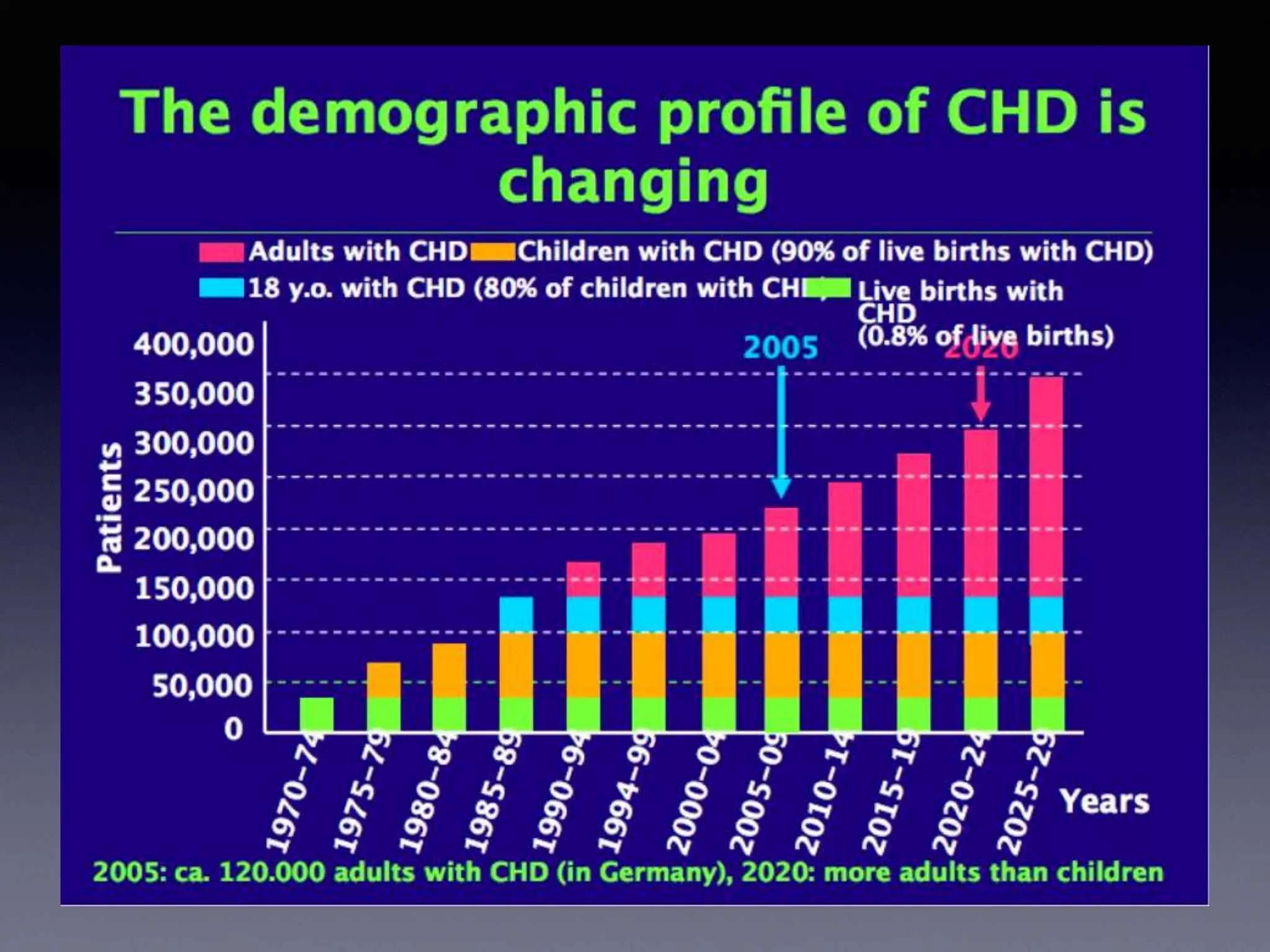
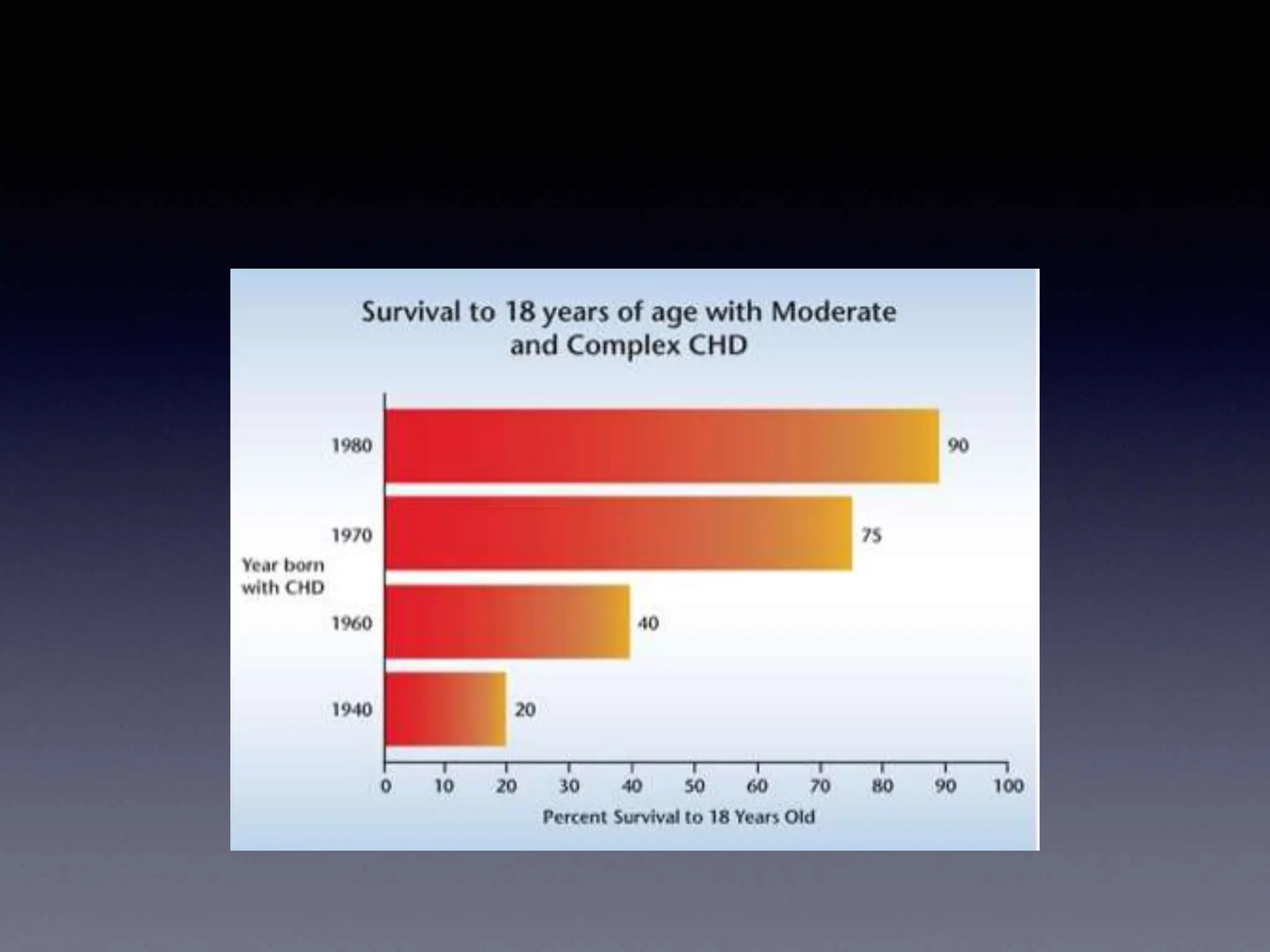
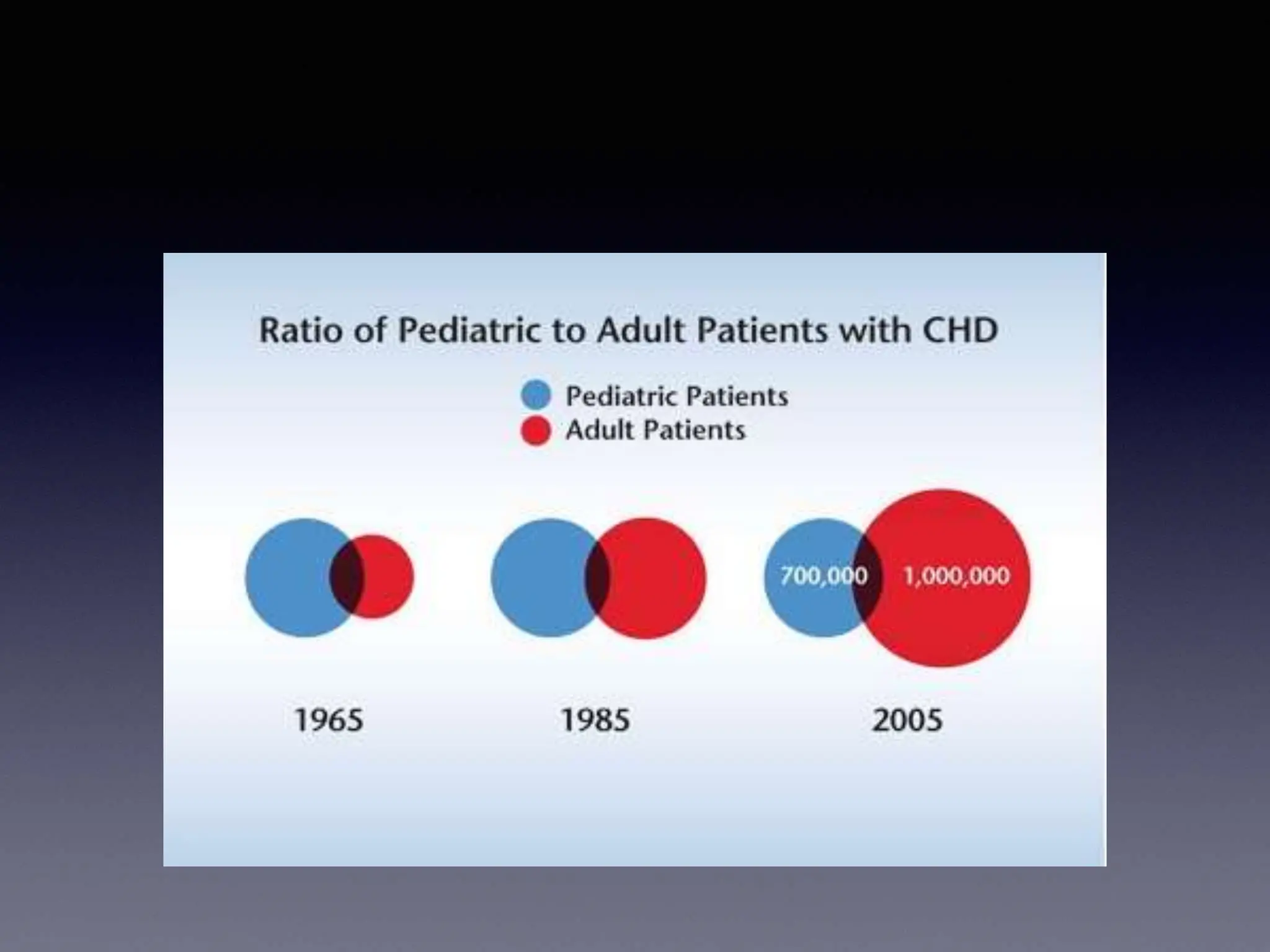
