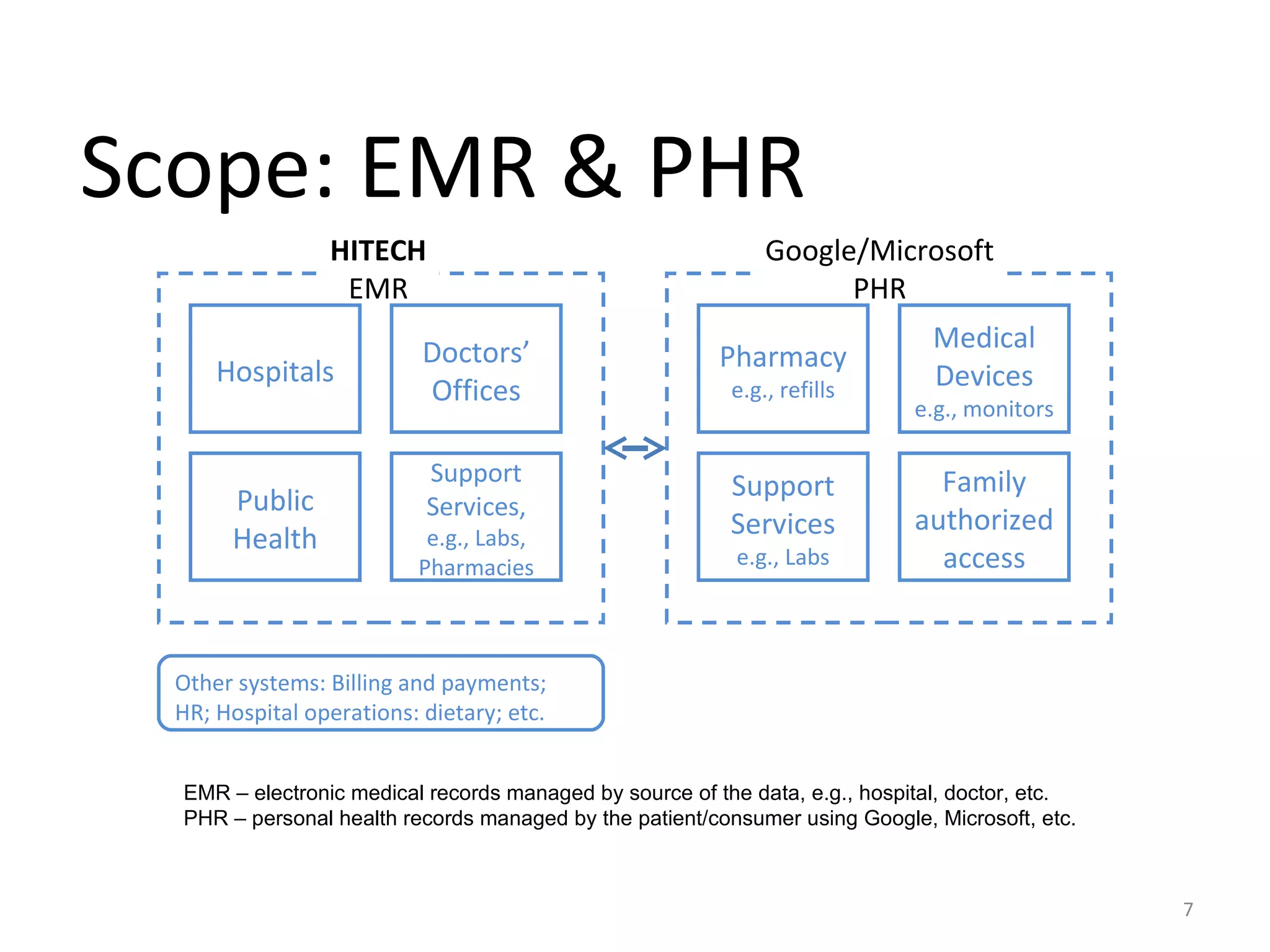
