Veterinary critical care fluid resuscitation debate
- 1. State of the Art Review Journal of Veterinary Emergency and Critical Care 25(1) 2015, pp 6–19 doi: 10.1111/vec.12281 The crystalloid-colloid debate: Consequences of resuscitation fluid selection in veterinary critical care Dava Cazzolli, DVM and Jennifer Prittie, DVM, DACVIM, DACVECC Abstract Objective – To provide a comprehensive review of the current literature in human and veterinary medicine evaluating the impact of resuscitation fluid choice on patient outcome and adverse effects. Data Sources – Prospective and retrospective studies, experimental models, and review articles in both human and veterinary medicine retrieved via PubMed. Human Data Synthesis – A series of recent, large, randomized controlled trials in critically ill human patients comparing crystalloid versus colloid driven fluid resuscitation algorithms have demonstrated no outcome ben- efit with the use of natural or synthetic colloids. Synthetic colloidal solutions are associated with an increased incidence of adverse effects including acute kidney injury, need for renal replacement therapy, and coagu- lopathies. Further, colloidal solutions demonstrate a larger volume of distribution in the setting of critical illness than hypothesized. These findings have created controversy regarding colloid fluid resuscitation in critically ill patients and challenge current resuscitation strategies. A thorough review of the most influential human data is provided. Veterinary Data Synthesis – No veterinary clinical outcome data pertaining to fluid resuscitation choice cur- rently exist. Veterinary data from experimental and small clinical trials evaluating the coagulopathic effects of hydroxyethyl starch solutions are described. Data pertaining to the use of natural colloids and albumin prod- ucts in clinical veterinary patients are reviewed. In addition, data pertaining to the comparative intravascular volume expansion effectiveness of different fluid types in canine patients are reviewed. Conclusions – Clinical data from critically ill human patients have failed to demonstrate an outcome advantage associated with colloidal fluid resuscitation and indicate that hydroxyethyl starch solutions may be associated with significant adverse effects, including acute kidney injury, need for renal replacement therapy, coagu- lopathies, and pathologic tissue uptake. The ability to apply these findings to veterinary patients is unknown; however, similar pathophysiology may apply, and critical re-evaluation of resuscitation strategies is justified. (J Vet Emerg Crit Care 2015; 25(1): 6–19) doi: 10.1111/vec.12281 Keywords: AKI, coagulopathy, colloid, fluid resuscitation, hydroxyethyl starch Abbreviations AKI acute kidney injury COP colloid osmotic pressure CT closure time EG endothelial glycocalyx ESL endothelial surface layer HES hydroxyethyl starch From the Animal Medical Center, Department of Emergency and Critical Care, New York, NY. Dr. Prittie is an Assistant Editor for the Journal, but only participated in the peer review process as an author. The authors declare no other conflict of interest. Address correspondence and reprint requests to Dr. Dava Cazzolli, Animal Medical Center, 510 East 62nd Street, New York, NY 10065. Email: dava.cazzolli@amcny.org Submitted March 28, 2014; Accepted October 30, 2014. HDS hemodynamic stabilization HSA human serum albumin ICU intensive care unit LPS lipopolysaccharide MS molar substitution MW molecular weight RRT renal replacement therapy RCT randomized controlled trial RIFLE risk, injury, failure, loss, end-stage kidney dis- ease vWF von Willebrand factor Introduction Intravenous fluid resuscitation plays a pivotal role in the treatment of circulatory failure in the emergency and intensive care unit (ICU) settings. Early goal 6 C Veterinary Emergency and Critical Care Society 2015
- 2. Crystalloids-colloid controversy directed therapy has demonstrated an outcome benefit in human septic shock patients and likely imparts a survival advantage in other patient populations as well.1,2 This treatment strategy directs resuscitation toward restoration of an effective circulating blood volume and adequate end-organ perfusion. Expansion of the intravascular space with exogenous fluids is a first line therapeutic intervention to restore perfusion and a fundamental component of early goal directed therapy. In the past decade, evidence-based clinical data have evolved in the human medical field, evaluating the impact of resuscitation fluid choice on patient mor- bidity and mortality.3 Until similar data are available evaluating fluid choice in veterinary shock patients, vet- erinarians are, in part, reliant on extrapolation of results from human clinical trials to guide resuscitation efforts. Across species, the optimal choice of resuscitation fluid remains controversial and is a matter of ongoing debate. Administration of any fluid intravenously will induce immediate plasma volume expansion. However, fluid types have variable systemic effects beyond expansion of the intravascular space and these effects may impact pa- tient outcome.3–5 As with other drugs utilized in the crit- ical care setting, the pharmacologic properties of certain fluids can impact organ function, modulate the immune system, and alter coagulation. In addition, fluids can in- fluence microcirculatory flow and perfusion by both di- rect and indirect effects on blood viscosity, red blood cell rheology, and endothelial function.5–7 The use of IV flu- ids in the medical field predates the initiation of modern stringent drug approval regulations by the Federal Drug Administration and until recently there has been little to no testing on the safety or efficacy of many of the com- monly used fluid types.8,9 No individual fluid is ideal, each type carrying its own inherent safety and toxicity profile. The most utilized resuscitation fluids in human and veterinary medicine are reviewed, with a specific focus on the expanding body of evidence surrounding the controversy between crystalloid and colloid driven resuscitation strategies in the critical care setting. Crystalloid Fluids Isotonic crystalloid fluid solutions remain the mainstay of fluid resuscitation in both human and veterinary medicine. Crystalloids are salt solutions that convey negligible oncotic pressure across the endothelial barrier. Infusion results in rapid dissemination into the entire extracellular fluid space, with 60–80% of the administered volume redistributed out of the vascular space and into the interstitium within 30–60 minutes. Substantial fluid volumes are required to adequately expand the intravascular space, correct hypovolemia, and restore end-organ perfusion in circulatory failure.3,5 Normal saline (0.9%) is the most frequently used replacement fluid in the human medical field. Although isotonic, normal saline is not a physiologic solution, con- taining a significantly higher chloride concentration and lower strong ion difference when compared to plasma.10 Resuscitation of critically ill patients with large vol- umes of normal saline may result in hypernatremia, hyperchloremia, and contribute to the development of a hyperchloremic metabolic acidosis. In addition, there is documented risk of hyperchloremia-induced acute kidney injury (AKI). This kidney injury is postulated to result from high chloride levels inducing renal vasoconstriction, decreased glomerular filtration, and subsequent ischemic renal tubular damage.11 Given the potential complications associated with 0.9% saline, isotonic crystalloid solutions such as lactated Ringer’s and Normosol-R have become increas- ingly popular for resuscitative purposes. These solutions are more physiologic than saline, containing a myriad of electrolytes as well as a buffer, typically lactate or acetate. The buffer additive requires metabolism prior to excretion, so theoretical contraindications to use of these solutions exist in particular disease states such as hepatic dysfunction.3 Human clinical trials have demonstrated that administration of a balanced salt solution over normal saline in surgical patients and critically ill patients was associated with a significant decrease in the rate of major complications, including postoperative infection, renal replacement therapy (RRT), and need for blood transfusion.12,13 A recent large, retrospective study in critically ill adults with sepsis found that resuscitation with balanced solutions, as opposed to normal saline, was associated with a lower risk of in-hospital mortality.14 A large scale, randomized controlled trial (RCT) comparing the effects of saline and balanced salt solutions is yet to be completed. The net positive fluid balance that occurs secondary to aggressive resuscitation with crystalloids is associ- ated with worsened patient outcome.15 Expansion of the total extracellular space causes direct damage to the architecture of the endothelial surface layer (ESL), culminating in impaired capillary exchange. Progressive capillary leak, tissue edema, and hypoxia ensue, with subsequent detrimental effects on cardiovascular, pul- monary, gastrointestinal, and renal function.5 Isotonic crystalloid administration induces a proinflammatory state, with augmented inflammatory cytokine produc- tion and endothelial cell activation.4,5 This exaggerated inflammatory response exacerbates the deleterious effects of fluid overload, generating worsened edema formation. Other forms of resuscitation injury include development of dilutional coagulopathy, compartment syndromes, and impaired tissue healing.5 At the cellular level, aggressive volume resuscitation incites cellular C Veterinary Emergency and Critical Care Society 2015, doi: 10.1111/vec.12281 7
