Antepartum haemorrhage i
•Download as PPTX, PDF•
78 likes•27,997 views
Antepartum haemorrhage -1
Report
Share
Report
Share
Recommended
More Related Content
What's hot
What's hot (20)
Similar to Antepartum haemorrhage i
Similar to Antepartum haemorrhage i (20)
Oligohydramnios by dr alka mukherjee dr apurva mukherjee nagpur m.s.

Oligohydramnios by dr alka mukherjee dr apurva mukherjee nagpur m.s.
BLEEDING DISORDERS IN LATE PREGNANCY-Renjini.R....pptx

BLEEDING DISORDERS IN LATE PREGNANCY-Renjini.R....pptx
More from obgymgmcri
More from obgymgmcri (20)
Recently uploaded
🍑👄Ludhiana Escorts Service☎️98157-77685🍑👄 Call Girl service in Ludhiana☎️Ludhiana Call Girls Service 🍑👄 Call Girls In Ludhiana Book Now :- 98157-77685
Our agency presents a selection of young, charming call girls available for bookings at Oyo Hotels. Experience high-class escort services at pocket-friendly rates, with our female escorts exuding both beauty and a delightful personality, ready to meet your desires. Whether it's Housewives, College girls, Russian girls, Muslim girls, or any other preference, we offer a diverse range of options to cater to your tastes.
We provide both in-call and out-call services for your convenience. Our in-call location in Delhi ensures cleanliness, hygiene, and 100% safety, while our out-call services offer doorstep delivery for added ease.
We value your time and money, hence we kindly request pic collectors, time-passers, and bargain hunters to refrain from contacting us. l Ludhiana, Majestic Grand Hotel, Ramada by Wyndham Ludhiana City Centre, Park Plaza Ludhiana, Windsor Fountain, G.T Road Ludhiana escort all Ludhiana service Russian available model female girls in Ludhiana VIP Lo price personal Ludhiana off class call girls payment high profile model and female escort 70% Off On Your First Booking Ludhiana Call Girls Service Cash Payment
Welcome to DILPREET Ludhiana Call Girl Service, the Trusted call girl agency around. We Offer 70% Discount On Your First Booking For Ludhiana Call Girls Service Cash Payment is available.🍑👄Ludhiana Escorts Service☎️98157-77685🍑👄 Call Girl service in Ludhiana☎️Ludh...

🍑👄Ludhiana Escorts Service☎️98157-77685🍑👄 Call Girl service in Ludhiana☎️Ludh...dilpreetentertainmen
❤️Chandigarh Escorts Service☎️9815457724☎️ Call Girl service in Chandigarh☎️ Chandigarh Call Girls Service ☎️ Call Girls In Chandigarh BEST Call Girls in CHANDIGARH Escort Service provide Cute Nice sweet and Sexy Models in beautiful CHANDIGARH city cash in hand to hand call girl in CHANDIGARH and CHANDIGARH escorts. HOT & SEXY MODELS // COLLEGE GIRLS IN CHANDIGARH AVAILABLE FOR COMPLETE ENJOYMENT WITH HIGH PROFILE INDIAN MODEL AVAILABLE HOTEL & HOME ★ SAFE AND SECURE HIGH CLASS SERVICE AFFORDABLE RATE ★ 100% SATISFACTION,UNLIMITED ENJOYMENT. ★ All Meetings are confidential and no information is provided to any one at any cost.
★ EXCLUSIVE Profiles Are Safe and Consensual with Most Limits Respected
★ Service Available In: - HOME & 24x7 :: 3 * 5 *7 *Star Hotel Service .In Call & Out call
Services :
★ A-Level (5 star escort)
★ Strip-tease
★ BBBJ (Bareback Blowjob)Receive advanced sexual techniques in different mode make their life more pleasurable.
★ Spending time in hotel rooms
★ BJ (Blowjob Without a Condom)
★ Completion (Oral to completion)
★ Covered (Covered blowjob Without a Condom)Chandigarh Call Girls❤️Chandigarh Escorts Service☎️9815457724☎️ Call Girl service in Chandigarh☎️ ...

❤️Chandigarh Escorts Service☎️9815457724☎️ Call Girl service in Chandigarh☎️ ...Rashmi Entertainment
Recently uploaded (20)
❤️Call Girl In Chandigarh☎️9814379184☎️ Call Girl service in Chandigarh☎️ Cha...

❤️Call Girl In Chandigarh☎️9814379184☎️ Call Girl service in Chandigarh☎️ Cha...
Delhi Call Girl Service 📞8650700400📞Just Call Divya📲 Call Girl In Delhi No💰Ad...

