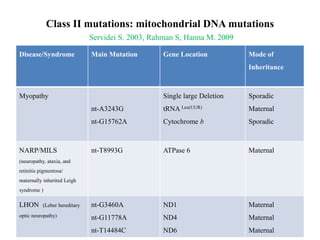
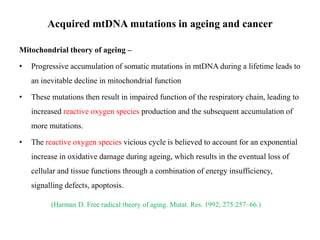
Mitochondrial diseases are caused by defects in mitochondrial structure or enzymes that result in deficient energy production. They can affect multiple organ systems and occur across all age groups. Mitochondrial DNA mutations can be inherited from the mother and nuclear DNA mutations can affect mitochondrial proteins or DNA maintenance. Common mitochondrial diseases include MELAS, MERRF, and Leigh syndrome. Mitochondrial dysfunction has also been implicated in aging and common diseases like heart disease and Parkinson's.































![General Principles of Treatment
Treat Underlying Neurologic Issues
• Seizures (antiepileptic drugs, avoid valproic acid).
• Spasticity (baclofen, botulinum toxin [focal]; avoid dantrolene if liver is
involved).
• Dystonia (diazepam, botulinum toxin [focal], trihexyphenidyl).
• Headache (acute: nonsteroidal anti-inflammatory drugs and acetaminophen;
avoid aspirin and triptans in MELAS, chronic: amitriptyline, calcium blockers,
riboflavin, coenzyme Q10, -lipoic acid).](https://image.slidesharecdn.com/mitochondrialdiseases-140122103237-phpapp02/85/Mitochondrial-diseases-37-320.jpg)