- 3. D. Cazzolli J. Prittie swelling, leading to cytosolic acidification, altered intracellular protein function and signaling pathways, and ultimately impaired cell activity.5 Several publications in the human medical field have demonstrated that fluid overload in the ICU setting is a common problem and is independently associated with increased morbidity and mortality.16–25 Hospitalized critically ill veterinary patients are likely prone to a similar increased risk for fluid overload and the related negative sequelae. A recent retrospective study comparing critically ill dogs to a stable popu- lation of neuroorthopedic dogs found that, over the course of hospitalization, critically ill dogs acquired a higher percent fluid overload (11.8 ± 1.7% versus 0.9 ± 2.6%, P = 0.001), which was directly correlated with mortality.26 Initial concerns that fluid overload may be a biomarker of illness severity have been replaced by the common belief that fluid overload in itself is a morbidity. Colloidal Solutions The selection of a resuscitation fluid with a volume of distribution limited to the intravascular space should minimize tissue edema formation. This purported advantage over isotonic crystalloids has led to the in- creasingly common use of colloidal resuscitation fluids in both human and veterinary medicine. Both natural and synthetic colloids carry the attractive theoretical benefit of a volume-sparing effect with a decreased risk of inducing a positive fluid balance.27 These solutions contain large molecules that cannot cross an intact vascular barrier. The effective oncotic pressure imparted by colloids across the endothelium is variable between specific solutions. According to Starling’s classic model of transcapillary fluid exchange, solutions hyperoncotic to plasma may generate a larger oncotic gradient across the endothelial barrier. This gradient functions to impede fluid movement to the interstitium and further augment the intravascular volume.10,27 In this regard, the theoretical volume-expanding ability of certain colloids may exceed the volume of fluid administered. Natural Colloids The existence of a readily available, isooncotic, species- specific albumin accounts for the more common implementation of natural colloidal solutions in human over veterinary fluid resuscitation algorithms. Albumin- containing fluids are theorized to confer benefits that surpass the colloidal and volume-sparing effects, includ- ing roles in serum drug and hormone binding, protection from oxidative damage, anticoagulant effects, and main- tenance of vascular integrity.28 The most frequently uti- lized natural colloid in human critical care is 4% human serum albumin (HSA), an isooncotic solution of purified albumin. Purified HSA solutions are also commercially available in concentrations ranging from 4% to 25%. Human serum albumin has been utilized in clinical veterinary patients, despite concerns regarding incom- plete protein homology among species.28–31 Several veterinary reports have demonstrated severe, even fatal, type III hypersensitivity reactions in dogs treated with HSA.32,33 There is also a significant risk with repeat administration, as high levels of anti-HSA antibody are produced in dogs within weeks of administration.34 Se- vere hypersensitivity reactions were purportedly limited to HSA administration to healthy dogs, due to an ab- sence of documentation with administration to critically ill dogs. This disparity has been postulated to be related to the immune compromise that occurs in the setting of critical illness,35 as critically ill patients are often less able to mount a significant immune response. In accord with this theory, decreased HSA-antibody production has been documented in critically ill as compared with healthy dogs.34 However, Powell et al recently published confirmed type III hypersensitivity reactions in 2 ill dogs treated with HSA, demonstrating that critical illness does not preclude the risk of antigenic reactions to this solution.35 The administration of HSA solutions to vet- erinary patients is controversial and likely not indicated for resuscitation purposes. This solution may have a role in treatment of specific populations of severely hypoalbuminemic veterinary patients provided there is clinician recognition of the associated risks. There is currently no equivalent, commercially available, species-specific, isooncotic natural colloid for use in veterinary patients. Lyophilized canine-specific albumin is sporadically available and may play a central role in canine fluid resuscitation in the future. In a small veterinary clinical trial, canine-specific albumin administration in 7 dogs with septic peritonitis resulted in increased albumin concentrations, colloid osmotic pressure (COP), and diastolic blood pressure 2 hours post-transfusion, as compared with a matched, clinician- directed therapy control group.36 The product appeared to have an acceptable safety profile. At this time, other clinical safety and efficacy data for this product are lacking and larger clinical trials are warranted. Plasma products such as frozen plasma (FP) and fresh frozen plasma (FFP) are isooncotic natural colloids that can be incorporated into resuscitation algorithms in sick human and veterinary patients. Across species, plasma (and other blood) products are used primarily for patients with acute hemorrhage or coagulopathy.4,37,38 These solutions provide albumin, coagulation factors, and immunoglobulins, among other plasma components. The administration of plasma products carries the risk of transfusion-related 8 C Veterinary Emergency and Critical Care Society 2015, doi: 10.1111/vec.12281
- 4. Crystalloids-colloid controversy Table 1: Nomenclature and classification of various available HES solutions42 Generation MW/MS Concentration Classification C2/C6 Carrier Solution Trade Name 1st 670/0.75 6% Hetastarch 4.5:1 Balanced Hextend 600/.07 6% Hetastarch 5:1 Saline Hespan 480/0.7 6% Hetastarch 5:1 Saline Plasmasteril 2nd 200/0.62 6% Hexastarch 9:1 Saline Elohes 200/0.5 6% or 10% Pentastarch 5:1 Saline Pentaspan 70/0.5 6% Pentastarch 3:1 Balanced Hemohes 3rd 130/0.42 6% or 10% Tetrastarch 6:1 Saline Tetraspan Vetstarch Voluven 130/0.42 6% or 10% Tetrastarch 6:1 Balanced Volulyte MW, molecular weight; MS, molar substitution. adverse events including febrile nonhemolytic trans- fusion reactions (FNHTR), transfusion-related acute lung injury (TRALI), immunomodulation, and potential pathogen transmission.4,37 Large volumes of plasma are required to increase serum albumin concentrations and affect plasma COP, especially in the face of ongoing protein loss (eg, 40 mL/kg of plasma is required to increase serum albumin concentration by 1 g/dL).29 In veterinary patients, limited availability and expense must also be taken into consideration. Synthetic Colloids Artificial colloids were developed as an alternate resus- citation fluid to albumin.39 Hydroxyethyl starch (HES) solutions were first introduced in the 1970s and are the most common synthetic colloid currently utilized in hu- man and veterinary patients in the United States.40 The remaining 2 classes of synthetic colloids, gelatins and dextrans, are used less frequently.39 Accordingly, the ma- jority of recently published clinical data comparing the use of colloidal to crystalloid fluids for resuscitation fo- cus on HES solutions.41–44 Hydroxyethyl starch solutions are readily available and inexpensive, provide rapid volume expansion, and have a volume of distribution theoretically limited to the intravascular space, making them an appealing replacement for isotonic crystalloids and natural colloids.40,45 Despite these promising char- acteristics, clinical evidence of morbidity reduction and survival advantage in ill patients is lacking. Hydroxyethyl starches Hydroxyethyl starches are polydisperse modified nat- ural polysaccharides, structurally similar to glycogen, dissolved in saline or a more balanced salt carrier. These polysaccharides are derived from amylopectin, a complex plant starch polymer obtained from waxy maize or potatoes.40,45 Natural starches cannot be used as a plasma substitute due to their relative instability and rapid degradation by plasma amylases.45 However, modification of the base polysaccharide by substitution of hydroxyethyl groups in place of hydroxyl groups results in increased solubility and decelerates the hydrolysis of the molecule by serum amylase.46,47 The molecular modification of the polysaccharide creates significant variation in the pharmacokinetic and phar- macodynamic profile of the resultant HES solution.40 Hydroxyethyl starch solutions are available in an isoon- cotic formulation (6%) and hyperoncotic formulation (10%), the latter of which has gone out of favor due to safety concerns.48 These fluids are named based on their concentration, average molecular weight (MW), and molar substitution (MS). The nomenclature used for HES solutions is outlined in Table 1 and described briefly below. Degradation of HES molecules, and ultimately HES half-life, is determined by serum amylase activity as well as the molecular structure of HES.40 Differences in serum amylase activity exist between species. Dogs have 3 times more serum amylase activity than people, and accordingly, have documented accelerated plasma HES clearance.49 The rate of HES degradation by serum amylase is dependent on the product MW, MS, and C2/C6 substitution ratio. Of these, MS and C2/C6 ratio are the most influential features.47 Continuous degrada- tion of larger HES molecules into smaller ones functions as a reservoir for colloidal replenishment. This affords larger MW solutions a longer overall plasma half-life and greater capacity for ongoing oncotic support.40 Molar substitution refers to the number of hydroxy- ethyl groups substituted per 100 available anhydrous glucose residue binding sites; hence, an MS of 0.5 indi- cates that 50% of available binding sites are occupied. The MS dictates starch classification, eg, 0.4 MS is a tetrastarch, 0.5 a pentastarch. Increasing MS is positively correlated with HES plasma half-life and retarded degradation, with plasma clearance of tetrastarches at least 20 times higher than that of hetastarch or pentastarch.50 Tetrastarch solutions, such as Voluven, Vetstarch, and Tetraspan, were introduced to the clinical market most recently and are considered late generation. C Veterinary Emergency and Critical Care Society 2015, doi: 10.1111/vec.12281 9
