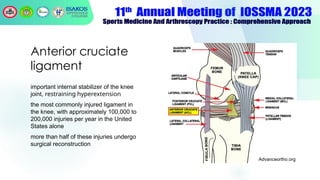
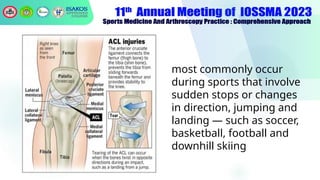
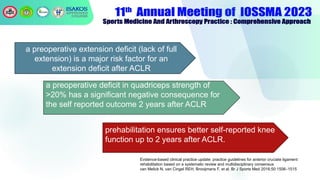
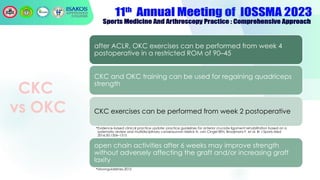
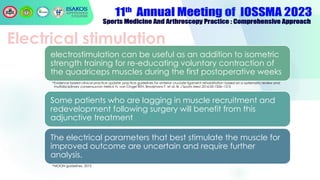
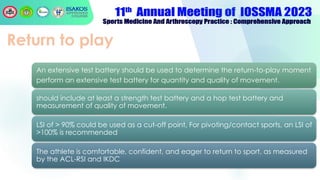
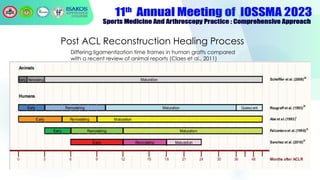
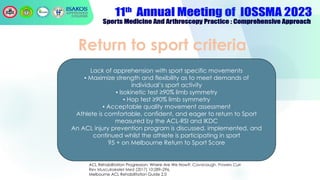
The document outlines the principles and protocols for anterior cruciate ligament (ACL) injury rehabilitation, emphasizing the significance of a structured rehabilitation program for successful recovery. Key elements include prehabilitation, immediate weight-bearing post-surgery, range of motion goals, neuromuscular training, and a detailed progression through phases towards returning to sports. It highlights the importance of tailored rehabilitation protocols based on individual readiness and specific criteria while also discussing injury prevention strategies.