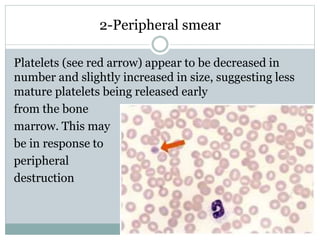
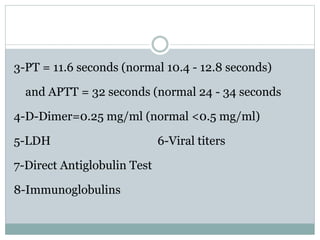
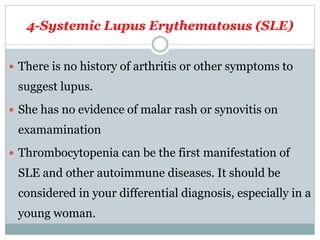
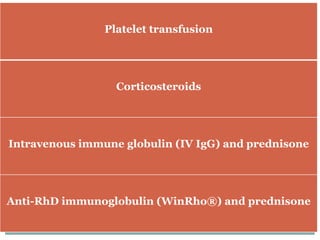
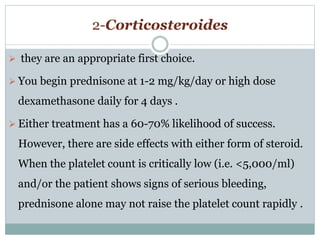
A 23-year old female presents with a rash, bruising, nosebleeds, and heavy menstruation. Her physical exam and labs reveal an isolated thrombocytopenia. Her peripheral smear shows decreased platelet numbers and slightly larger platelets, suggesting early release from the bone marrow in response to peripheral destruction. Further history and testing are needed to determine the cause of the thrombocytopenia.