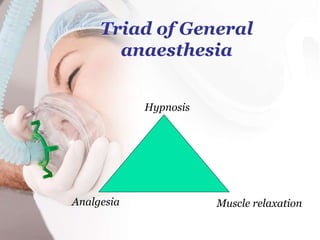
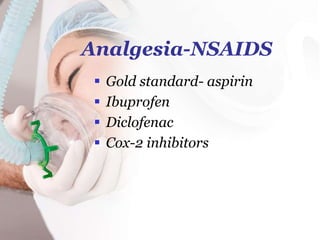
The document discusses the history and types of anesthesia, including how general anesthesia was not used until the 1800s when ether and chloroform were discovered, and describes the different types of anesthesia like general, regional, and local anesthesia as well as the phases of general anesthesia from induction to recovery. It also covers the advantages and disadvantages of different anesthesia methods and considerations for choosing the right type of anesthesia for a patient's procedure and condition.