د حاتم_البيطار دبلومة مكافحة العدوي 01005684344.pdfد حاتم_البيطار دبلومة مكافحة العدوي 01005684344.pdfد حاتم_البيطار دبلومة مكافحة العدوي 01005684344.pdfد حاتم_البيطار دبلومة مكافحة العدوي 01005684344.pdfد حاتم_البيطار دبلومة مكافحة العدوي 01005684344.pdfد حاتم_البيطار دبلومة مكافحة العدوي 01005684344.pdfد حاتم_البيطار دبلومة مكافحة العدوي 01005684344.pdfد حاتم_البيطار دبلومة مكافحة العدوي 01005684344.pdfد حاتم_البيطار دبلومة مكافحة العدوي 01005684344.pdfد حاتم_البيطار دبلومة مكافحة العدوي 01005684344.pdfد حاتم_البيطار دبلومة مكافحة العدوي 01005684344.pdfد حاتم_البيطار دبلومة مكافحة العدوي 01005684344.pdfد حاتم_البيطار دبلومة مكافحة العدوي 01005684344.pdfد حاتم_البيطار دبلومة مكافحة العدوي 01005684344.pdfد حاتم_البيطار دبلومة مكافحة العدوي 01005684344.pdfد حاتم_البيطار دبلومة مكافحة العدوي 01005684344.pdfد حاتم_البيطار دبلومة مكافحة العدوي 01005684344.pdfد حاتم_البيطار دبلومة مكافحة العدوي 01005684344.pdfد حاتم_البيطار دبلومة مكافحة العدوي 01005684344.pdfد حاتم_البيطار دبلومة مكافحة العدوي 01005684344.pdfد حاتم_البيطار دبلومة مكافحة العدوي 01005684344.pdfد حاتم_البيطار دبلومة مكافحة العدوي 01005684344.pdfد حاتم_البيطار دبلومة مكافحة العدوي 01005684344.pdfد حاتم_البيطار دبلومة مكافحة العدوي 01005684344.pdfد حاتم_البيطار دبلومة مكافحة العدوي 01005684344.pdfد حاتم_البيطار دبلومة مكافحة العدوي 01005684344.pdfد حاتم_البيطار دبلومة مكافحة العدوي 01005684344.pdfد حاتم_البيطار دبلومة مكافحة العدوي 01005684344.pdfد حاتم_البيطار دبلومة مكافحة العدوي 01005684344.pdfد حاتم_البيطار دبلومة مكافحة العدوي 01005684344.pdfد حاتم_البيطار دبلومة مكافحة العدوي 01005684344.pdfد حاتم_البيطار دبلومة مكافحة العدوي 01005684344.pdfد حاتم_البيطار دبلومة مكافحة العدوي 01005684344.pdfد حاتم_البيطار دبلومة مكافحة العدوي 01005684344.pdfد حاتم_البيطار دبلومة مكافحة العدوي 01005684344.pdfد حاتم_البيطار دبلومة مكافحة العدوي 01005684344.pdfد حاتم_البيطار دبلومة مكافحة العدوي 01005684344.pdfد حاتم_البيطار دبلومة مكافحة العدوي 01005684344.pdfد حاتم_البيطار دبلومة مكافحة العدوي 01005684344.pdfد حاتم_البيطار دبلومة مكافحة العدوي 01005684344.pdfد حاتم_البيطار دبلومة مكافحة العدوي 01005684344.pdfد حاتم_البيطار دبلومة مكافحة العدوي 01005684344.pdfد حاتم_البيطار دبلومة مكافحة العدوي 01005684344.pdfد حاتم_البيطار دبلومة مكافحة العدوي 01005684344.pdfد حاتم_البيطار دبلومة مكافحة العدوي 01005684344.pdfد حاتم_البيطار دبلومة مكافحة العدوي 01005684344.pdfد حاتم_البيطار دبلومة مكافحة العدوي 01005684344.pdfد حاتم_البيطار دبلومة مكافحة العدوي 01005684344.pdfد حاتم_البيطار دبلومة مكافحة العدوي 01005684344.pdfد حاتم_البيطار دبلومة مكافحة العدوي 01005684344.pdfد حاتم_البيطار دبلومة مكافحة العدوي 01005684344.pdfد حاتم_البيطار دبلومة مكافحة العدوي 01005684344.pdfد حاتم_البيطار دبلومة مكافحة العدوي 01005684344.pdfد حاتم_البيطار دبلومة مكافحة العدوي 01005684344.pdfد حاتم_البيطار دبلومة مكافحة العدوي 01005684344.pdfد حاتم_البيطار دبلومة مكافحة العدوي 01005684344.pdfد حاتم_البيطار دبلومة مكافحة العدوي 01005684344.pdfد حاتم_البيطار دبلومة مكافحة العدوي 01005684344.pdfد حاتم_البيطار دبلومة مكافحة العدوي 010056



















































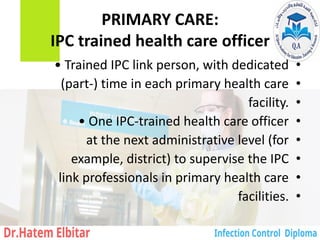
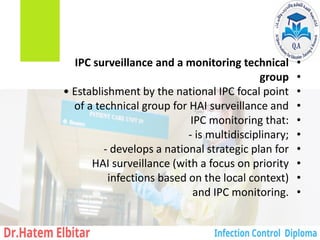
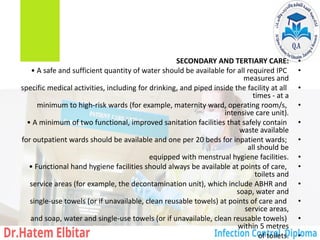
![SECONDARY CARE:
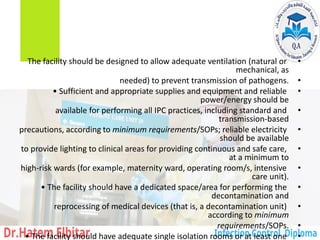
functional IPC programme
•
• Trained IPC focal point (one full-time trained
•
IPC Officer [nurse or doctor]) as per the
•
recommended ratio of 1:250 beds with
•
dedicated time to carry out IPC activities
•
in all facilities (for example, if the facility
•
has 120 beds, one 50% full-time equivalent
•
dedicated officer).
•
• Dedicated budget for IPC implementation](https://image.slidesharecdn.com/01005684344-250513002438-6e4f045c/85/_-01005684344-pdf-189-320.jpg)