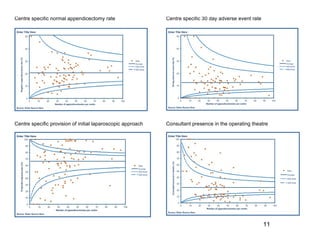
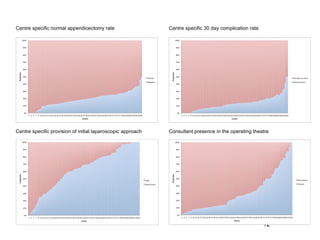
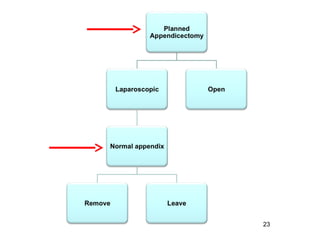
The document summarizes a national multicenter audit of appendicectomy procedures conducted in the United Kingdom. Over 3,300 appendicectomy cases were collected from 95 centers. Key findings included an initial laparoscopic approach rate of 66.3% and a histologically normal appendix rate of 20.6%. The audit demonstrated the feasibility of a large multicenter collaborative research network. Future randomized controlled trials are proposed, including comparing laparoscopic versus open appendicectomy and evaluating the treatment of appendicitis with antibiotics versus an operative approach.