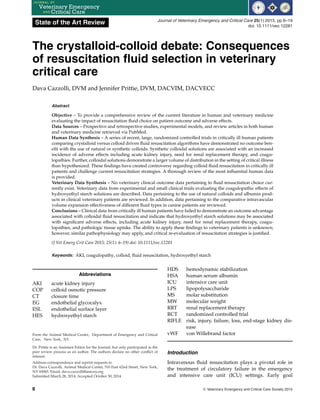
- 5. D. Cazzolli J. Prittie Figure 1: Structural formula of hydroxyethyl starch, with carbons 1–6 of the base glucose subunit labeled. The polymerized glucose units are principally connected via 1–4 linkages, as depicted above, but also have several 1–6 starch branch points. R=H or hydroxyethy (CH2CH2OH) substitution point; R1–H, hydroxyethyl group or glucose branching point. Cleavage by serum ␣-amylase occurs between the C1–4 polymer linkages (labeled A). These products were expected to carry improved safety profiles compared to early generation, high MW/MS solutions, due to conjectured diminished plasma and tissue retention.40 Hydroxyethyl groups are substituted on the C2, C3, and C6 carbons of the base glucose monomer (Figure 1). The pattern of substitution among these 3 sites affects amylase affinity and ultimately degradation efficacy. Substitution on the C2 position in particular leads to allosteric inhibition of the cleavage of the HES molecule by plasma amylases, resulting in an increased plasma half-life of the HES solution. Comparable products, ie, with the same MW/MS, that differ solely in the C2/C6 substitution ratio have been shown to have very different pharmacokinetics and plasma half-lives; an increase in the C2/C6 substitution ratio is inversely cor- related with rate of degradation.37,46,47 These molecular modifications prolong plasma half-life and can lead to significant plasma accumulation of colloid, even in the presence of high amylase activity. Highly substituted HES products have a terminal half-life that increases with repetitive dosing as well as with longer infusion durations.46 After initial intravascular hydrolysis by serum amy- lase, smaller HES molecules (55 kDa) are excreted unchanged in the urine or are taken up into tissues, namely, cells of the reticuloendothelial system.40 Cellular uptake of larger HES molecules (55 kDa) also occurs but with decreased frequency, and subsequent slow intracellular degradation ensues.40 Cellular lysosomes lack the amylase enzymes required for efficient HES hydrolysis, making the half-life of HES in tissues far longer than in plasma. In the presence of an intact, healthy ESL, the volume of distribution of HES solutions is theoretically limited to the intravascular space.51–53 The large osmotically active particles in these solutions retain water within the plasma compartment and impede tissue edema. Moreover, the large MW of HES molecules allows for absorption into the glycocalyx layer of the ESL and further augments resistance to ultrafiltration of fluid across the capillary barrier.51 Adverse Effects The most significant adverse effects reported with the use of synthetic colloids are coagulation disorders, AKI, and increased mortality. Other documented adverse effects include pruritus, reticuloendothelial dysfunction, hepatopathies, and anaphylactoid reactions.8 Specific patient populations, particularly septic patients, appear to be at higher risk of adverse effects, and administration of artificial colloids to these patients may be associated with increased mortality. Significant debate surrounds the safety of HES solutions with the most recent clinical data prompting the ban of their use in Europe and guidelines recommending against their use in certain patient cohorts.54,55 It has yet to be determined whether these safety data extend into all patient populations and across species. Coagulopathy Increased postoperative bleeding and transfusion requirements following synthetic colloid administration were first described decades ago and continue to be reported today.56–61 The mechanism of coagulopathy is incompletely elucidated, but is thought to be mediated by direct effects of colloid molecules on the coagulation system and not exclusively via hemodilution.50,62 These effects are known to be dose-dependent with HES solutions and have been reported with administration 10 C Veterinary Emergency and Critical Care Society 2015, doi: 10.1111/vec.12281
- 6. Crystalloids-colloid controversy within the manufacturer recommended daily dosing range. Administration of HES has been shown to lead to platelet dysfunction, reduced von Willebrand factor (vWF) and factor VIII activity, and an acquired fibrino- gen deficiency or dysfunction.50 Likewise, both gelatin and dextran solutions have demonstrated interference with both primary and secondary hemostasis.62 The pathophysiology of HES-induced platelet dysfunction is multifactorial. Hydroxyethyl starch molecules induce cellular abnormalities that result in de- creased agonist-induced expression of the glycoprotein (GP) ␣IIb/3 receptor on platelet surfaces, culminating in inhibited platelet adhesion and aggregation and pro- longed measured platelet closure time (CT).50 There is additional evidence that HES molecules may bind to and coat the platelet surface, leading to further inhibition of activation, aggregation, and adhesion to fibrinogen. Ef- fects on platelet dysfunction are more pronounced with administration of early generation HES solutions, and this has been corroborated by both human and veteri- nary data.50,62–71 Smart et al performed an in vivo study evaluating the effect of a 20 mL/kg dose of HES 670/0.75, a high MW HES solution, on platelet function in healthy dogs and found a significantly prolonged platelet CT that persisted for 24 hours.65 The effect on platelet func- tion of this HES solution has also been evaluated after a 24-hour constant rate infusion (CRI) in healthy dogs. Administration of a CRI caused a significant increase in platelet CT from baseline until the end of the infusion. A CRI of 2 mL/kg/hr resulted in a platelet CT above the normal reference interval in a majority of the treated dogs.72 No clinical evidence of bleeding was detected in any dog in this study. Additional veterinary in vitro data, including data on newer generation HES solutions, have shown a dose-dependent prolongation of platelet CT with HES as compared with saline-hemodilution.66–70 Along with alterations in primary hemostasis, syn- thetic colloids can also produce changes in secondary hemostasis. Acquired von Willebrand syndrome with decreased factor VIII activity is a recognized conse- quence of administration of all classes of synthetic colloids.50,62 Data from both patients and healthy human volunteers have shown up to 80% reduction in circulating factor VIII and vWF activity after HES administration within the manufacturer dosing range. Although the precise pathophysiology remains in- completely understood, binding of colloids to factor VIII/vWF complexes is postulated to accelerate complex clearance from the plasma.50,62 Clinical data have also revealed reduced fibrino- gen concentrations, impaired fibrin crosslinking, and compromised clot stability associated with the admin- istration of both dextran and HES solutions.71 Current data demonstrate that hemodilution with HES results in a weaker clot, less stable fibrin network, and less firm platelet aggregation, as compared to crystalloid or al- bumin hemodilution.64 Viscoelastic coagulation studies in human and veterinary patients have demonstrated patterns consistent with hypocoaguability following both in vivo and in vitro HES hemodilution.64,73–75 A recent systematic review on viscoelastic analysis of HES 130/0.4 in human patients that incorporated data from 7 in vitro and 7 in vivo studies found a significant hypocoagulatory effect of HES on the kinetics of clot formation.64 This effect was found to be dose-dependent; however, significant effects were still noted at low doses (40 mL/kg). Falco et al reported a hypocoaguable thromboestometric pattern with in vitro HES 130/0.4-hemodilution (eg, Vetstarch) of canine blood (1:4 and 1:10 dilutions), purportedly mediated by changes in fibrinogen concentration and platelet function.75 A small randomized, prospective veterinary trial was published evaluating the hemostatic effects and clinical bleeding associated with 6% HES (600/.75), as compared with lactated Ringer’s solution (LRS), in healthy dogs anesthetized for orthopedic surgery.76 Dogs in this study were given either a 10 mL/kg bolus of HES or LRS, followed by a maintenance infusion of 10 mL/kg/hr of LRS during anesthesia. Although there was a significant prolongation of prothrombin time and buccal mucosal bleeding time at 1 hr postinfusion in both groups, there was no significant difference between groups in vWF antigen concentration, fVIII coagu- lant activity, platelet aggregation or clinical bleeding.76 Hypotheses that tetrastarches would be devoid of hemo- static impairment in people remain unsubstantiated, and recent data evaluating these solutions have shown reduced, but not absent, HES-associated coagulation abnormalities and clinical bleeding tendencies.57–60 The risk for clinical bleeding in veterinary patients treated with HES solutions has not been clarified. Acute Kidney Injury All classes of synthetic colloids have been associated with renal impairment; however, HES solutions have been cited most frequently.39,77–79 Shortgen et al pub- lished the first large, RCT documenting an increased incidence of AKI with HES (6%, 200/0.6) administration as compared to a 3% gelatin solution in human patients with sepsis or septic shock.80 Since then, several RCTs have demonstrated increased incidence of AKI and need for RRT in heterogeneous human patient populations treated with HES solutions.41–44,81–84 The pathophysi- ology of HES-associated AKI is not fully understood, and several mechanisms have been proposed to explain the tubular injury incurred. Hyperviscosity-mediated ischemic injury, HES uptake by the renal interstitial C Veterinary Emergency and Critical Care Society 2015, doi: 10.1111/vec.12281 11