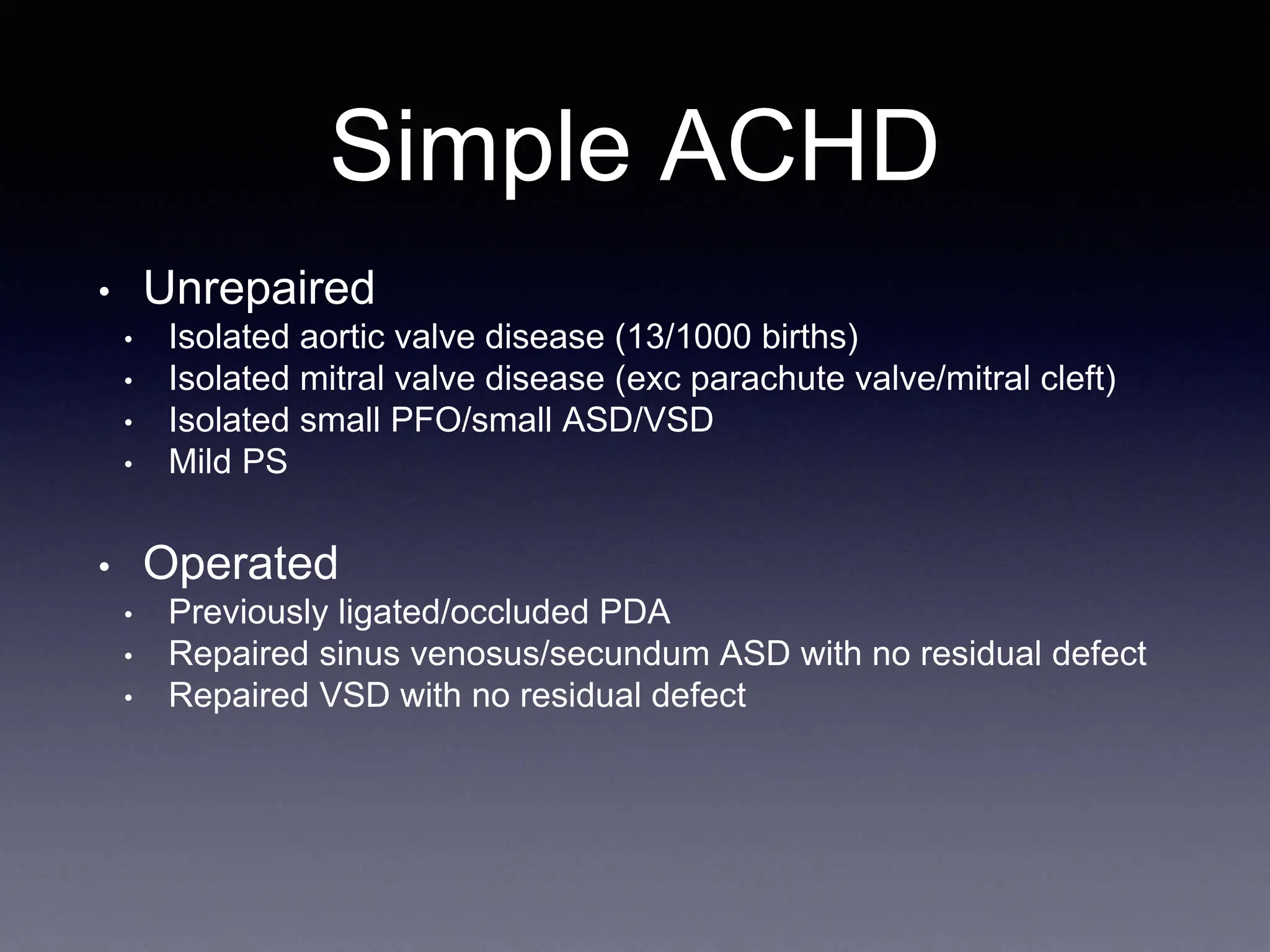
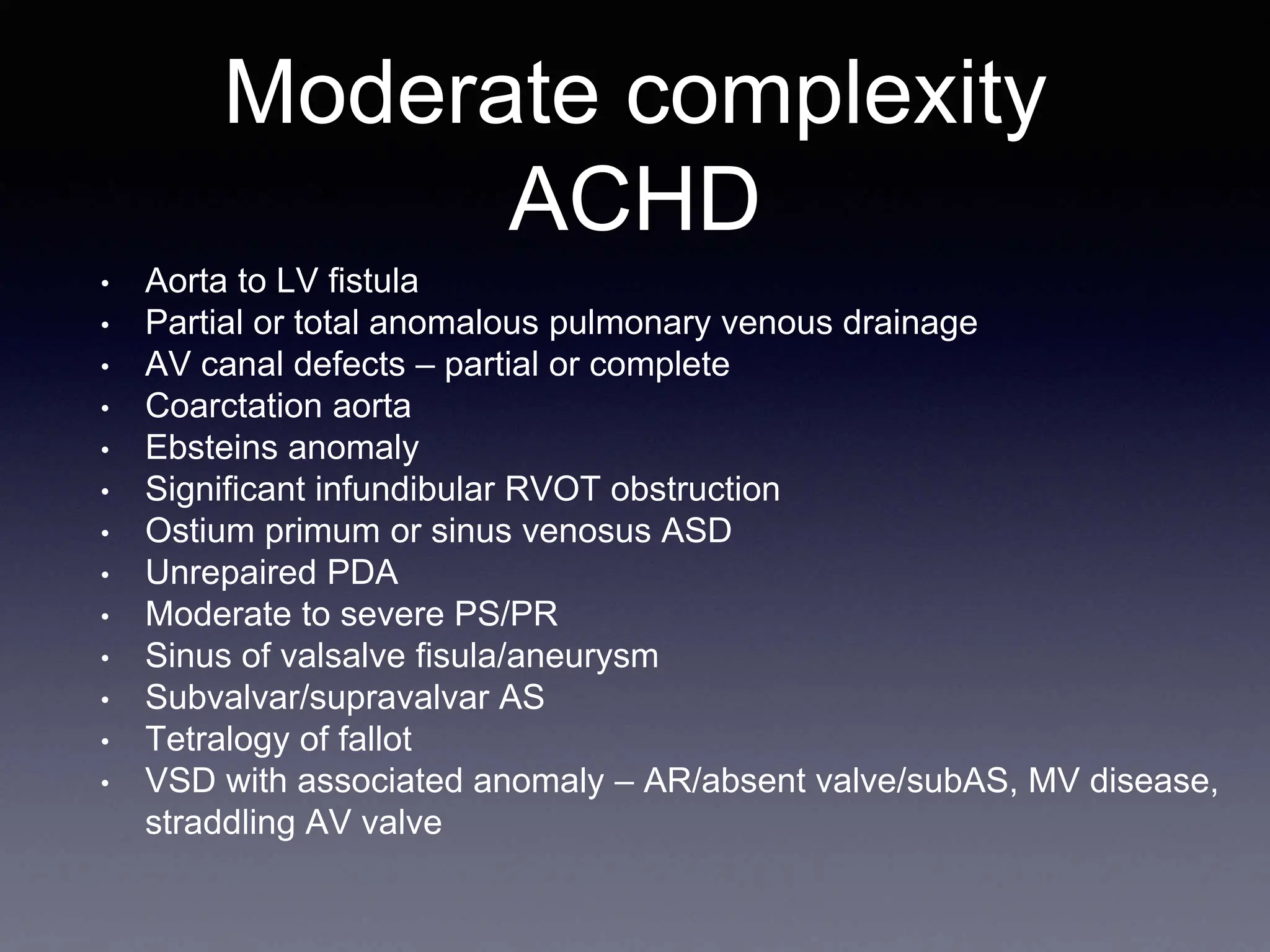
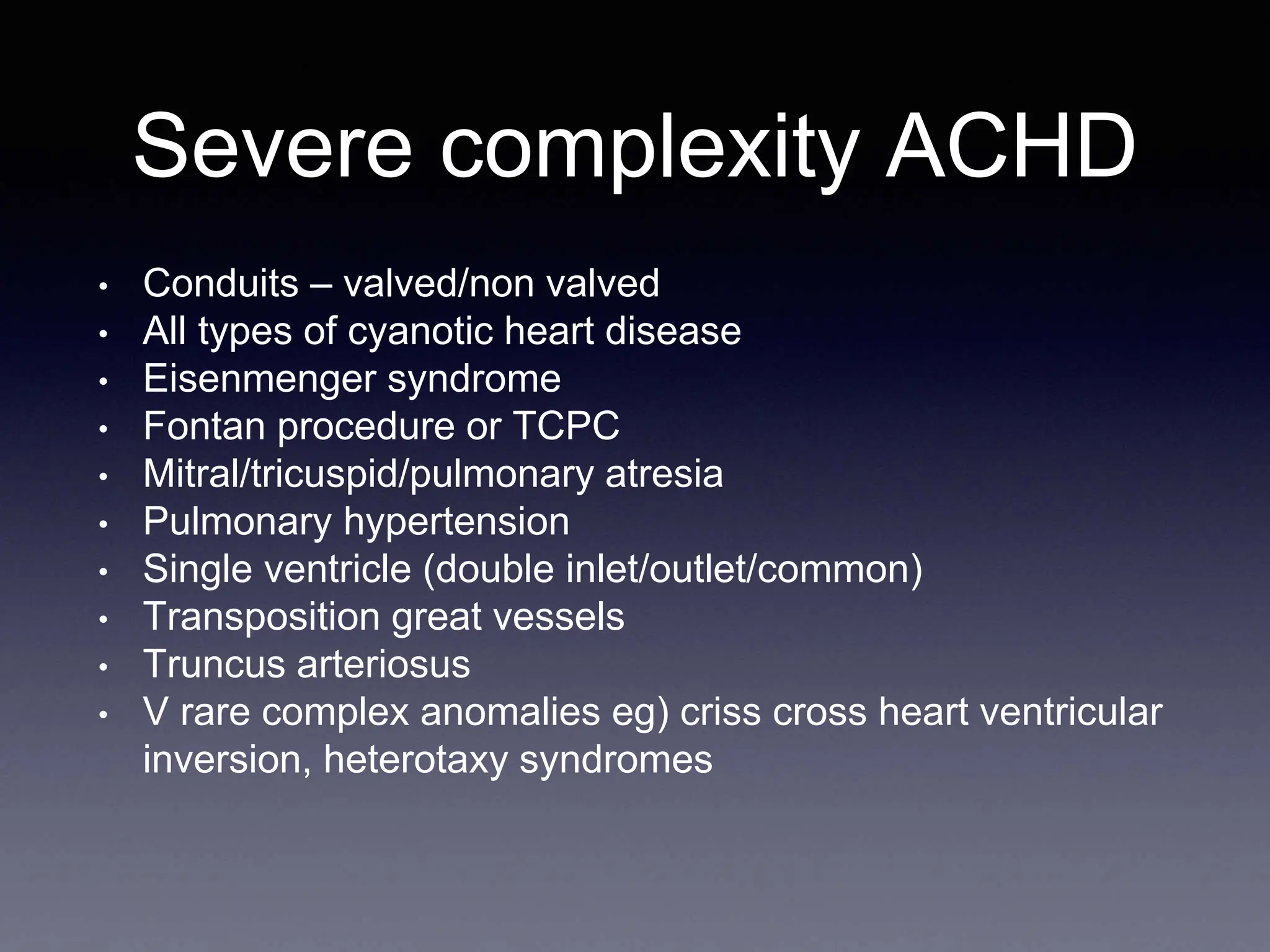
