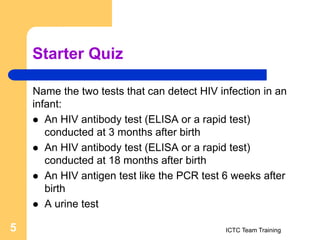
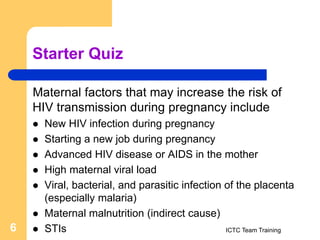
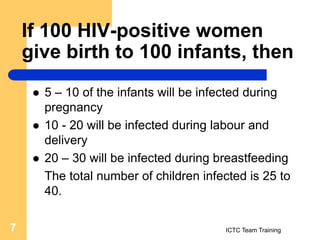
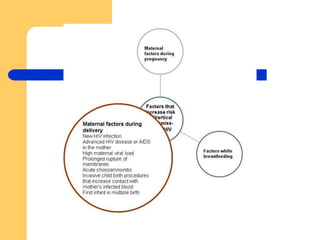
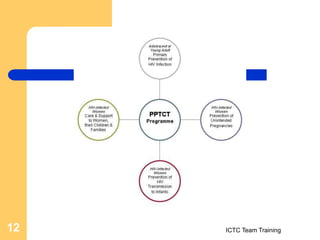
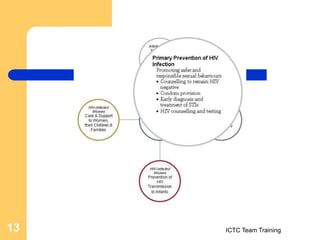
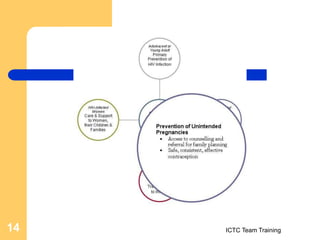
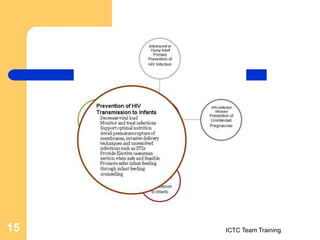
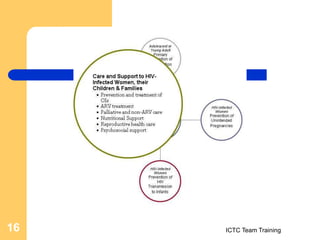
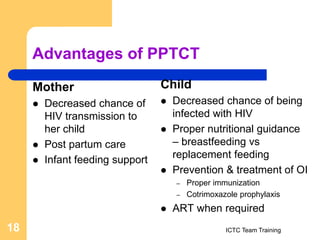
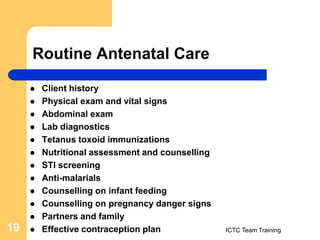
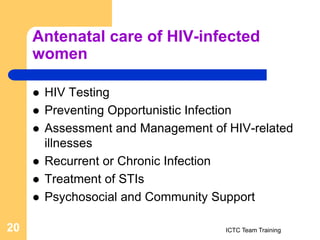
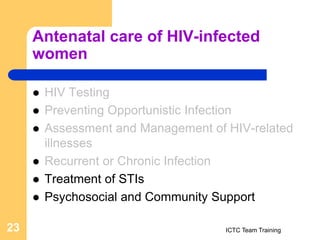
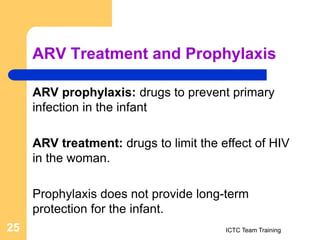
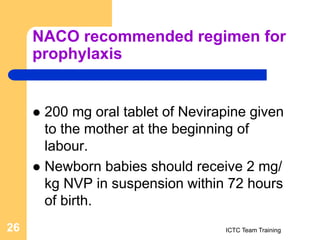
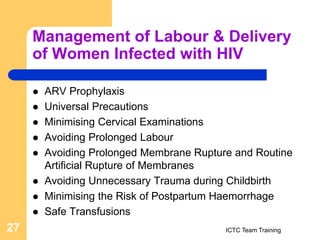
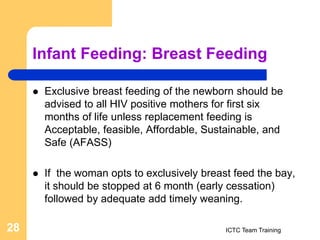
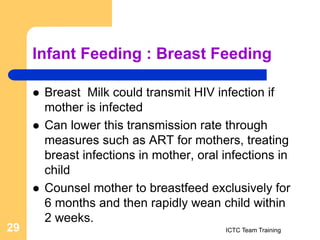
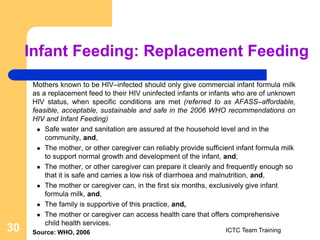
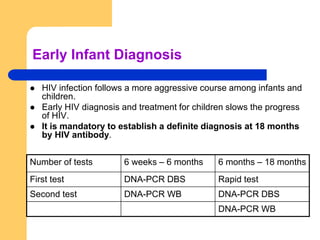
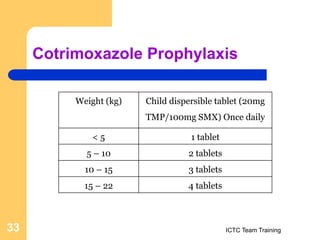
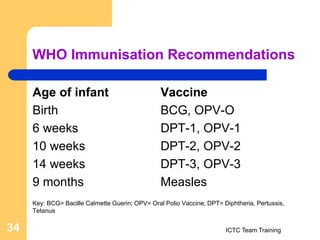
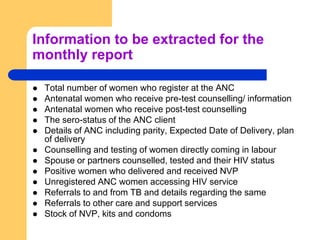
The document provides information on prevention of parent-to-child transmission (PPTCT) of HIV, including definitions of exclusive breastfeeding, reasons for choosing cup feeding over bottle feeding, factors influencing a woman's choice to breastfeed or use replacement feeding, tests for detecting HIV in infants, risk factors for mother-to-child transmission, and the number of children likely to be infected from an HIV-positive mother. It also summarizes guidelines for antenatal care of HIV-positive women, antiretroviral prophylaxis and treatment, management of labor and delivery, infant feeding options, early infant diagnosis, cotrimoxazole prophylaxis, immunizations and exposed infant care.