- 7. D. Cazzolli J. Prittie reticuloendothelial system, and osmotic nephrosis have been proposed pathophysiologies.85–87 Hyperviscosity- mediated injury has largely been discounted but is theoretically possible if a hyperoncotic colloid (eg, 10% HES solutions) is used in a dehydrated patient.87,88 Filtration of HES molecules into the tubular fluid gener- ates a hyperviscous urine, resulting in stasis of flow and obstruction of the tubular lumen. This mechanism of in- jury relies on the creation of hyperoncotic tubular fluid, which has debatable clinical relevance in the setting of critical illness. Experimental models have demonstrated HES-induced renal interstitial cell proliferation and macrophage infiltration and these changes are believed to contribute to the development of AKI.86,87 Lastly, HES solutions can induce osmotic nephrosis, a process of vacuolization and swelling of proximal renal tubular cells after exogenous solute administration, within a few hours of exposure.89 These tubular lesions are reversible structural changes that can be associated with AKI and have been documented with both early and late generation HES administration. Preferential uptake of HES molecules occurs in proximal tubular luminal ep- ithelial cells via pinocytosis, and intracellular lysosomal storage can lead to accumulation of intracellular water, cytoplasmic swelling, and altered cellular integrity and function, culminating in tubular damage and the clinical syndrome of AKI.87,89 Late generation HES solutions were postulated to be less nephrotoxic; however, human clinical trials have continued to document AKI in patients treated with these solutions.42–44 Tissue Accumulation and Pruritus HES molecules have been shown to accumulate in numerous tissues after infusion in human patients and animal models, including reticuloendothelial cells, dermal cells, nerve cells, and hepatocytes, an effect that appears to be unique to HES over other synthetic colloids.90 While tissue uptake of HES is both dose- and time-dependent, HES can accumulate in cytoplasmic vacuoles that can persist for long periods of time even after relatively low-dose infusions of a HES solution for volume replacement.90–92 Intracellular HES accumula- tion is implicated in the pathogenesis of major complica- tions and organ dysfunction. For example, tissue uptake in small peripheral nerves and skin is implicated in HES- associated pruritus and has a reported incidence ranging from 30% to 60% in HES-treated human patients.93 HES- induced pruritus has a delayed onset (typically 1–6 weeks postexposure), is refractory to available thera- pies, and can last up to 24 months.94,95 Current data have failed to support previous hypotheses that newer generation lower MW HES solutions will have reduced tissue uptake and expedited renal excretion. In fact, a recently meta-analysis demonstrated a 42.3% overall tissue uptake of low MW HES ( 200 kDa), as compared with a 24.6% tissue uptake of a high MW HES.91 In- creased renal tubular cell uptake has been postulated to explain the persistent renal toxicity associated with late generation HES solutions.89 Given that many adverse effects, including AKI and potentially mortality, may be correlated with HES cellular uptake, the overall safety profile of late generation HES solutions is challenged. Crystalloid versus Colloid Fluid Resuscitation: The Evidence The absence of a confirmed survival advantage in conjunction with increased documentation of adverse effects is the core of the controversy of continued use of colloidal solutions in the resuscitation of critically ill human patients. Significant disparity exists between the theorized advantages of colloidal therapy and sup- portive clinical data, particularly in patient cohorts with higher illness severity scores. In the past decade several well-designed RCTs have been published in human critical care comparing fluid resuscitation with colloid versus crystalloid.41–44,96,97 Results of these trials have led to safety concerns regarding synthetic colloids and recommendations against their use in several patient populations. Efficacy The efficacy of a resuscitation fluid can be defined as its ability to restore effective circulating blood volume, organ perfusion, and tissue oxygenation while mini- mizing unnecessary fluid loading that could contribute to a positive fluid balance. In several recent studies in critically ill human patients, the volume-sparing effect of colloidal solutions as compared to crystalloids has been marginal, with intravascular volume expansion efficacy close to a ratio of 1.2–1.4:1 for crystalloid:colloid.41–44,96 This is in contrast to the anticipated superior volume expansion predicted from the physiologic properties of colloidal solutions. If only marginal differences in fluid volumes needed to restore effective circulating volume exist between crystalloid and colloid resuscitation in the critically ill state, the inherent advantage of a colloid becomes greatly diminished. Past data from healthy human volunteers and ex- perimental animals demonstrated 3–4 times as much crystalloid than colloid infusion are needed to achieve an equivalent increase in intravascular volume.51,98 Silver- stein et al reported on the comparative change in blood volume in healthy dogs, as assessed by an in-line hemat- ocrit monitor, after an IV bolus of different fluid types. An 80 mL/kg of saline, 4 mL/kg of hypertonic saline (7.5%), 20 mL/kg of dextran-70, and 20 mL/kg of 6% HES were 12 C Veterinary Emergency and Critical Care Society 2015, doi: 10.1111/vec.12281
- 8. Crystalloids-colloid controversy compared.99 Infusion of saline resulted in the largest immediate increase in blood volume, as the percent in- crease was directly correlated with the volume infused. However, this increase was transient and followed by a rapid decline, attributed to prompt fluid redistribution into the interstitium. The synthetic colloidal solutions generated the largest cumulative effects between 30 and 240 minutes, with blood volumes that continued to increase beyond the administration interval. However, through the total study period (0–240 min), there was no statistically significant difference in the volume expand- ing efficiency of either synthetic colloid compared with normal saline.99 A more recent comparative veterinary research study evaluated the effect of tetrastarch ad- ministration on hemodynamic and laboratory variables in healthy dogs and dogs with lipopolysaccharide (LPS)-induced systemic inflammation, as compared with an equal volume of saline.100 Comparable volume- expanding efficacy was found after administration of saline or HES in both healthy and LPS-treated dogs. This was evidenced by similar changes in PCV and plasma protein concentration. Tetrastarch administration led to an expected increase in plasma COP, whereas saline led to a dilutional-associated decrease in COP. Despite the provision of oncotic support, no significant beneficial effect on hemodynamic stabilization (HDS) in the LPS-treated dogs was demonstrated with tetrastarch over normal saline.100 Several human clinical RCTs have investigated the efficacy of colloids as compared to crystalloids in their ability to achieve HDS, as well as the fluid volume required to reach these goals. The SAFE trial, published a decade ago, is the largest published RCT to date comparing the use of 4% HSA to normal saline for fluid resuscitation in human ICU patients. Enrolling approximately 7,000 patients, this study found albumin administration to be safe, but failed to demonstrate a significant volume-sparing effect.101 Similar total fluid volumes were administered between groups. The overall ratio of albumin:crystalloid administration over the first 4 days of the study was 1:1.4.101 More recently, the ALBIOS trial evaluated the use of albumin in human patients with severe sepsis or septic shock.102 Patients were randomized to receive either 20% albumin and crystalloid solution or crystalloid solution alone. Al- bumin replacement, as compared to crystalloids alone, did afford some hemodynamic benefits. However, no significant difference in total administered fluid volume was found between groups.102 The landmark VISEP trial, published in 2008, ran- domized 537 patients with severe sepsis or septic shock to resuscitation with Ringer’s lactate solution (LRS) or a pentastarch solution (10% HES 200/0.5).41 Although pa- tients in the LRS group received more total resuscitation fluid than patients in the HES group, the ratio of total fluid administered in the LRS group compared to that in the HES group was 1.32:1 for the entire study period.41 Similarly, the CRYSTMAS trial, a prospective, random- ized, double-blinded study in 196 patients with severe sepsis, compared resuscitation with 6% HES 130/0.4 (Voluven) versus normal saline. Significantly less study fluid was required to achieve HDS in HES-treated com- pared with saline-treated patients (1379 ± 886 mL versus 1709 ± 1164 mL, P = 0.0185).90 However, cumulative volume of study fluid used over 4 days was similar between groups. Although time to HDS was expedited and initially more efficient with the use of HES, this did not translate into a sustainable volume-sparing effect. Two large, well-designed RCTs, the Scandinavian Starch Trial (S6) and the CHEST trial, were published in 2012 comparing fluid resuscitation with crystalloids alone versus algorithms incorporating colloidal solu- tions in critically ill human patients.42,43 The S6 trial was a multicenter, parallel-group, blinded trial, enrolling 800 patients with severe sepsis. Patients were randomly assigned to fluid resuscitation in the ICU with either 6% HES 130/0.4 (Tetraspan) or Ringer’s acetate at doses up to 33 mL /kg/d.42 No significant difference in trial fluid volumes was found between groups, failing to support a substantial volume-sparing effect of colloid administration in this ill patient population. The CHEST trial has been the largest and most influential study to date critically evaluating the use of HES as a resuscitation fluid in a heterogeneous human ICU patient population. This double-blinded RCT, enrolling 7,000 intensive care patients, compared 6% HES 130/0.4 (Voluven) with normal saline resuscitation in the ICU setting.43 During the first 4 days, the HES group received significantly less study fluid than the saline group (526 ± 425 mL versus 616 ± 488 mL, P 0.001), with most of the volume administered in the first 24 hours of ICU admission. The HES group also received significantly less nonstudy fluid than the saline group (851 ± 675 mL versus 1115 ± 993 mL, P 0.001), resulting in a lower positive net fluid balance (921 ± 1069 mL versus 982 ± 1161 mL, P = 0.03).43 However, as with previous studies, the documented volume-sparing effect of colloidal therapy was far less than predicted. The HES group experienced more rapid HDS, reduced vasopressor doses, and significantly higher central venous pressures than the saline group. Other parameters, such as time to normalization of serum lactate, heart rate, and blood pressure were similar between groups. Evaluating the first 4 days of treatment, there was no difference between groups on overall achievement of HDS.43 These data show colloidal solutions have a larger than predicted volume of distribution in critically ill patients. Augmented fluid dissemination out of the intravascular C Veterinary Emergency and Critical Care Society 2015, doi: 10.1111/vec.12281 13
