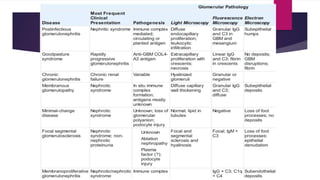
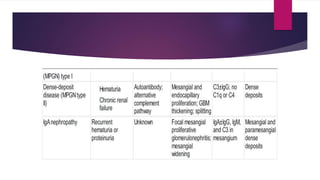
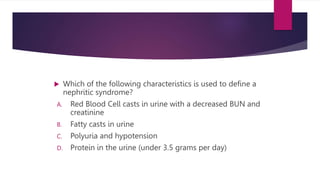
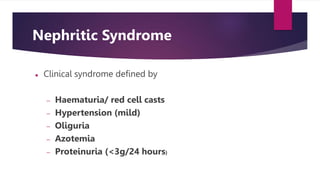
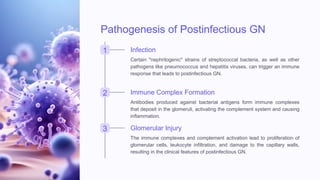
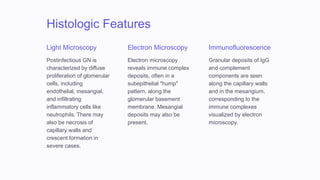
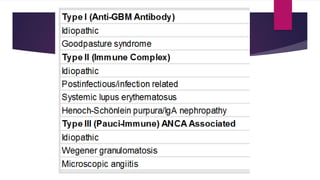
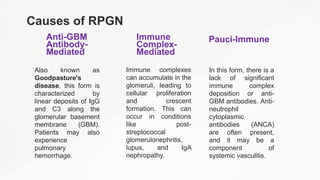
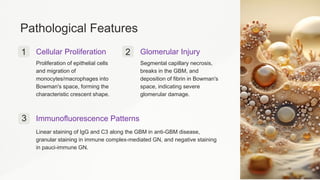
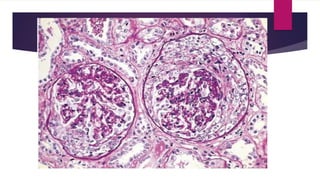
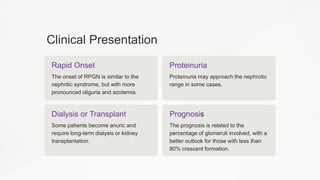
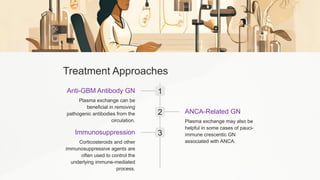
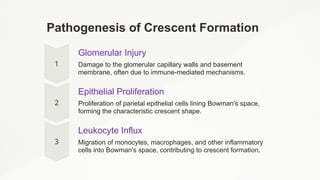
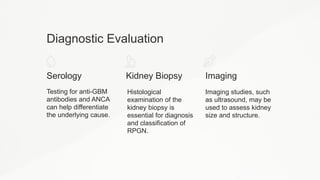
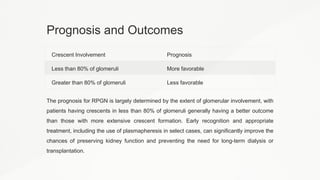
The document discusses various glomerular diseases, focusing on nephritic syndrome and rapidly progressive glomerulonephritis (RPGN). It outlines the pathogenesis, clinical presentation, diagnostic evaluation, and treatment options for conditions like postinfectious glomerulonephritis and RPGN, emphasizing the importance of understanding these syndromes for effective management. Additionally, it highlights the need for ongoing research into their underlying mechanisms and potential novel therapies.