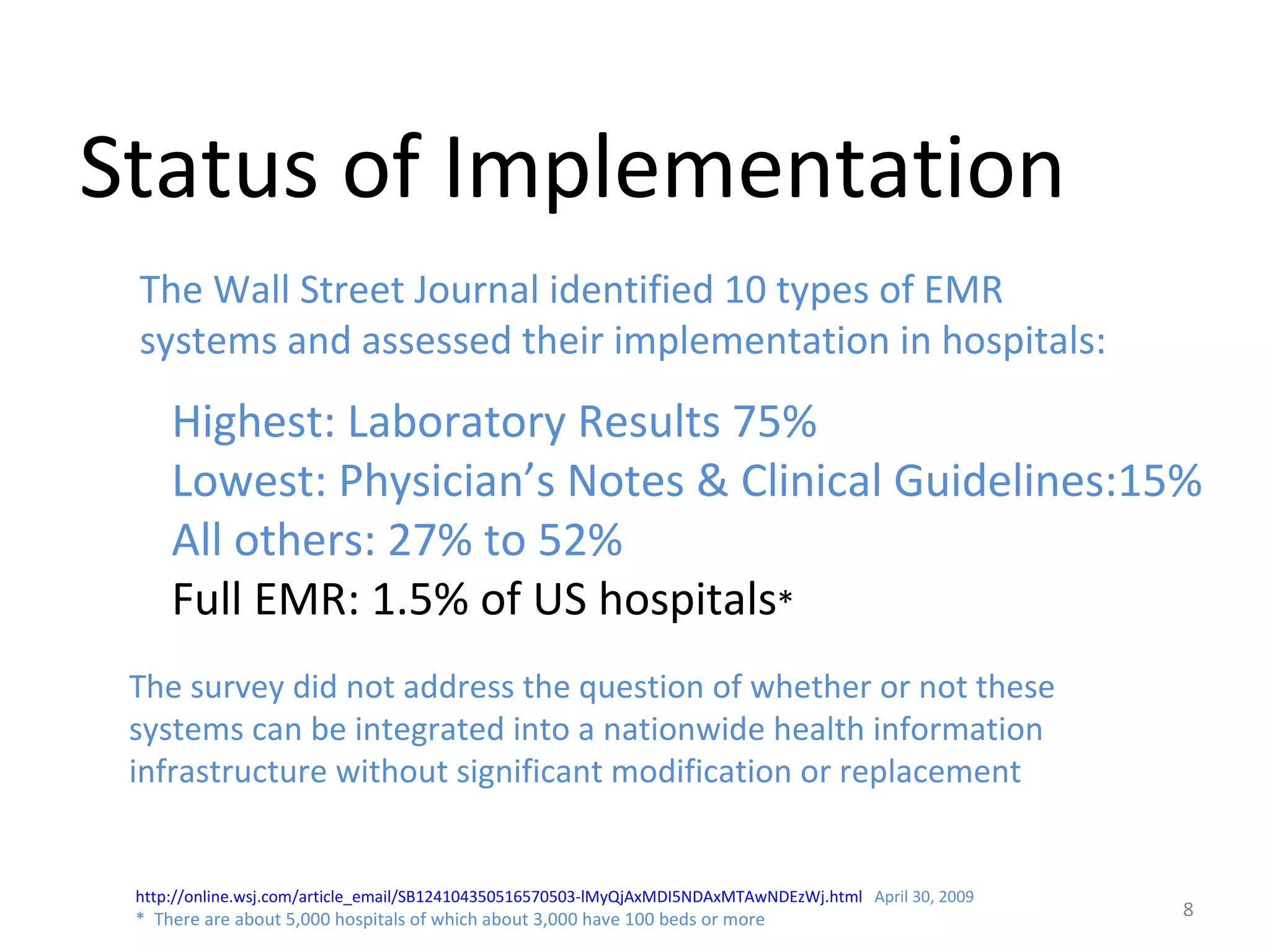