- 9. D. Cazzolli J. Prittie space is likely multifactorial. Systemic inflammation and the upregulated cytokine production that often accompany critical illness lead to endothelial injury, degradation of the EG, and consequent capillary leak.5 In addition, aggressive fluid resuscitation can exacerbate the already compromised integrity of the vascular barrier by causing direct damage to the EG.52 Patient intravascular volume status may also play a significant role in the distribution of solutions through fluid compartments. Colloidal resuscitation has been demonstrated to be most efficacious in the treatment of intravascular hypovolemia, with 80–100% of the infused volume remaining in the intravas- cular space. Conversely, administration of a bolus of isooncotic fluids into the circulation of a normo- volemic patient has a reduced plasma volume- expanding effect, with upwards of 60% of the infused volume being shifted into the interstitium.27,103 This increased volume of distribution is proposed to be mediated by hypervolemia-associated damage to the endothelial barrier. Iatrogenic hypervolemia stimulates the release of atrial natriuretic peptide (ANP), a hormone that plays a direct role in endothelial glycocalyx (EG) degradation.27 Accurate determination of intravascular volume status in clinical practice is inherently difficult and not well correlated to macrohemodynamics.104 Approximately 50% of hemodynamically unstable critically ill human patients treated with pragmatic volume loading are nonresponders, meaning there is no increase in cardiac stroke volume after an IV fluid challenge.104 These volume nonresponders are treated with IV fluids without the associated benefit of an improved cardiac output. The seemingly unavoidable “failed” fluid challenge in certain ill patient cohorts, a portion of whom are euvolemic, carries a risk of further compromise to the ESL and accelerated evolution of tissue edema and a positive fluid balance. The revised Starling model and glycocalyx paradigm of transvascular exchange highlights the importance of an intact ESL in the maintenance of transcapillary fluid exchange and provides new insights into the physiology of microvascular fluid flux.52,53 In this revised model, the oncotic pressure differential across the EG layer limits but does not eliminate or reverse fluid movement from the intravascular space to the interstitium. Fluid reabsorption from the interstitium does not occur in the venous capillary bed, but rather the majority of filtered fluid is returned to the vasculature via the lymphatics. A healthy EG is essential to avoid capillary leak and tissue edema formation.52 These features of transcapillary fluid exchange highlight the intrinsic limitations asso- ciated with attempts to impede or correct edema with colloid administration in patients with low capillary hydrostatic pressures or ESL damage.52 With these alterations in place, differences in distributive volume between crystalloids and colloids become less apparent. Safety As more clinical data accrue, a questionable safety profile of synthetic colloidal solutions in critical care has been uncovered. As described in detail previously, HES solutions are associated with clinically significant adverse effects, the most detrimental of which are coagulopathies and AKI. In the VISEP study, patients in the HES arm of the trial had a higher rate of AKI (34.9% versus 22.8%, P = 0.002), increased need for RRT (18.3% versus 9.2%, P = 0.001), lower median platelet count, and received more units of packed red cells.41 In post- hoc univariate analysis, there was a direct correlation between the cumulative dose of HES, the need for RRT, and rate of death at 90 days. Group differences in AKI occurrence and mortality were not evident until greater than 20 days into the study period.41 The findings of this study have been heavily criticized for numerous reasons including the use of a hyperoncotic HES solution, which is considered more likely to cause nephrotic renal tubular lesions and hyperviscosity-mediated AKI. Concerns with the safety profile of tetrastarches have prompted further studies. In the CRYSTMAS study, patients were only administered Voluven for 4 days, a significantly shorter duration than in other studies. Patients received this fluid at standard doses (ࣘ50 mL/kg/d on day 1 and ࣘ25 mL/kg/d on days 2–4), with a lower total dose than reported in the VISEP study.96 Patients in both the tetrastarch and saline groups had comparable kidney function as assessed by risk, injury, failure, loss, end-stage kidney disease (RIFLE) and acute kidney injury network (AKIN) scoring systems. Likewise, there was no evidence of AKI utilizing urinary biomarker analysis. Coagulation parameters were similar between groups and there were no difference in transfusion requirements.96 The number of patients enrolled in this trial was much smaller (196 total) and the short duration of tetrastarch administra- tion may have played a role in the lack of documented adverse effects. Similarly, the CRISTAL trial, a large, randomized trial evaluating the use of isotonic crys- talloids versus any colloid (70% treated with HES) for fluid resuscitation of patients with hypovolemic shock, found no evidence of increased need for RRT between patients in the crystalloid and colloid treatment arm.97 Conversely, the two largest and most influential studies disclosed significant safety concerns with the use of HES in critical illness.42,43 The S6 trial found an increased need for RRT in the HES group (22% versus 16%, P = 0.04) and a positive correlation between RRT 14 C Veterinary Emergency and Critical Care Society 2015, doi: 10.1111/vec.12281
- 10. Crystalloids-colloid controversy and 90-day mortality was found.42 Increased incidence of severe bleeding was also documented in the HES group (10% versus 6%, P = 0.09). In the CHEST trial, there was a statistically significant increased need for RRT in the HES group (7.0% versus 5.8%, P = 0.04), with paradoxically more AKI, based on RIFLE scores, in the saline arm.43 The discrepancy between AKI diagnosis and need for RRT is reconciled by close evaluation of the study findings. Treatment with HES was associated with increased urine output in patients with less severe AKI as compared with similar patients receiving saline. This was postulated to be mediated by increased in- travascular volume or a direct diuretic effect. Despite an increased urine production, patients in the HES group showed consistently higher serum creatinine concen- trations as compared with the saline group. Since urine output is incorporated into the RIFLE scoring system, higher RIFLE injury scores were documented in the saline group despite the greater need for RRT in the HES group.43 Several influential meta-analyses were published in 2013 evaluating the current clinical data on the safety of colloidal fluid resuscitation.81,105–109 A Cochrane review assessed all RCT comparing colloids versus crystalloids for fluid resuscitation in critically ill patients.105 An overall increased risk of AKI, RRT, and kidney failure was found in HES-treated individuals. As described above, this increased risk of AKI with HES persisted despite a paradoxical superior maintenance of urine output. An average of 16 days passed before 50% of pa- tients receiving HES developed AKI, although subgroup analysis demonstrated group differences evolving after only 3 days in certain cohorts. No significant differences were found between septic and nonseptic patients. In addition, specific HES solution formulation (MW, MS, C2/C6) and total HES dose did not impact development of AKI across included studies.105 A second Cochrane review specifically evaluated the effect of HES on kidney function, as compared with any other fluid therapy.106 This is the most complete systematic review of RCTs published on the effects of HES on kidney function. A significant increase in the need for RRT was found in the HES-treated individuals (RR = 1.31). Although the risk of meeting RIFLE-R (risk) criteria for AKI was higher in patients receiving any fluid other than HES, HES-treated individuals were more susceptible to development of more severe RIFLE outcomes.106 No differences in need for RRT and RIFLE-F-based outcomes were seen between sepsis versus nonsepsis patients in subgroup analysis, between high versus low MW and MS HES so- lutions, or based on total volume of HES administered. This study concluded that all HES products increase the risk of AKI and RRT across patient populations and that a safe volume of any HES solution has yet to be determined. An additional influential meta-analysis was published in late 2013 and included RCTs of critically ill adult patients treated in an emergency or ICU setting.81 Pooled results