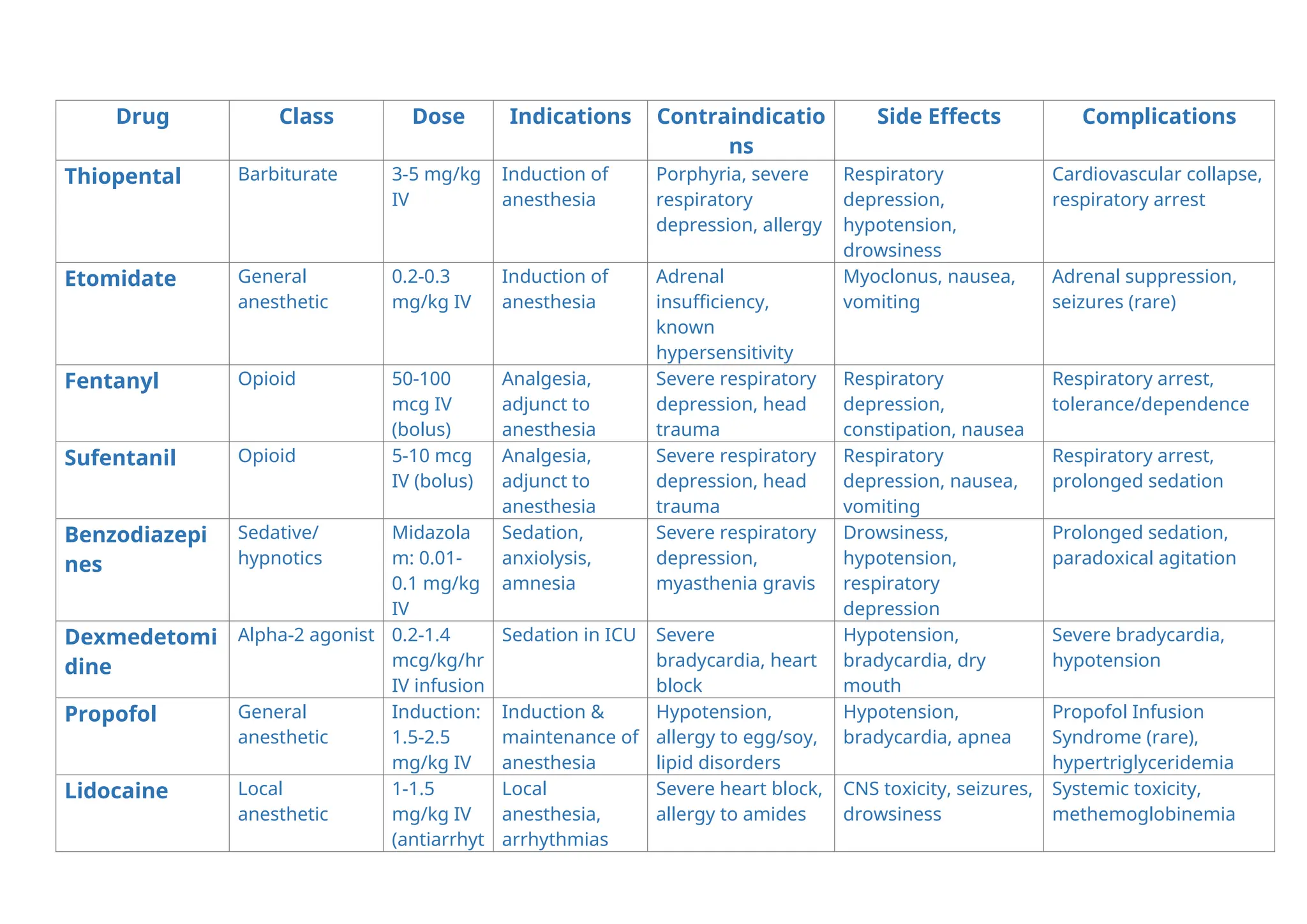
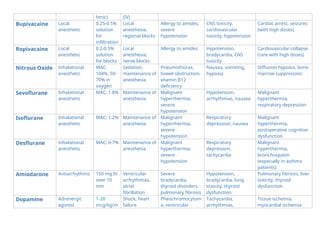
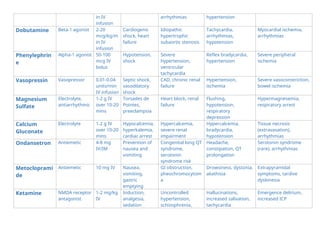
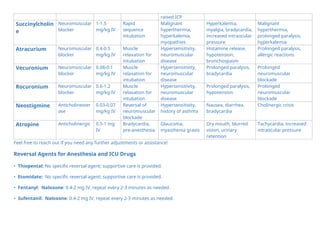
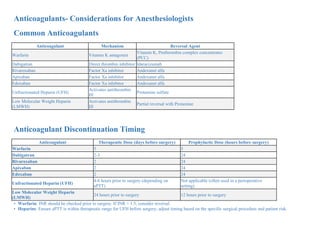
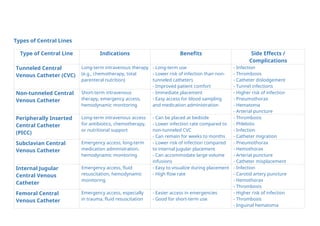
The document provides a comprehensive overview of various anesthetic and emergency medications, detailing their drug class, dosage, indications, contraindications, side effects, and complications. It also includes guidelines for the reversal of these agents and considerations for managing anticoagulants in perioperative settings, emphasizing the importance of monitoring and patient safety. Additionally, it outlines the types of central lines used for intravenous therapy, explaining their indications, benefits, and potential complications.