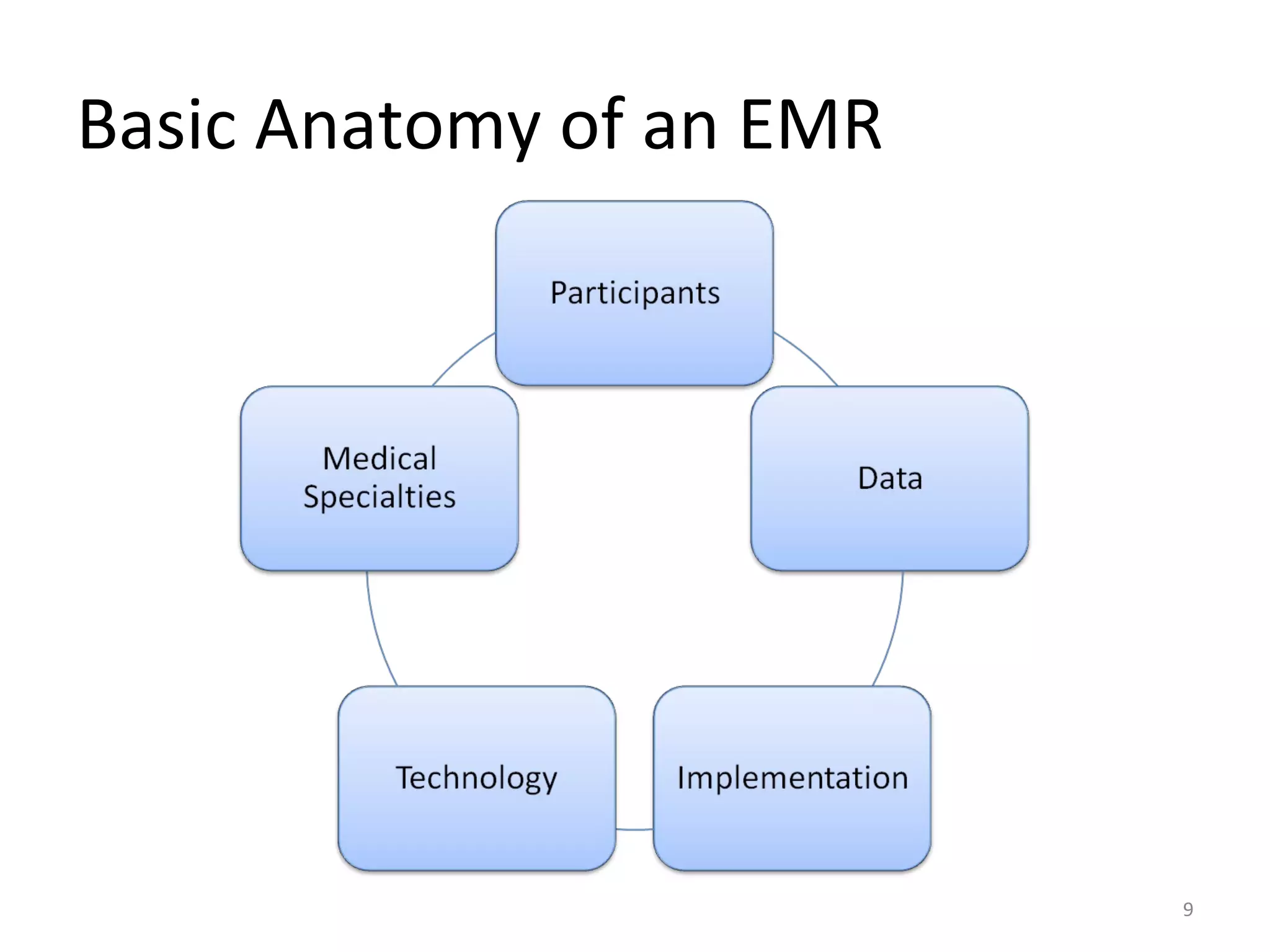