from 10,290 patients involved in 28 trials found, in accordance with other reports, incidence of AKI and need for RRT (reported in a total of 5 trials involving 8,725 patients) were significantly higher (RR = 1.27 and 1.32, respectively) in patients receiving HES.81 These authors concluded that in most clinical situations it is likely that these risks outweigh any benefits, and that alternate volume replacement therapies should be used in place of HES products. Currently, there are no published data confirming an association between HES administration and AKI in the veterinary population. Outcome There has been minimal clinical evidence to date that the incorporation of colloidal solutions into fluid resuscitation algorithms affords a survival advantage. The SAFE trial found no outcome difference between patients randomized to crystalloid versus 4% HSA, concluding that the 2 solutions were equivalent.101 No significant adverse effects associated with colloid administration were identified, refuting the conclusions of a previously published Cochrane review that sug- gested the use of albumin was associated with increased mortality among critically ill patients.110 The Cochrane group incorporated all RCTs on albumin resuscitation, including trials that employed hyperoncotic albumin formulations, which may account for the discrepancy in results. Though the SAFE study was not powered or designed to detect benefits or risks in specific sub- group populations, it suggested a mortality advantage associated with albumin administration in the sepsis cohort.101 The ALBIOS trial later investigated the use of albumin in septic human patients and found albumin administration did not provide a survival advantage or improvement in any measured secondary outcomes.102 Trials comparing resuscitation with crystalloids to synthetic colloids have had somewhat disparate results. In the S6 trial, an increased risk of death at day 90 in the HES group as compared with the Ringer’s acetate group was demonstrated (51% versus 43%, P = 0.03).72 Diver- gence of Kaplan-Meier survival curves did not begin to evolve between groups until close to 20 days poststudy enrollment. The CHEST trial failed to demonstrate a difference in 90-day mortality between crystalloid and HES-resuscitated individuals, the primary endpoint of the trial.43 The crystalloid versus colloid Cochrane re- view found no evidence that resuscitation with colloids reduces the risk of death when compared with crystal- loid resuscitation and suggested that the use of HES in particular may increase the risk of death.105 However, C Veterinary Emergency and Critical Care Society 2015, doi: 10.1111/vec.12281 15
- 11. D. Cazzolli J. Prittie the aforementioned meta-analysis demonstrated HES was significantly associated with increased risk of death (R = 1.09).81 In contrast, in the CRISTAL trial, while no difference in primary outcome of 28-day mortality was found between patients resuscitated with crystalloid versus colloid, there were fewer deaths at 90 days in the colloid arm (30.7% versus 34.2%, P = 0.03).97 Approximately 70% of the 1,414 patients in the colloid cohort were treated with HES. The results of this trial are in contrast to the previously discussed major trials and possible explanations include tight control over daily colloid dose limits; colloid-associated reduction in cardiovas- cular and respiratory failures that may have inferred renal protection (by way of less need for vasopressor therapies); and use of chloride-rich solutions (saline) in a majority of patients in the crystalloid arm. Compared to the previously discussed RCTs, the CRISTAL trial had a less rigorous design with some overlap in colloidal types administered to each patient, making conclusions refer- able to a particular colloid type inherently challenging. Resuscitation with colloidal solutions in lieu of a purely crystalloid-driven regimen in the setting of severe illness has not demonstrated a survival advantage. The reported adverse effects associated with HES have been compelling enough to prompt the current Surviving Sepsis Campaign Guidelines to recommend against the use of HES for fluid resuscitation of severe sepsis and septic shock (grade 1B).55 They instead suggest the incorporation of HSA in the fluid resuscitation plan of patients with severe sepsis and septic shock when substantial amounts of crystalloids are required (grade 2C).55 In addition, the use of HES solutions has been banned from use in the European market.54 In spite of these studies, HES solutions are still used with frequency in human and veterinary medicine in the United States. Veterinary Implications Despite the recent surge in clinical data in the field of human critical care, minimal safety and efficacy data exist in veterinary medicine regarding the use of HES as a resuscitation fluid. The large-scale veterinary clinical trials required to establish an influence of HES resusci- tation on patient outcome and adverse effects are likely not logistically feasible in the near future. Veterinary studies are often not powered to detect mortality differ- ences in a diverse patient population with a myriad of underlying comorbidities. Caution must be used when extrapolating human data and associated conclusions to veterinary patient populations given several patient and population-dependent factors, which confer an inherent risk of error. Human and veterinary ICU patients are two distinctly different patient populations. It is unknown whether the data from critically ill human patients are representative of a risk that spans across species and are applicable to all patient populations. Overall illness severity in veterinary ICU patients is far less than in their human counterparts, attributable to the impact of veterinary client financial constraints and the ability to elect for humane euthanasia in severe disease states. A majority of the aforementioned human clinical trials evaluating the use of HES as a resuscitation fluid enrolled patients who were diagnosed with severe sepsis or septic shock, on aggressive vasopressor therapy and often reliant on mechanical ventilation.41–44 In veterinary medicine, sepsis is not treated with nearly the same fre- quency, nor is illness severity within this patient popula- tion comparable to that of human patients. Although this severely ill cohort represents a percentage of veterinary ICU patients, it does not represent the population as a whole. Moreover, a large disparity exists in the duration of hospitalization between patient populations. Criti- cally ill human patients commonly have hospitalizations that are on the order of weeks to months, whereas aver- age veterinary ICU hospitalizations are days in duration. Accordingly, the total administered volume of most re- suscitation fluids is far less in veterinary patients, owing to the significantly shorter mean duration of hospital- ization in conjunction with lower illness severity and perceived global volume deficits. The HES-associated adverse effects of AKI and mortality have been noted to be dose- and time-dependent in some trials. Hydroxy- ethyl starch-associated AKI typically becomes evident 5–20 days after ICU admission.106 The abbreviated hospi- talization in veterinary patients may mitigate the risk of HES toxicity. Patients in the CRYSTMAS trial who were treated with HES for only 4 days did not develop a HES- associated AKI that other large trials, with longer dura- tions of treatment and total administered volumes, have reported.96 Conversely, some subgroup analyses have shown renal impairment within 3 days in high-risk pa- tient populations, which may represent a differentiated risk for the more severely ill cohorts discussed above.106 Of importance is the absence of validated alternate means of provision of intravascular oncotic support to veterinary patients. As outlined earlier, a species- specific, readily available, cost effective natural colloid solution does not currently exist. With the known morbidity associated with large volume crystalloid administration and positive net fluid balance, there is a drive to provide resuscitation that may limit these effects. Adjunct colloidal support is often required to adequately resuscitate a patient with substantial circula- tory failure and achieve normalization of hemodynamic parameters without causing a net positive fluid balance. The results of the CRISTAL and CRYSTMAS trials are intriguing and may be more pragmatic and applicable 16 C Veterinary Emergency and Critical Care Society 2015, doi: 10.1111/vec.12281
