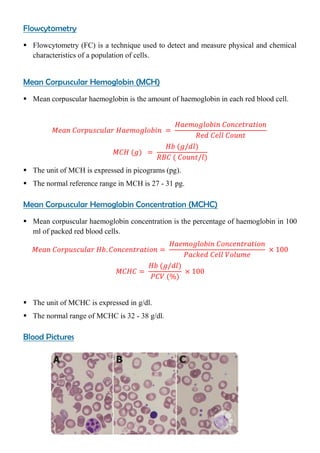
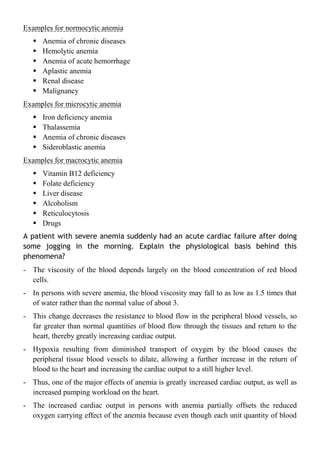
The document provides a comprehensive overview of anemia, including its definition, types, causes, symptoms, and classifications. It discusses different gradings of anemia according to hemoglobin levels and explains various forms such as blood loss anemia, impaired production, and hemolytic anemia, along with their underlying mechanisms. Additionally, it covers the signs, oral manifestations, and diagnostic investigations for anemia, emphasizing its significance in medical practice.