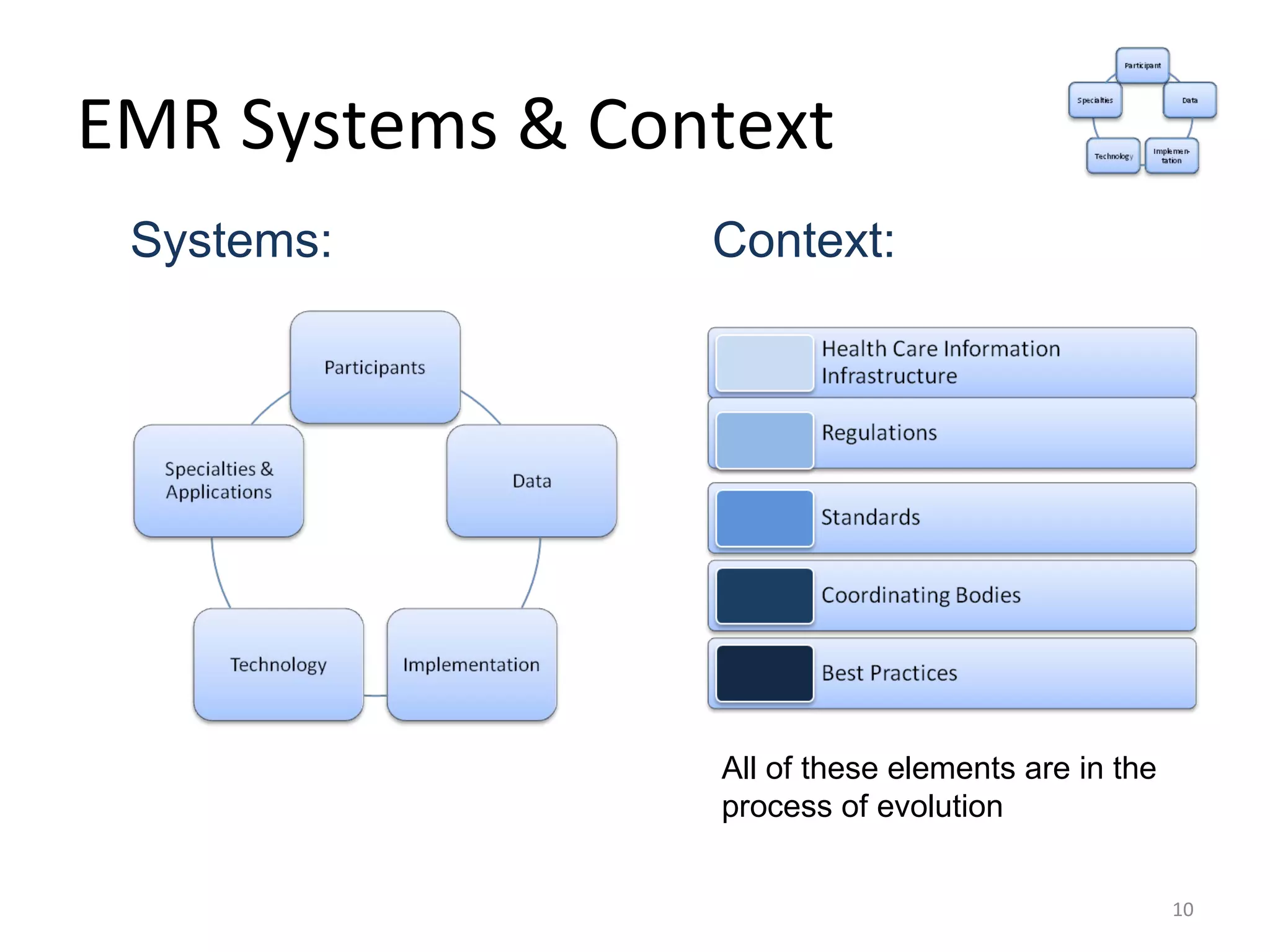