- 12. Crystalloids-colloid controversy to veterinary ICU patients, as these trials focused on hypovolemic patients with severe volume deficits requiring rapid correction and short duration HES use.96,97 Careful analysis of the current data also sug- gests that veterinary patients may not be as susceptible to or at risk for the adverse effects documented in human patients. A judicious, thoughtful use of HES in veterinary patients is merited, with astute consideration of the potential side effects, as is prudent with the use of any drug in the intensive care setting. Adherence to manufacturer recommended daily dosing is advocated, with consideration of earlier use of vasopressors and inotrope therapy in the treatment of circulatory failure once initial fluid resuscitation has failed. There is compelling evidence supporting avoidance of use of HES solutions in certain human patient populations, including patients with known renal dysfunction and patients with sepsis, systemic inflammation or suspected severe capillary leak and third spacing. The application of these restrictions to veterinary patients may not be justified at the present time; however, as mentioned previously, safety evaluations have not been performed. In addition, although the potential toxicities associated with synthetic colloids are widely acknowledged in human critical care, the potential benefit in hypovolemic resuscitation remains an unsettled dispute. Veterinary clinical data evaluating the effect of synthetic colloid fluid resuscitation on incidence of adverse effects and patient outcome are lacking and warranted. References 1. Rivers E, Nguyen B, Havstad S, et al. Early goal-directed therapy in the treatment of severe sepsis and septic shock. N Engl J Med 2001; 345(19):1368–1377. 2. Prittie J. Optimal endpoints of resuscitation and early goal-directed therapy. J Vet Emerg Crit Care 2006; 16(4):329–339. 3. Myburgh JA, Mythen MG. Resuscitation fluids. N Engl J Med 2013; 369(13):1243–1251. 4. Santry HP, Alam HB. Fluid resuscitation: past, present and future. Shock 2010; 33(3):229–241. 5. Cotton BA, Guy JS, Morris JA, et al. The cellular, metabolic and systemic consequences of aggressive fluid resuscitation strategies. Shock 2006; 26(2):115–121. 6. Casrto VJ, Astiz ME, Rackow EC. Effect of crystalloid and colloid solutions on blood rheology in sepsis. Shock 1997; 8(2):104–107. 7. Neff TA, Fischler L, Mark M, et al. The influence of two different hydroxyethyl starch solutions (6% HES 130/0.4 and 200/0.5) on blood viscosity. Anesth Analg 2005; 100(6):1773–1780. 8. Hartog CS, Bauer M, Reinhart K. The efficacy and safety of colloid resuscitation in the critically ill. Anesth Analg 2011; 112(1):156–164. 9. Kruer RM, Ensor CR. Colloids in the intensive care unit. Am J Health-Syst Pharm 2012; 69(19):1635–1642. 10. Raghunathan K, Shaw AD, Bagshaw SM. Fluids are drugs: type, dose and toxicity. Curr Opin Crit Care 2013; 19(4):290–298. 11. Yunos NM, Kim IB, Bellomo R, et al. The biochemical effects of restricting chloride-rich fluids in intensive care. Crit Care Med 2011; 39(11):2419–2424. 12. Shaw AD, Bagshaw SM, Goldstein SL, et al. Major complications, mortality, and resource utilization after open abdominal surgery: 0.9% saline compared to Plasma-Lyte. Ann Surg 2012; 255(5):821– 829. 13. Yunos NM, Bellomo R, Hegarty C, et al. Association between a chloride-liberal vs chloride-restrictive intravenous fluid adminis- tration strategy and kidney injury in critically ill adults. J Am Med Assoc 2012; 308(15):1566–1572. 14. Raghunathan K, Shaw A, Nathanson B, et al. Association be- tween the choice of IV crystalloid and in-hospital mortality among critically ill adults with sepsis. Crit Care Med 2014; 42(7):1585– 1591. 15. Lowell JA, Schifferdecker C, Driscoll DF, et al. Postoperative fluid overload: not a benign problem. Crit Care Med 1990; 18(7):728–733. 16. Vaara ST, Korhonen AM, Kaukonen KM, et al. Fluid overload is associated with an increased risk for 90-day mortality in critically ill patients with renal replacement therapy: data from the prospective FINNAKI study. Crit Care 2012; 16(5):R197. 17. Payen D, de Pont AC, Sakr Y, et al. Sepsis Occurrence in Acutely Ill Patients (SOAP) Investigators. A positive fluid balance is asso- ciated with a worse outcome in patients with acute renal failure. Crit Care 2008; 12(3):R74. 18. Arikan AA, Zappitelli M, Goldstein SL, et al. Fluid overload is associated with impaired oxygenation and morbidity in critically ill children. Pediatr Crit Care Med 2012; 13(3):253–258. 19. Flori HR, Church G, Liu KD, et al. Positive fluid balance is associ- ated with higher mortality and prolonged mechanical ventilation in pediatric patients with acute lung injury. Crit Care Res Pract 2011; 2011:854142. 20. Boyd JH, Forbes J, Nakada TA, et al. Fluid resuscitation in septic shock: a positive fluid balance and elevated central venous pres- sure are associated with increased mortality. Crit Care Med 2011; 39(2):259–265. 21. Bagshaw SM, Brophy PD, Cruz D, et al. Fluid balance as a biomarker: impact of fluid overload on outcome in critically ill patients with acute kidney injury. Crit Care 2008; 12(4):169–171. 22. Sakr Y, Vincent JL, Reinhart K, et al. Sepsis Occurence in Acutely Ill Patients Investigators. High tidal volume and positive fluid bal- ance are associated with worse outcome in acute lung injury. Chest 2005; 128(5):3098–3108. 23. Sadaka F, Juarez M, Naydenov S, et al. Fluid resuscitation in septic shock: the effect of increasing fluid balance on mortality. J Intensive Care Med 2014; 29(4):213–217. 24. Shim HJ, Jang JY, Lee SH, et al. The effect of positive balance on the outcomes of critically ill noncardiac postsurgical patients: a retrospective cohort study. J Crit Care 2014; 29(1):43–48. 25. Abulebda K, Cvijanovich NZ, Thomas NJ, et al. Post-ICU admis- sion fluid balance and pediatric septic shock outcomes: a risk- stratified analysis. Crit Care Med 2014; 42(2):397–403. 26. Mobley A, Sullivan L. Retrospective determination of fluid over- load in critically ill dogs (Abstr). J Vet Emer Crit Care 2012; 22(S2):S8 27. Chappell D, Jacob M, Hofmann-Kiefer K, et al. A rational ap- proach to perioperative fluid management. Anesthesiology 2008; 109(4):732–740. 28. Mazzaferro EM, Rudloff E, Kirby R. The role of albumin replace- ment in the critically ill veterinary patient. J Vet Emerg Crit Care 2002; 12(2):113–124. 29. Mathews KA, Barry M. The use of 25% human serum albumin: outcome and efficacy in raisin serum albumin and systemic blood pressure in critically ill dogs and cats. J Vet Emerg Crit Care 2005; 15(2):110–118. 30. Trow AV, Rozanski EA, deLaforcade AM, et al. Evaluation of the use of human albumin in critically ill dogs: 73 cases (2003–2006). J Am Vet Med Assoc 2008; 233(4):607–612. 31. Vigano F, Perissinotto L, Bosco VRF. Administration of 5% human serum albumin in critically ill small animal patients with hypoal- buminemia: 418 dogs and 170 cats (199–2008). J Vet Emerg Crit Care 2010; 20(2):237–243. 32. Francis AH, Martin LG, Haldorson GJ, et al. Adverse reactions suggestive of type III hypersensitivity in six healthy dogs given human albumin. J Am Vet Med Assoc 2007; 230(6):873–879. 33. Cohn LA, Kerl ME, Lenox CE, et al. Response of healthy dogs to infusions of human serum albumin. Am J Vet Res 2007; 68(6):657– 663. C Veterinary Emergency and Critical Care Society 2015, doi: 10.1111/vec.12281 17
- 13. D. Cazzolli J. Prittie 34. Martin LG, Luther TY, Alperin DC, et al. Serum antibodies against human albumin in critically ill and healthy dogs. J Am Vet Med Assoc 2008; 232(7):1004–1009. 35. Powell C, Thompson L, Murtaugh RJ. Type III hypersensitivity reaction with immune complex deposition in 2 critically ill dogs administered human serum albumin. J Vet Emerg Crit Care 2013; 23(6):598–604. 36. Craft EM, Powell LL. The use of canine-specific albumin in dogs with septic peritonitis. J Vet Emerg Crit Care 2012; 22(6):631–639. 37. Tocci LJ. Transfusion medicine in small animal practice. Vet Clin North Am Small Anim Pract 2010; 40(3):485–494. 38. Theusinger OM, Madjdpour C, Spahn DR. Resuscitation and trans- fusion management in trauma patients: emerging concepts. Curr Opin Crit Care 2012; 18(6):661–670. 39. Downar J, Lapinsky SE. Pro/con debate: should synthetic colloids be used in patients with septic shock? Crit Care 2009; 13(1):203–207. 40. Westphal M, James MF, Kozek-Langenecker S, et al. Hydroxyethyl starches: different products—different effects. Anesthesiol 2009; 111(1):187–202. 41. Brunkhorst FM, Engel C, Bloos F, et al. Intensive insulin therapy and pentastarch resuscitation in severe sepsis. N Engl J Med 2008; 358(2):125–139. 42. Perner A, Haase N, Guttormsen AB, et al. Hydroxyethyl starch 130/0.42 versus Ringer’s acetate in severe sepsis. N Engl J Med 2012; 367(2):124–134. 43. Myburgh JA, Finfer S, Bellomo R, et al. Hydroxyethyl starch or saline for fluid resuscitation in intensive care. N Engl J Med 2012; 367(20):1901–1911. 44. Haase N. Hydroxyethyl starch in sepsis. Dan Med J 2014; 61:B4764. 45. Boldt J. Modern rapidly degradable hydroxyethyl starches: current concepts. Anesth Analg 2009; 108(5):1574–82. 46. Trieb J, Haass G, Pindur MT, et al. All medium starches are not the same: influence of degree of hydroxyethyl subsitution of hydroxy- ethyl starch on plasma volume, hemorrheologic conditions, and coagulation. Transfusion 1996; 36:450–455. 47. Jungheinrich C. The starch family: are they all equal? Pharmacoki- netics and pharmacodynamics of hydroxyethyl starches. Transfus Altern Transfus Med 2007; 9:152–163. 48. Schortgen F, Girou E, Deye N, et al. The risk associated with hyper- oncotic colloids in patients with shock. Intensive Care Med 2008; 34:2157–2168. 49. Yacobi A, Gibson TP, McEntegart CM, et al. Pharmacokinetics of high molecular weight hydroxyethyl starch in dogs. Res Commun Chem Pathol Pharmacol 1982; 36(2):199–204. 50. Kozek-Langenecker SA. Effects of hydroxyethyl starch solutions on hemostasis. Anesth 2005; 103(3):654–660. 51. Zhi-Yong P, Kellum JA. Perioperative fluids: a clear road ahead. Curr Opin Crit Care 2013; 19:353–358. 52. Woodcock TE, Woodcock TM. Revised Starling equation and the glycocalyx model of transvascular fluid exchange: an improved paradigm for prescribing intravenous fluid therapy. Br J Anaesth 2012; 108(3):384–394. 53. Levick JR, Michel CC. Microvascular fluid exchange and the re- vised Starling principle. Cardiovac Res 2010; 87(2):198–210. 54. Reinhart K, Perner A, Sprung CL, et al. Consensus statement of the ESICM task force on colloid volume therapy in critically ill patients. Intensive Care Med 2012; 38(3):368–383. 55. Dellinger RP, Levy MM, Rhodes A, et al. Surviving Sepsis Cam- paign: International Guidelines for Management of Severe Sepsis and Septic Shock: 2012. Crit Care Med 2013; 41(2):580–637. 56. Schramko A, Suojaranta-Ylinen R, Kuitunen A, et al. Hydroxy- ethylstarch and gelatin solutions impair blood coagulation after cardiac surgery: a prospective randomized trial. Br J Anaesth 2010; 104(6):691–697. 57. Haase N, Wetterslev J, Winkel P, et al. Bleeding and risk of death with hydroxyethyl starch in severe sepsis: post hoc analyses of a randomized clinical trial. Intensive Care Med 2013; 39(12):2126– 2134. 58. Skhirtladze K, Base EM, Lassnigg A, et al. Comparison of the ef- fects of albumin 5%, hydroxyethyl starch 130/0.4 6%, and Ringer’s acetate on blood loss and coagulation after cardiac surgery. Br J of Anesth 2014; 112(2):255–564. 