Delhi Call Girl Service 📞8650700400📞Just Call Divya📲 Call Girl In Delhi No💰Ad...
Call Now ☎ 8868886958 || Call Girls in Chandigarh Escort Service Chandigarh

Call Now ☎ 8868886958 || Call Girls in Chandigarh Escort Service Chandigarh
Low Rate Call Girls Udaipur {9xx000xx09} ❤️VVIP NISHA CCall Girls in Udaipur ...

Low Rate Call Girls Udaipur {9xx000xx09} ❤️VVIP NISHA CCall Girls in Udaipur ...
🍑👄Ludhiana Escorts Service☎️98157-77685🍑👄 Call Girl service in Ludhiana☎️Ludh...

🍑👄Ludhiana Escorts Service☎️98157-77685🍑👄 Call Girl service in Ludhiana☎️Ludh...
💞 Safe And Secure Call Girls Nanded 🧿 9332606886 🧿 High Class Call Girl Servi...

💞 Safe And Secure Call Girls Nanded 🧿 9332606886 🧿 High Class Call Girl Servi...
Indore Call Girl Service 📞9235973566📞Just Call Inaaya📲 Call Girls In Indore N...

Indore Call Girl Service 📞9235973566📞Just Call Inaaya📲 Call Girls In Indore N...
💞 Safe And Secure Call Girls chhindwara 🧿 9332606886 🧿 High Class Call Girl S...

💞 Safe And Secure Call Girls chhindwara 🧿 9332606886 🧿 High Class Call Girl S...
Low Rate Call Girls Pune {9xx000xx09} ❤️VVIP NISHA Call Girls in Pune Maharas...

Low Rate Call Girls Pune {9xx000xx09} ❤️VVIP NISHA Call Girls in Pune Maharas...
Low Rate Call Girls Goa {9xx000xx09} ❤️VVIP NISHA CCall Girls in Goa Escort s...

Low Rate Call Girls Goa {9xx000xx09} ❤️VVIP NISHA CCall Girls in Goa Escort s...
❤️ Zirakpur Call Girl Service ☎️9878799926☎️ Call Girl service in Zirakpur ☎...

❤️ Zirakpur Call Girl Service ☎️9878799926☎️ Call Girl service in Zirakpur ☎...
💸Cash Payment No Advance Call Girls Hyderabad 🧿 9332606886 🧿 High Class Call ...

💸Cash Payment No Advance Call Girls Hyderabad 🧿 9332606886 🧿 High Class Call ...
Gorgeous Call Girls In Pune {9xx000xx09} ❤️VVIP ANKITA Call Girl in Pune Maha...

Gorgeous Call Girls In Pune {9xx000xx09} ❤️VVIP ANKITA Call Girl in Pune Maha...
💞 Safe And Secure Call Girls Coimbatore 🧿 9332606886 🧿 High Class Call Girl S...

💞 Safe And Secure Call Girls Coimbatore 🧿 9332606886 🧿 High Class Call Girl S...
❤️Chandigarh Escorts Service☎️9815457724☎️ Call Girl service in Chandigarh☎️ ...

❤️Chandigarh Escorts Service☎️9815457724☎️ Call Girl service in Chandigarh☎️ ...
Call Girls Service Amritsar Just Call 9352988975 Top Class Call Girl Service ...

Call Girls Service Amritsar Just Call 9352988975 Top Class Call Girl Service ...
❤️Chandigarh Escorts Service☎️9814379184☎️ Call Girl service in Chandigarh☎️ ...

❤️Chandigarh Escorts Service☎️9814379184☎️ Call Girl service in Chandigarh☎️ ...
science quiz bee questions.doc FOR ELEMENTARY SCIENCE

