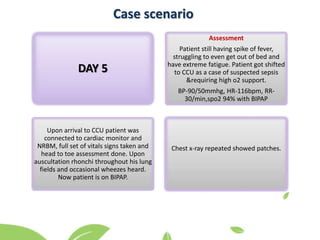
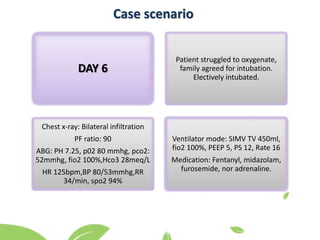
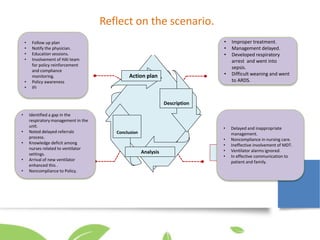
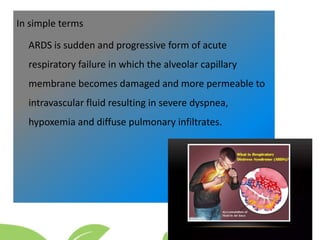
The document provides information on a reflective learning session for nursing staff on acute respiratory distress syndrome (ARDS). It includes case scenarios of a patient's progression to ARDS over 6 days. Objectives are defined to help staff understand ARDS, differentiate it from other causes, discuss gaps in nursing practice, and demonstrate monitoring ventilator parameters. A discussion is prompted on the case, and an action plan is proposed to notify managers, ensure compliance, involve multidisciplinary teams early, provide training on ventilators, and conduct an immediate feedback interview.


![References
• Adeani,I.Febriani,R. (2020).Using GIBBS Reflective cycle in making reflections of literature analysis. Research gate.
Volume6(2):139-148. Available from:
https://www.researchgate.net/publication/343599316_Using_GIBBS'_reflective_cycle_in_making_reflections_of_literary_an
alysis. [Accessed On 17 December 2022].
• Heart Hospital nursing educators and experienced colleagues in CCU.
• Ajibowo, A . Kolawole, O. Sadia, H.Amedu,O.Chaudary,H.Hussaini,H.Hambolu,E.Khan,T.Kauser,H.Khan,A. ( 2022) A
Comprehensive Review of the Management of Acute Respiratory Distress Syndrome. Cureus 14(10): e30669.Available from:
https://www.cureus.com/articles/105730-a-comprehensive-review-of-the-management-of-acute-respiratory-distress-
syndrome [Accessed On 19 December 2022].
• HMC Intranet Clinical guidelines. Prone Positioning in Severe Acute Respiratory Distress Syndrome (ARDS) in Intensive Care
Unit (ICU)CG1014.Available from:
https://itawasol.hamad.qa/EN/SiteSearch/Pages/results.aspx?k=PRONING#k=PRONE:~:text=https%3A//itawasol.hamad.qa/K
nowledgeCenterDocuments/Clinical%20Guidelines/Hamad%20General%20Hospital/CG%2010146%20Prone%20Positioning%
20in%20Severe%20Acute%20Respiratory%20Distress%20Syndrome%20(ARDS)%20in%20Intensive%20Care%20Unit%20(ICU).
pdf [Accessed On 18 December 2022].
• HMC Intranet Clinical Policy. Care Of mechanically Ventilated Patients. CL6011.Available from:
https://itawasol.hamad.qa/EN/How%20We%20Work/HMC-Policies/CP/Manuals/Pages/Clinical-Policy-Manual-(CL).aspx
[Accessed On 18 December 2022].](https://image.slidesharecdn.com/ardsfinalppt-230409190112-554b4bbb/85/ARDS-final-PPT-pptx-29-320.jpg)
