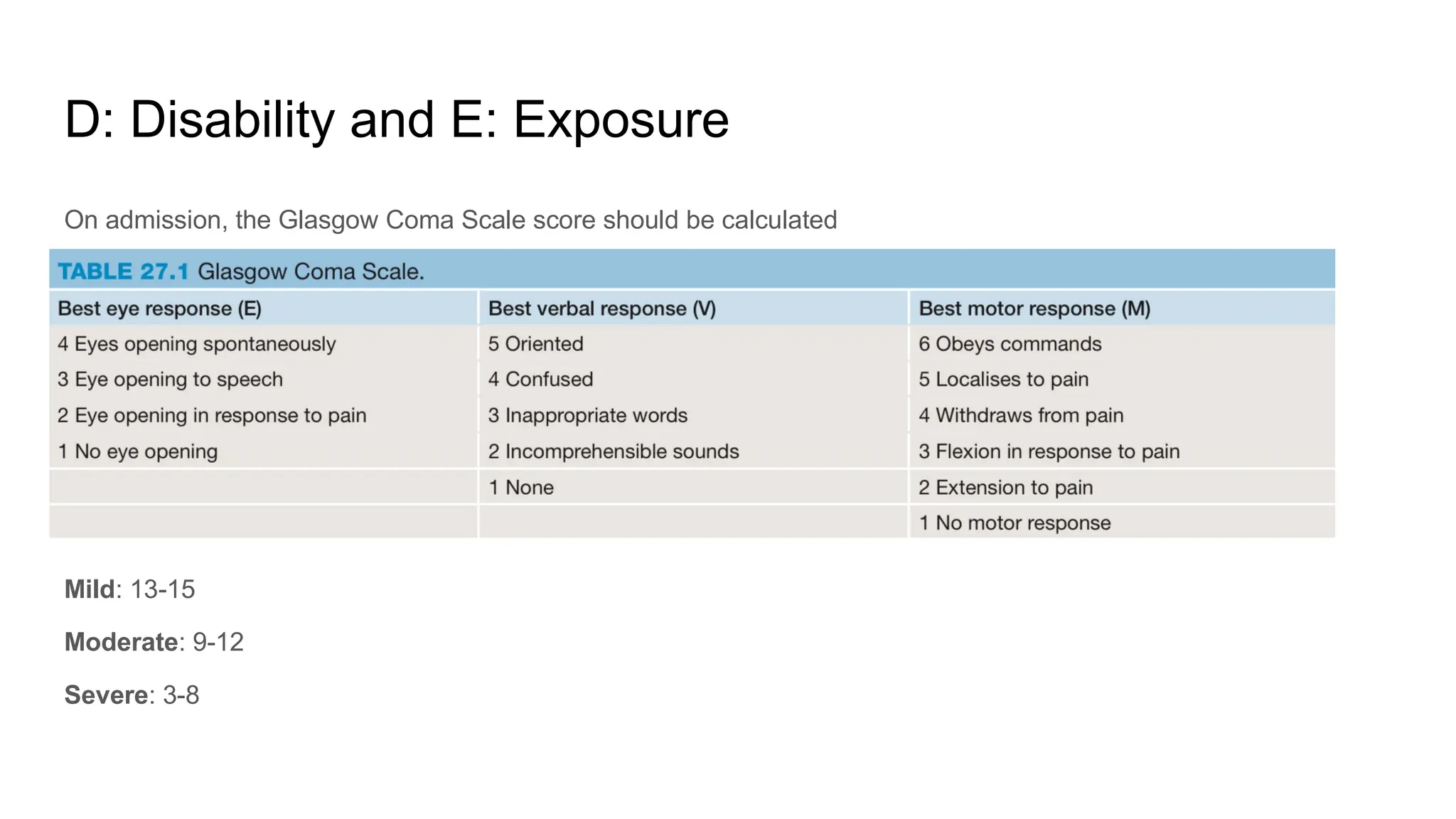
The document outlines the Advanced Trauma Life Support (ATLS) protocols for assessing and managing severely injured patients, emphasizing early identification and coordination with trauma teams. It details the primary and secondary survey processes, stressing the critical steps in airway management, hemorrhage control, and maintaining hemodynamic stability. It also highlights the importance of thorough examinations and temperature regulation during patient care.