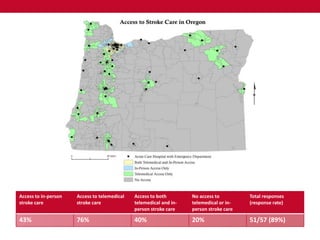
Telemedicine expanded access to stroke care in Oregon. A survey found 43% of respondents had access to in-person stroke care, 76% to telemedicine care, and 40% to both. Counties with high telemedicine access had lower uninsured rates and older adult populations compared to counties with low access. Telemedicine reduced the population without access to stroke care from 57% to 20%.