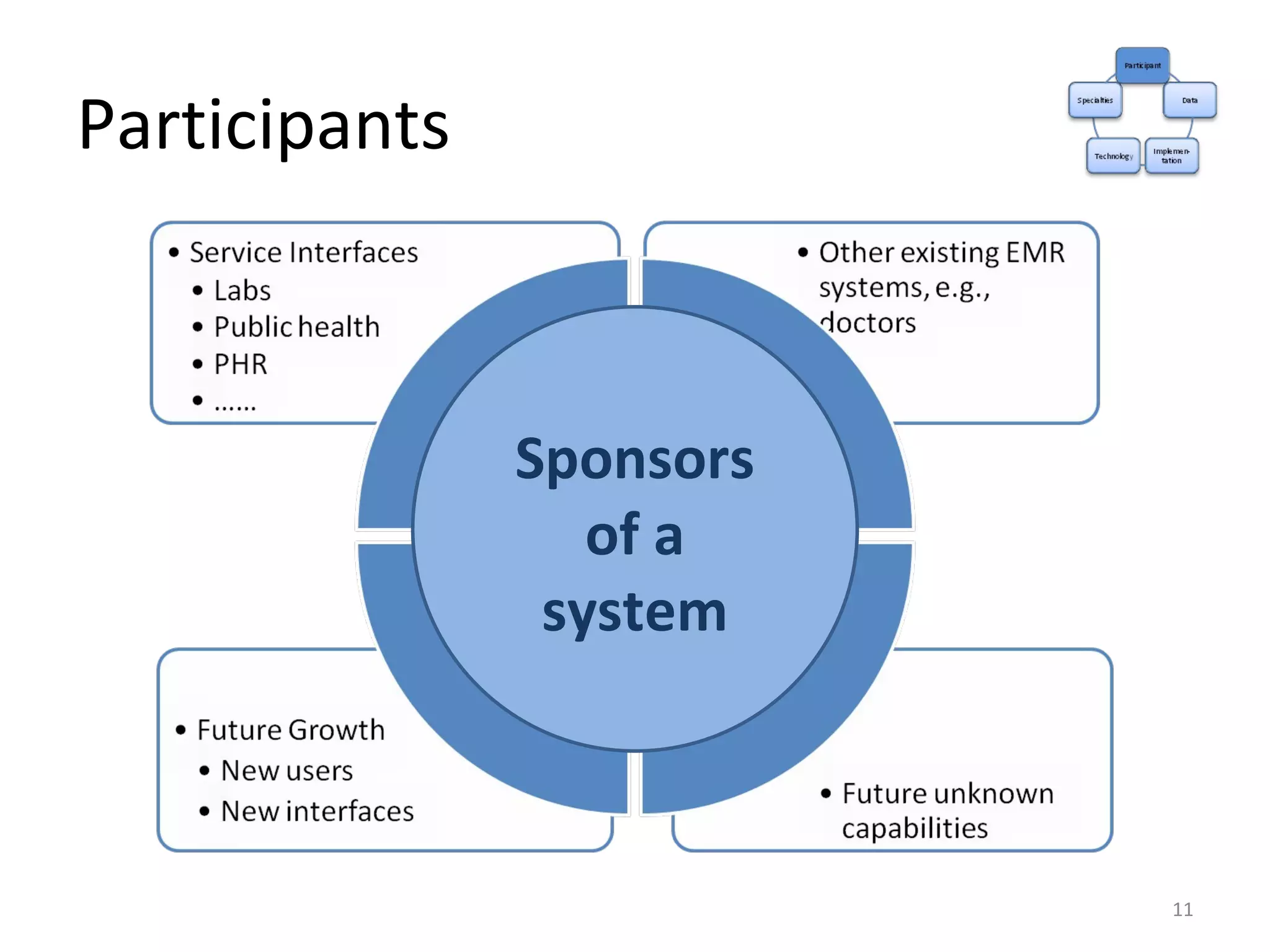
