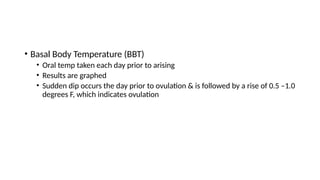
Infertility is defined as the inability to conceive after one year of unprotected intercourse, classified as primary or secondary infertility. Contributing factors include male factors, ovulation issues, tubal/uterine problems, and unexplained causes, with various treatments available like medications, hormonal therapy, and surgical options. Diagnostic assessments involve hormonal testing, imaging studies, and semen analysis to determine the underlying causes and guide treatment.