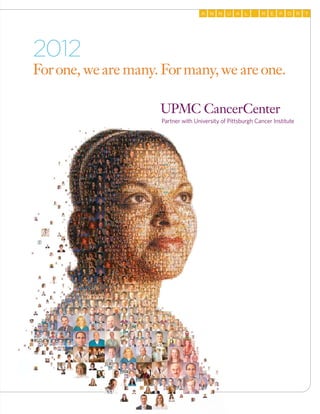
This document is the 2012 annual report for UPMC CancerCenter and University of Pittsburgh Cancer Institute. It highlights three key points:
1. UPMC CancerCenter brings together physicians, researchers, and staff from across the region to provide comprehensive cancer services through its large network of centers.
2. The report summarizes accomplishments in 2012, including new facilities like the Mario Lemieux Center for Blood Cancers, clinical trials, and international partnerships.
3. UPMC CancerCenter's leadership expresses pride in the organization's progress and anticipation for continued scientific advances that will improve cancer care and work towards eliminating the disease.