59. Rasmussen KC, Johansson PI, Hojskov M, et al. Hydroxyethyl starch reduces coagulation competence and increases blood loss during major surgery. Ann Surg 2014; 259(2):249–254. 60. Haase N, Wetterselv J, Winkel P, Perner A, on behalf of the 6S trial group and the Scandanavian Critical Care Trial Group. Bleeding and the risk of death with hydroxyethyl starch in severe sepsis— post-hoc analyses of a randomized clinical trial. Intensive Care Med 2013; 39(12):2126–2134. 61. Haase N, Perner A, Hennings LI, et al. Hydroxyethyl starch 130/0.38–0.45 verses crystalloid or albumin in patients with sepsis: systematic review with meta-analysis and trial sequential analysis. BMJ 2013; 346:f839. 62. de Jonge E, Levi M. Effects of different plasma substitutes on blood coagulation: a comparative review. Crit Care Med 2001; 29(6):1261– 1267. 63. Sossdorf M, Marx S, Schaarschmidt B, et al. HES 130/0.4 impairs haemostasis and stimulates pro-inflammatory blood platelet func- tion. Crit Care 2009; 13(6):R208. 64. Hartog CS, Reuter D, Loesche W, et al. Influence of hydroxyethyl starch (HES) 130/0.4 on hemostasis as measured by visoelastic device analysis: a systematic review. Intensive Care Med 2011; 37(11):1725–1737. 65. Smart L, Kass PH, Wierenga JR, et al. The effect of hetastarch (670/0.75) in vivo on platelet closure time in the dog. J Vet Emerg Crit Care 2009; 19(5):444–449. 66. Blong AE, Epstein KL, Brainard BM. In vitro effects of three for- mulations of hydroxyethyl starch solutions on coagulation and platelet function in horses. Am J Vet Res 2013; 74(5):712–20. 67. Classen J, Adamik KN, Weber K, et al. In vitro effect of hydroxy- ethyl starch 130/0.42 on canine platelet function. Am J Vet Res 2012; 73(12):1908–1912. 68. Wierenga JR, Jandrey KE, Haskins SC, et al. In vitro comparison of the effects of two forms of hydroxyethyl starch solutions on platelet function in dogs. Am J Vet Res 2007; 68(6):605–609. 69. Epstein KL, Bergren A, Giguère S, et al. Cardiovascular, colloid osmotic pressure, and hemostatic effects of 2 formulations of hy- droxyethyl starch in healthy horses. J Vet Intern Med 2014; 28(1): 223–233. 70. McBride D, Hosgood GL, Mansfield CS, et al. Effect of hydroxy- ethyl starch 130/0.4 and 200/0.5 solutions on canine platelet func- tion in vitro. Am J Vet Res 2013; 74(8):1133–1137. 71. Fenger-Eriksen C, Tonnesen E, Ingerslev J, et al. Mechanisms of hydroxyethyl starch-induced dilutional coagulopathy. J Thromb Haemost 2009; 7(7):1099–1105. 72. Helmbold KA, Mellema MS, Hopper K, et al. The effect of het- astarch 670/0.75 administered in vivo as a constant rate infusion on platelet closure time in the dog. J Vet Emerg Crit Care 2014; 24(4):381–387. 73. Madjdpour C, Dettori N, Frascarolo P, et al. Molecular weight of hydroxyethyl starch: is there an effect on blood coagulation and pharmacokinetics? Br J Anaesth 2005; 94(5):569–576. 74. Viljoen A, Page PC, Fosgate GT, et al. Coagulation, oncotic and haemodilutional effects of a third generation hydroxyethyl starch (130/0.4) solution in horses. Equine Vet J 2014; 46(6):739– 744. 75. Falco S, Bruno B, Bellino C, et al. In vitro evaluation of canine hemostasis following dilution with hydroxyethyl starch (130/0.4) via thromboelastometry. J Vet Emerg Crit Care 2012; 22(6):640–645. 76. Chohan AS, Greene SA, Grubb TL, et al. Effects of 6% hetastarch (600/0.75) or lactated Ringer’s solution on hemostatic variables and clinical bleeding in healthy dogs anesthetized for orthopedic surgery. Vet Anaesth Analg 2011; 38(2):94–105. 77. Groeneveld AB, Navickis RJ, Wilkes MM. Update on the compara- tive safety of colloids: a systematic review of clinical studies. Ann Surg 2011; 253(3):470–483. 78. Hartog CS, Welte T, Schlarrmann P, et al. Fluid replacement with hydroxyethyl starch in critical care—a reassessment. Dtsch Arztebl Int 2013; 110:443–450. 79. Schabinski F, Oishi J, Tuche F, et al. Effects of a predominantly hydroxyethyl starch (HES)-based and a predominantly non-HES- based fluid therapy on renal function in surgical ICU patients. Intensive Care Med 2009; 35:1539–1547. 18 C Veterinary Emergency and Critical Care Society 2015, doi: 10.1111/vec.12281
- 14. Crystalloids-colloid controversy 80. Schortgen F, Lacherade JC, Bruneel F, et al. Effects of hydroxyethyl- starch and gelatin on renal function in severe sepsis: a multicentre randomized study. Lancet 2001; 357(9260):911–916. 81. Zarychanski R, Abou-Setta AM, Turgeon AF, et al. Association of hydroxyethyl starch administration with mortality and acute kid- ney injury in critically ill patients requiring volume resuscitation: a systematic review and meta-analysis. J Am Med Assoc 2013; 309(7):678–688. 82. Martin C, Jacob M, Vicaut E, et al. Effect of waxy maize-derived hydroxyethyl starch 130/0.4 on renal function in surgical patients. Anesthesiol 2013; 118(2):387–394. 83. Sakr Y, Payen D, Reinhart K, et al. Effects of hydroxyethyl starch ad- ministration on renal function in critically ill patients. Br J Anaesth 2007; 98(2):216–224. 84. Lissauer ME, Chi A, Kramer ME, et al. Association of 6% het- astarch resuscitation with adverse outcomes in critically ill trauma patients. Am J of Surg 2011; 202(1):53–58. 85. Schortgen F, Brochard L. Colloid-induced kidney injury: experi- mental evidence may help to understand mechanisms. Crit Care 2009; 13(2):130–131. 86. Siegemund M. 10% Hydroxyethylstarch impairs renal function and induces interstitial proliferation, macrophage infiltration and tubu- lar damage. Crit Care 2009; 13(4):413–414. 87. Huter L, Simon TP, Weinman L, et al. Hydroxyethylstarch impairs renal function and induces interstitial proliferation, macrophage infiltration, and tubular damage in an isolated renal perfusion model. Crit Care 2009; 13(1):R23. 88. Simon TP, Schuerholz T, Huter L, et al. Impairment of renal func- tion using hyperoncotic colloids in a two hit model of shock: a prospective randomized study. Crit Care 2012; 16(1):R16. 89. Dickenmann M, Oetti T, Mihatsch MJ. Osmotic nephrosis: acute kidney injury with accumulation of proximal tubular lysosomes due to administration of exogenous solutes. Am J Kidney Dis 2008; 51(3):491–503. 90. Wiedermann CJ, Joannidis M. Accumulation of hydroxyethyl starch in human and animal tissues: a systematic review. Inten- sive Care Med. 2014; 40(2):160–170. 91. Bellmann R, Feistritzer C, Wiedermann CJ. Effect of molecu- lar weight and substitution on tissue uptake of hydroxyethyl starch: a meta-analysis of clinical studies. Clin Pharmacokinet 2012; 51(4):225–236. 92. Sirtl C, Laubenthal H, Zumtobel V, et al. Tissue deposits of hy- droxyethyl starch (HES): dose-dependent and time-related. Br J Anaesth 1999; 82(4):510–515. 93. Ständer S, Richter L, Osada N, et al. Hydroxyethyl starch-induced pruritus: clinical characteristics and influence of dose, molecu- lar weight and substitution. Acta Derm Venereol 2014; 94(3):282– 287. 94. Bork K. Pruritis precipitated by hydroxyethyl starch: a review. Br J Dermatol 2005;152(1):3–12. 95. Wittbrodt P, Haase N, Butowska D, et al, the 6S trial group and the Scandinavian Critical Care Trials Group. Quality of life and pruritus in patients with severe sepsis resuscitated with hydroxy- ethyl starch long-term follow-up of a randomized trial. Crit Care 2013;17(2):R58. 96. Guidet B, Martinet O, Boulain T, et al. Assessment of hemodynamic efficacy and safety of 6% hydroxyethylstarch 130/0.4 vs 0.9% NaCl fluid replacement in patients with severe sepsis: the CRYSTMAS study. Crit Care 2012; 16(3):R94. 97. Annane D, Siami S, Jaber S, et al. Effects of fluid resuscitation with colloids vs crystalloids on mortality in critically ill patients pre- senting with hypovolemic shock: the CRISTAL randomized trial. J Am Med Assoc 2013; 310(17):1809–1817. 98. Shoemaker WC, Schluchter M, Hopins JA, et al. Comparison of the relative effectiveness of colloids and crystalloids in emergency resuscitation. Am J Surg 1981; 142(5):73–84. 99. Silverstein DC, Aldrich J, Haskins SC, et al. Assessment of changes in blood volume in response to resuscitative fluid administration in dogs. J Vet Emerg Crit Care 2005; 15(3):185–192. 100. Gauthier V, Holowaychuk MK, Kerr CL, et al. Effect of synthetic colloid administration on hemodynamic and laboratory variables in healthy dogs and dogs with systemic inflammation. J Vet Emerg Crit Care 2014; 24(3):251–258. 101. SAFE Study Investigators. A comparison of albumin and saline for fluid resuscitation in the intensive care unit. N Engl J Med 2004; 350(22):2247–2256. 102. Caironi P, Tognoni G, Masson S, et al. Albumin replacement in patients with severe sepsis or septic shock. N Engl J Med 2014; 370(15):1412–1421. 103. Chappell D, Jacob M. Hydroxyethyl starch—the importance of be- ing earnest. Scand J Trauma Resusc Emerg Med 2013; 21(1):61–64. 104. Marik PE, Monnet X, Tebou JL. Hemodynamic parameters to guide fluid therapy. Ann Intensive Care 2011; 1(1):1–9. 105. Perel P, Roberts I, Ker K. Colloids versus crystalloids for fluid resuscitation in critically ill patients. Cochrane Database Syst Rev 2013: CD000567. 106. Mutter TC, Ruth CA, Dart AB. Hydroxyethyl starch (HES) verses other fluid therapies: effects on kidney function. Cochrane Database Syst Rev 2013: CD007594. 107. Gattas DJ, Dan A, Myburgh J, et al. Fluid resuscitation with 6% hydroxyethyl starch (130/0.4) in acutely ill patients: an updated systematic review and meta-analysis. Anesth Analg 2012; 114:159– 169. 108. Patel A, Waheed U, Brett SJ. Randomized trials of 6% tetrastarch (hydroxyethyl starch 130/0.4 or 0.42) for severe sepsis reporting mortality: systematic review and meta-analysis. Intensive Care Med 2013; 39:811–822. 109. Gattas DJ, Dan A, Myburgh J, et al. Fluid resuscitation with 6% hydroxyethyl starch (130/0.4 and 130/0.42) in acutely ill patients: systematic review of effects on mortality and treatment with renal replacement therapy. Intensive Care Med 2013; 39:558–568. 110. Cochrane Injuries Group Albumin Reviewers. Human albumin administration in critically ill patients: systematic review of ran- domized controlled trials. BMJ 1998; 317(7153):235–240. C Veterinary Emergency and Critical Care Society 2015, doi: 10.1111/vec.12281 19