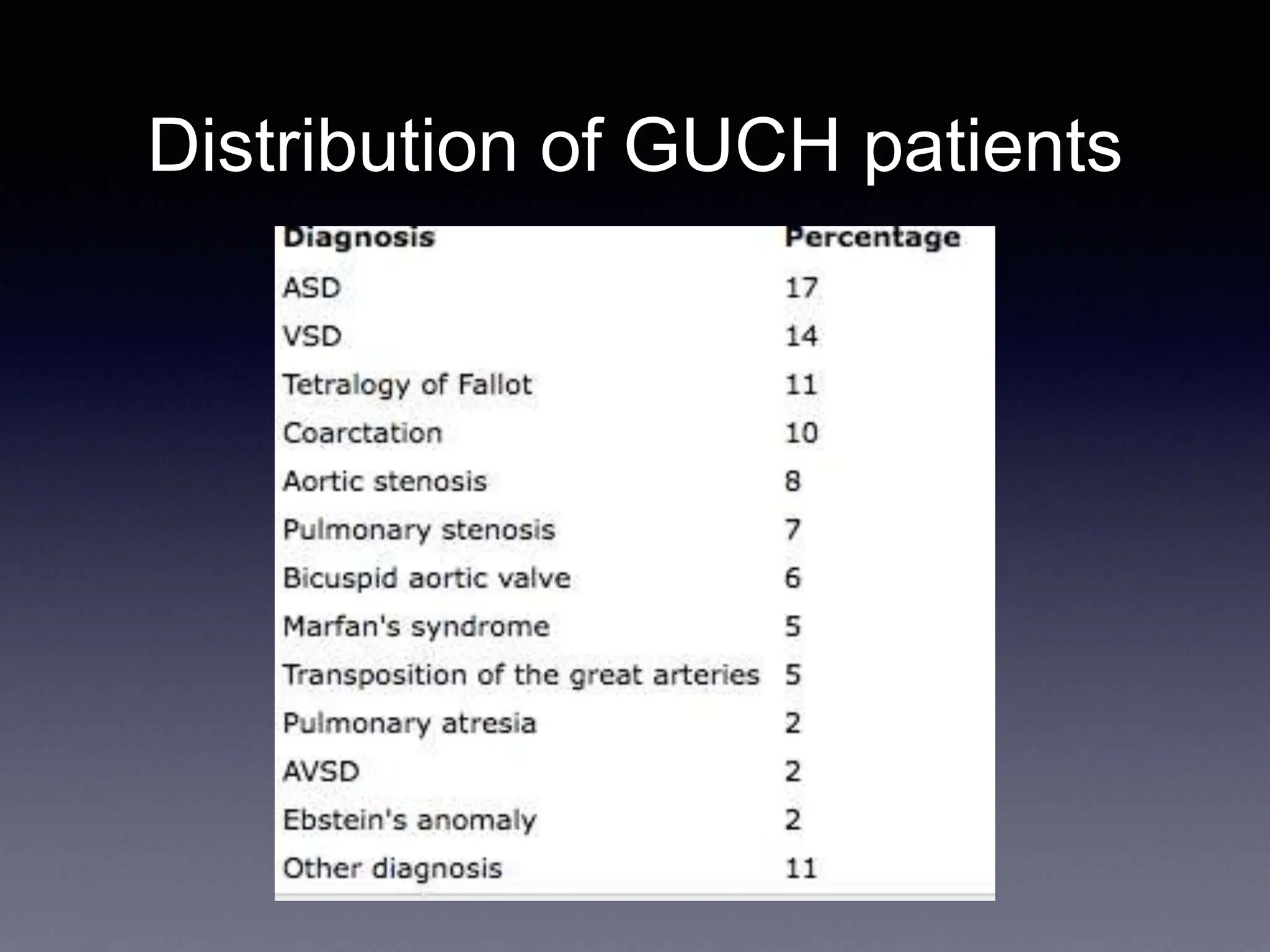
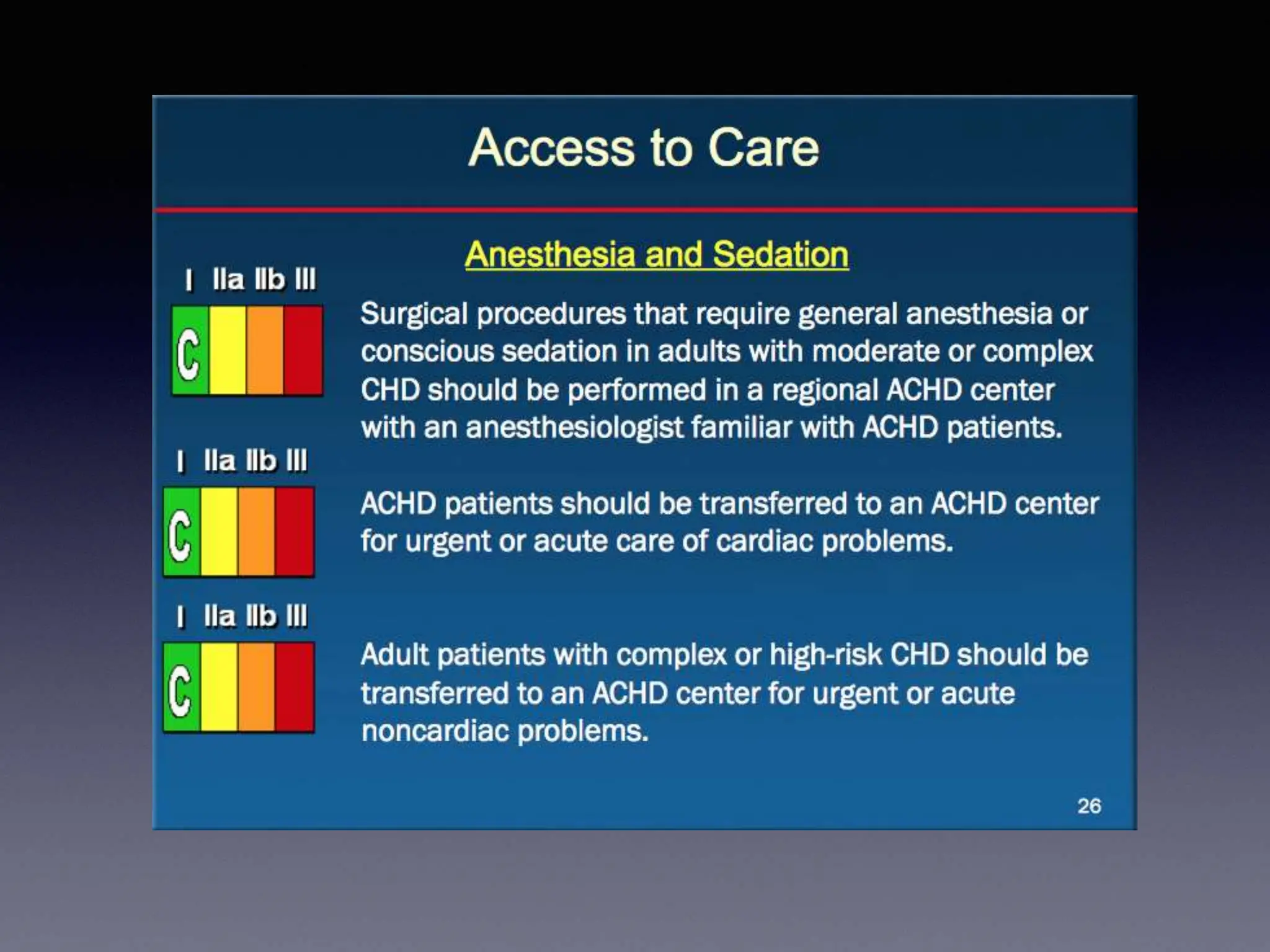
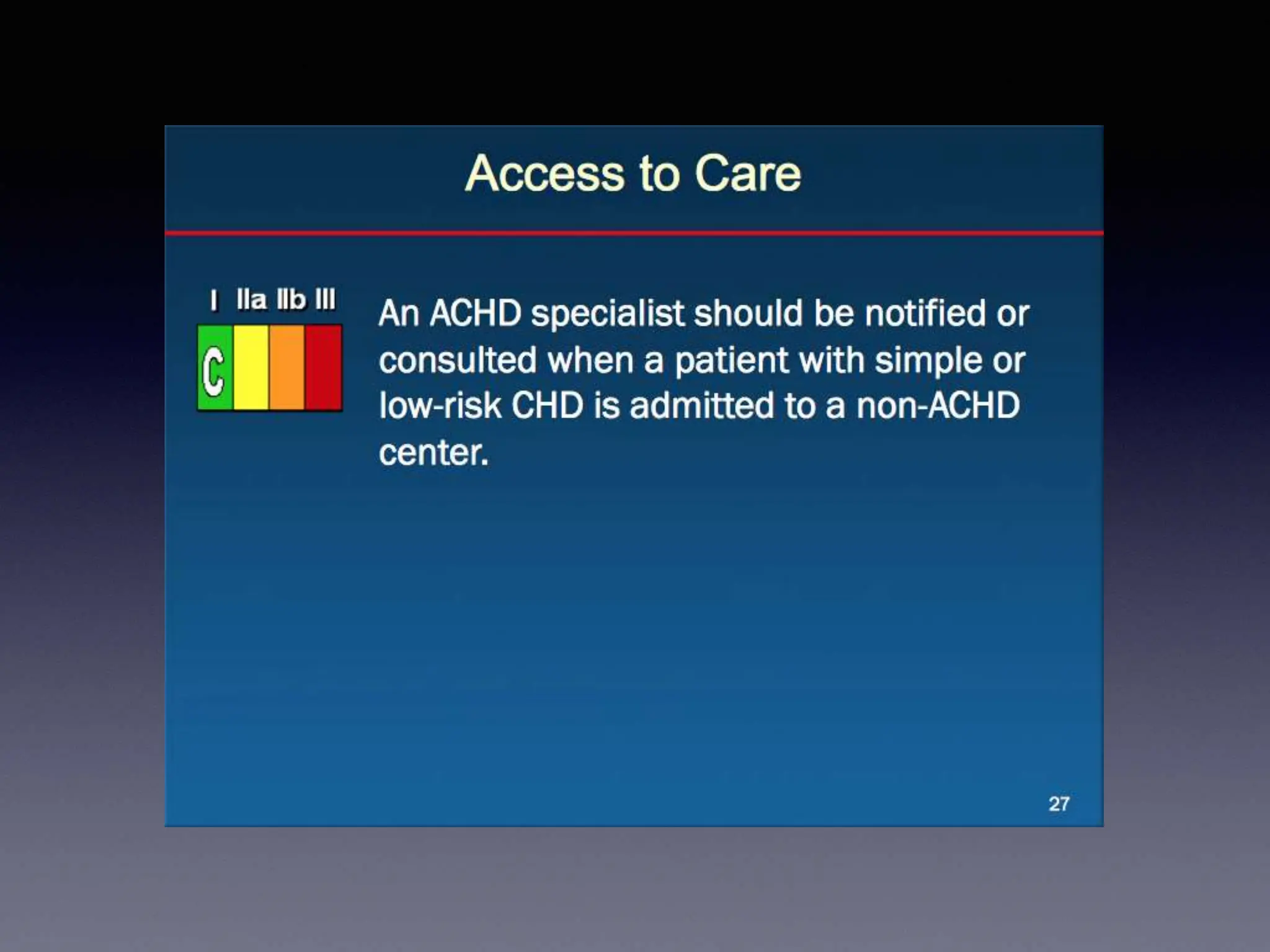