science quiz bee questions.doc FOR ELEMENTARY SCIENCE
Antepartum haemorrhage i
- 2. DEFINITION • It is defined as bleeding from or into the genital tract after the 28th week of pregnancy but before the birth of the baby. • Incidence -3% amongst hospital deliveries.
- 3. CAUSES
- 4. PLACENTA PREVIA When the placenta is implanted partially or completely over the lower uterine segment (over and adjacent to the internal os) it is called PLACENTA PREVIA. INCIDENCE: -About one-third cases of antepartum hemorrhage. -The incidence of placenta previa ranges from 0.5–1%. -In 80% cases, it is found to multiparous women. -Incidence increases beyond the age of 35, with high birth order pregnancies and in multiple pregnancy.
- 5. ETIOLOGY • Dropping down theory • Persistence of chorionic activity in the decidua capsularis and its development into capsular placenta • Defective decidua • Big surface area of placenta
- 6. Predisposing factors • Multiparity • Increased maternal age(>35yrs) • History of previous cesarean section or any other scar in the uterus (myomectomy or hysterotomy) • Placental size and abnormality (succenturiate lobes) • Smoking • Prior curettage
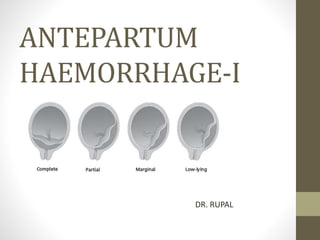
- 7. TYPES/DEGREES OF PLACENTA PREVIA *For clinical purpose, the types are graded into Mild degree (Type-I and II anterior) and Major degree (Type-IIposterior, III and IV).
- 8. CLINICAL FEATURES SYMPTOMS ONLY SYMPTOM- VAGINAL BLEEDING Classical features of bleeeding suddenonset,painless,apparently causeless and recurrent. • 5% cases occurs for the first time during labor, especially in primigravidae. • one-third of cases, there is a history of “warning hemorrhage” usually slight. • bleeding is unrelated to activity and often occurs during sleep and the patient becomes frightened on awakening to find herself in a pool of blood
- 9. • SIGNS General condition and anemia are proportionate to the visible blood loss. ABDOMINAL EXAMINATION The size of the uterus is proportionate to the period of gestation. The uterus feels relaxed, soft and elastic Persistence of malpresentation like breech or transverse or unstable lie is more frequent. The head - floating Fetal heart sound is usually present, unless there is major separation of the placenta with the patient
- 10. • VULVAL INSPECTION -blood is bright red • Vaginal examination must not be done outside the operation theater in the hospital, as it can provoke further separation of placenta with torrential hemorrhage and may be fatal • CONFIRMATION OF DIAGNOSIS- USG
- 12. MANAGEMENT IMMEDIATE (1) Amount of the blood Loss assessed — by noting the general condition, pallor, pulse rate and blood pressure (2) Blood samples are taken for group, cross matching and estimation of hemoglobin (3) A large-bore IV cannula is sited and an infusion of normal saline is started and compatible cross matched blood transfusion should be arranged (4) Gentle abdominal palpation to ascertain any uterine tenderness and auscultation to note the fetal heart rate (5)Inspection of the vulva to note the presence of any active bleeding. (6)Confirmation of diagnosis is made from the history, physical examination and with USG.
- 13. EXPECTANT MANAGEMENT Macafee and Johnson (1945) • The aim is to continue pregnancy for fetal maturity without compromising the maternal health. • Vital prerequisites: (1)Availability of blood for transfusion whenever required (2)Facilities for cesarean section should be available throughout 24 hours. • Selection of cases: (1)Mother is in good health status(hemoglobin > 10 g%; hematocrit > 30%) (2)Duration of pregnancy is less than 37 weeks (3)Active vaginal bleeding is absent (4) Fetal well being is assured (USG).
- 14. (1) Bed rest with bathroom privileges (2) Investigations—like hemoglobin estimation, blood grouping and urine for protein are done (3) Periodic inspection of the vulval pads and fetal surveillance with USG at interval of 2–3 weeks (see p. 244) (4) Supplementary hematinics (5) When the patient is allowed out of the bed (2-3 days after the bleeding stops), a gentle speculum examination is made to exclude local cervical and vaginal lesions for bleeding. (6) Use of tocolysis (magnesium sulfate) can be done if vaginal bleeding is associated with uterine contractions (7) Rh immunoglobin should be given to all Rh negative (unsensitized) women.
- 15. • Expectant management at Hospital or at Home? Hospital setting is ideal. home care may be allowed in some. Selected cases are — (a) patient lives close to hospital (b) 24-hour transportation is available (c) Bed rest assured and (d) patient is well motivated to understand the risks. • Termination of the expectant treatment:37 weeks of pregnancy. • Steroid therapy is indicated when the duration of pregnancy is less than 34 weeks
- 16. ACTIVE MANAGEMENT(DELIVERY) Bleeding occurs at or after 37 weeks of pregnancy Patient is in labor Patient is in exsanguinated state on admission Bleeding is continuing and of moderate degree Baby is dead or known to be congenitally deformed DEFINITIVE MANAGEMENT • Cesarean delivery –placental edge is within 2 cm from the internal os. • Vaginal delivery -placenta edge is clearly 2–3 cm away from the internal cervical os