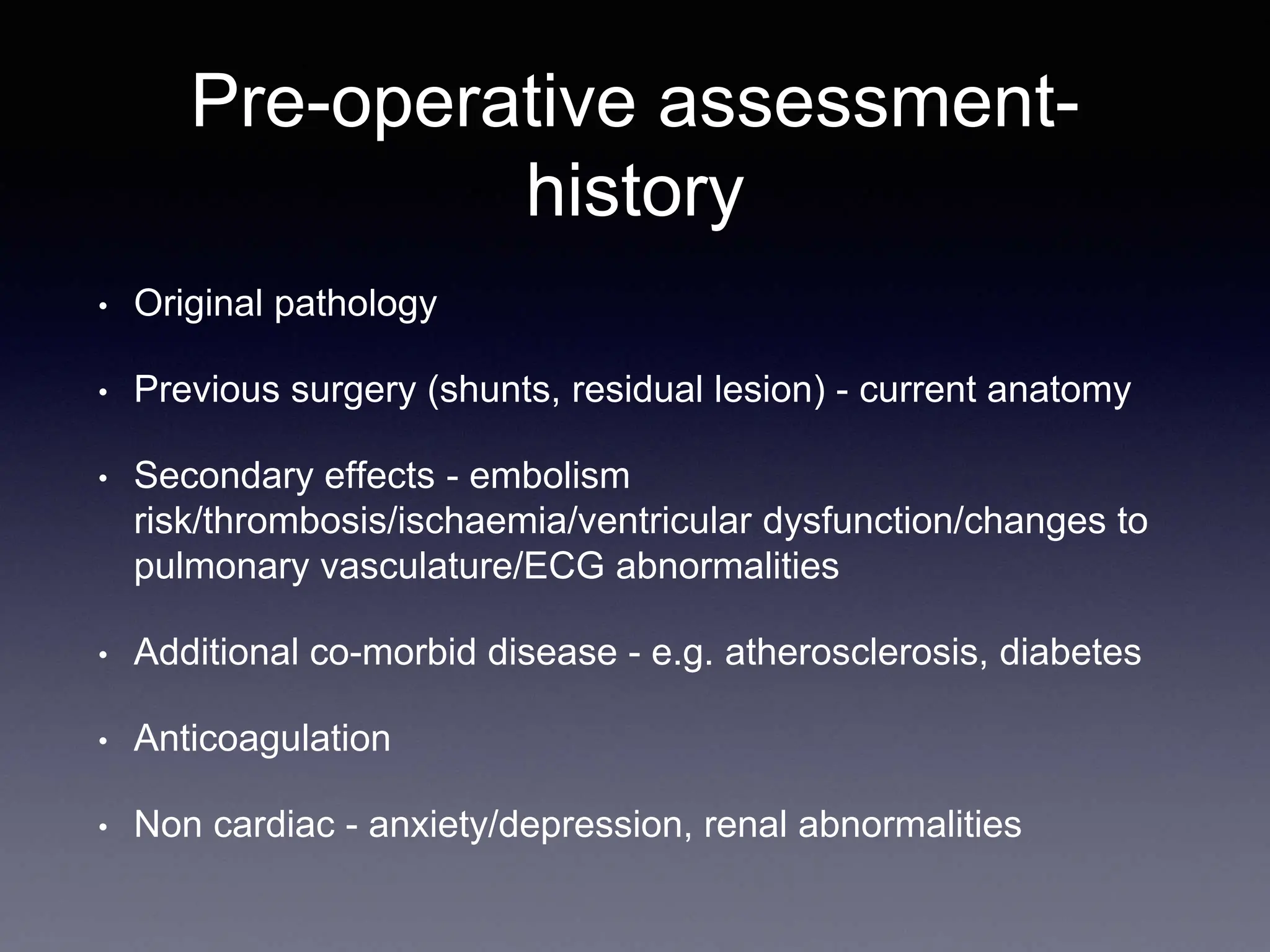
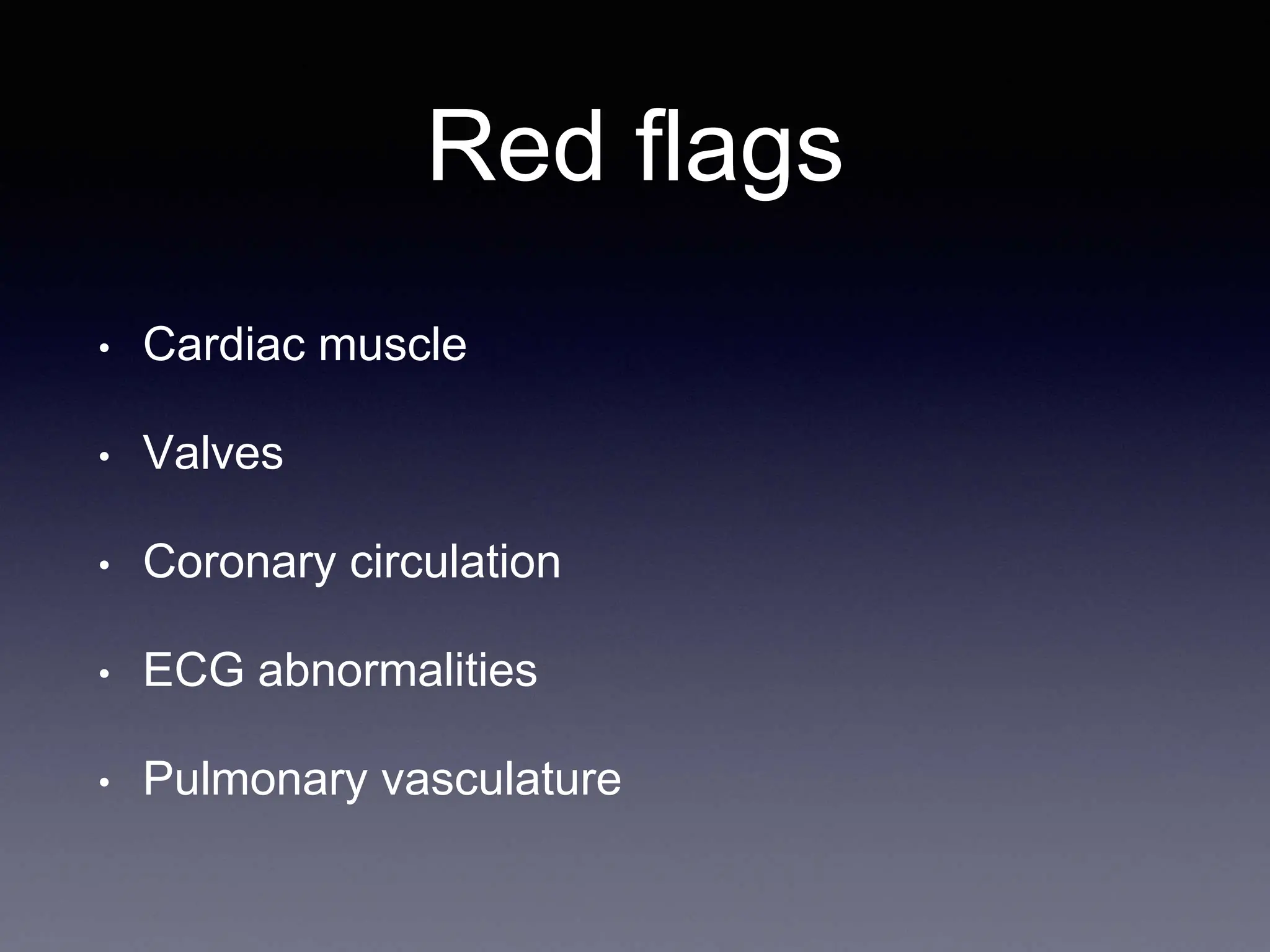
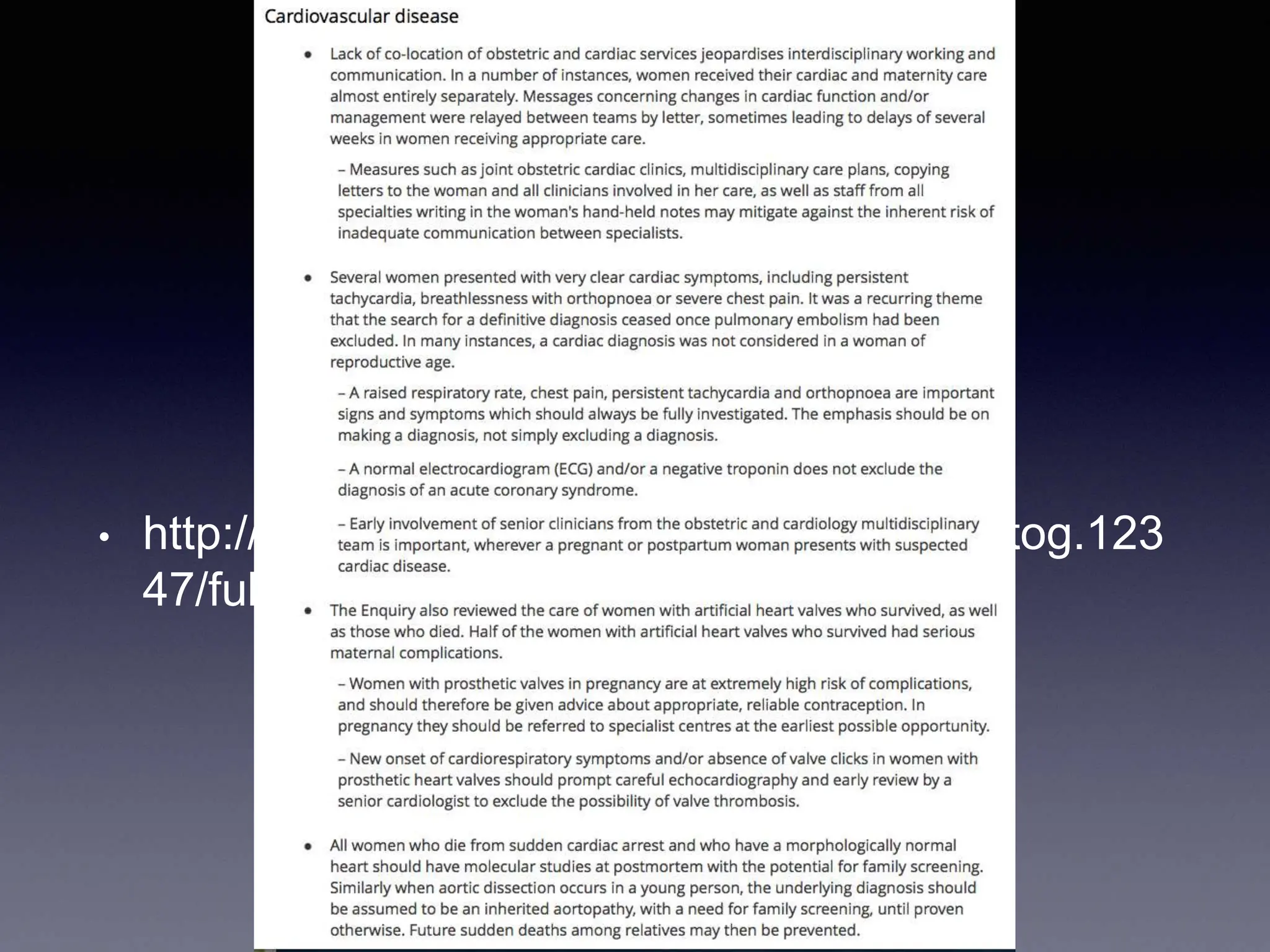
This document outlines key points regarding anaesthesia management for adult congenital heart disease (ACHD), emphasizing the need for awareness of the growing population and acute presentation frameworks. It highlights different complexities of ACHD, pre-operative assessments, and considerations for anaesthetic practices, including drug choice and patient history. Additionally, it discusses pregnancy management for ACHD patients, focusing on risks and the importance of expert consultation.