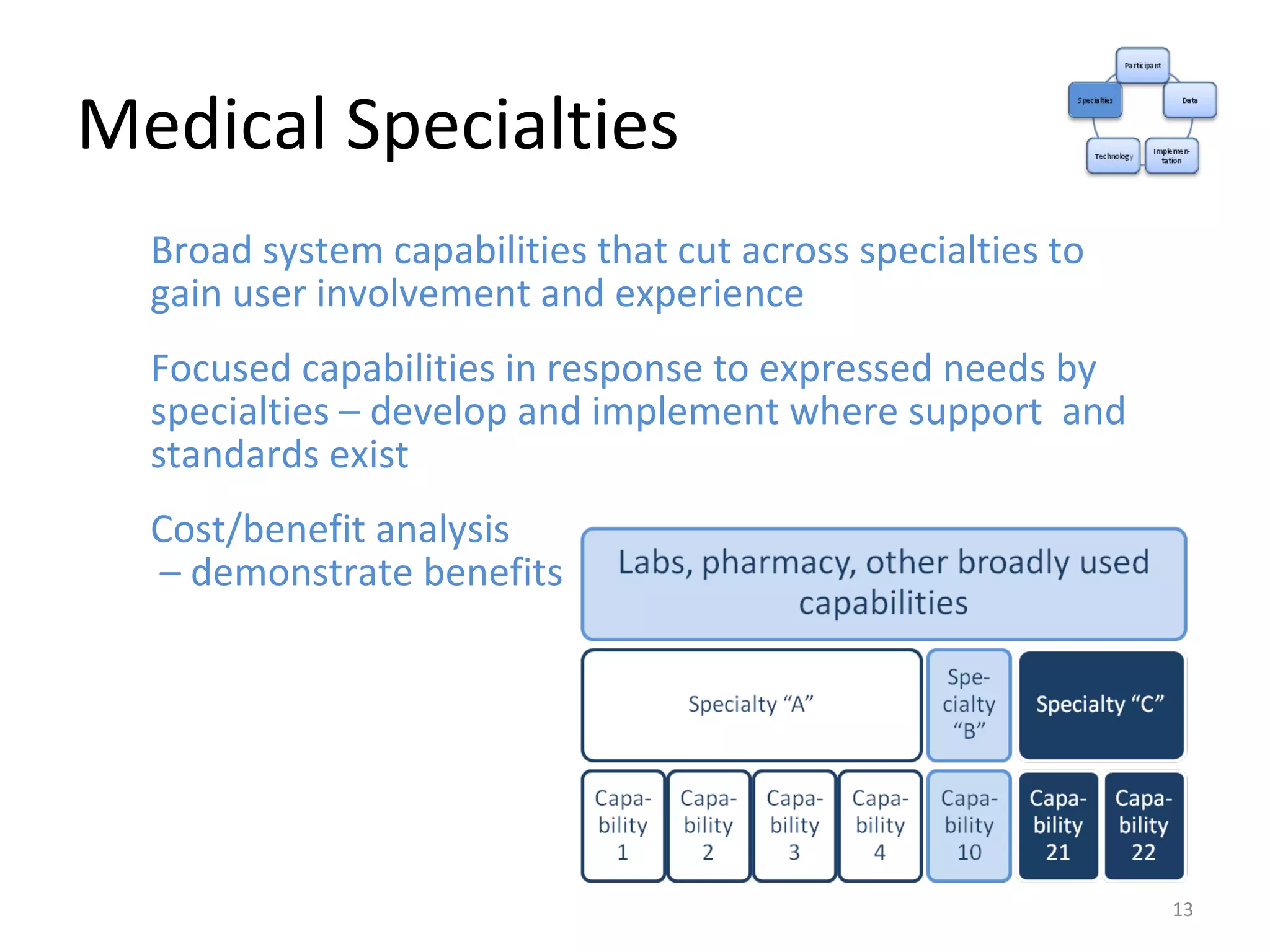
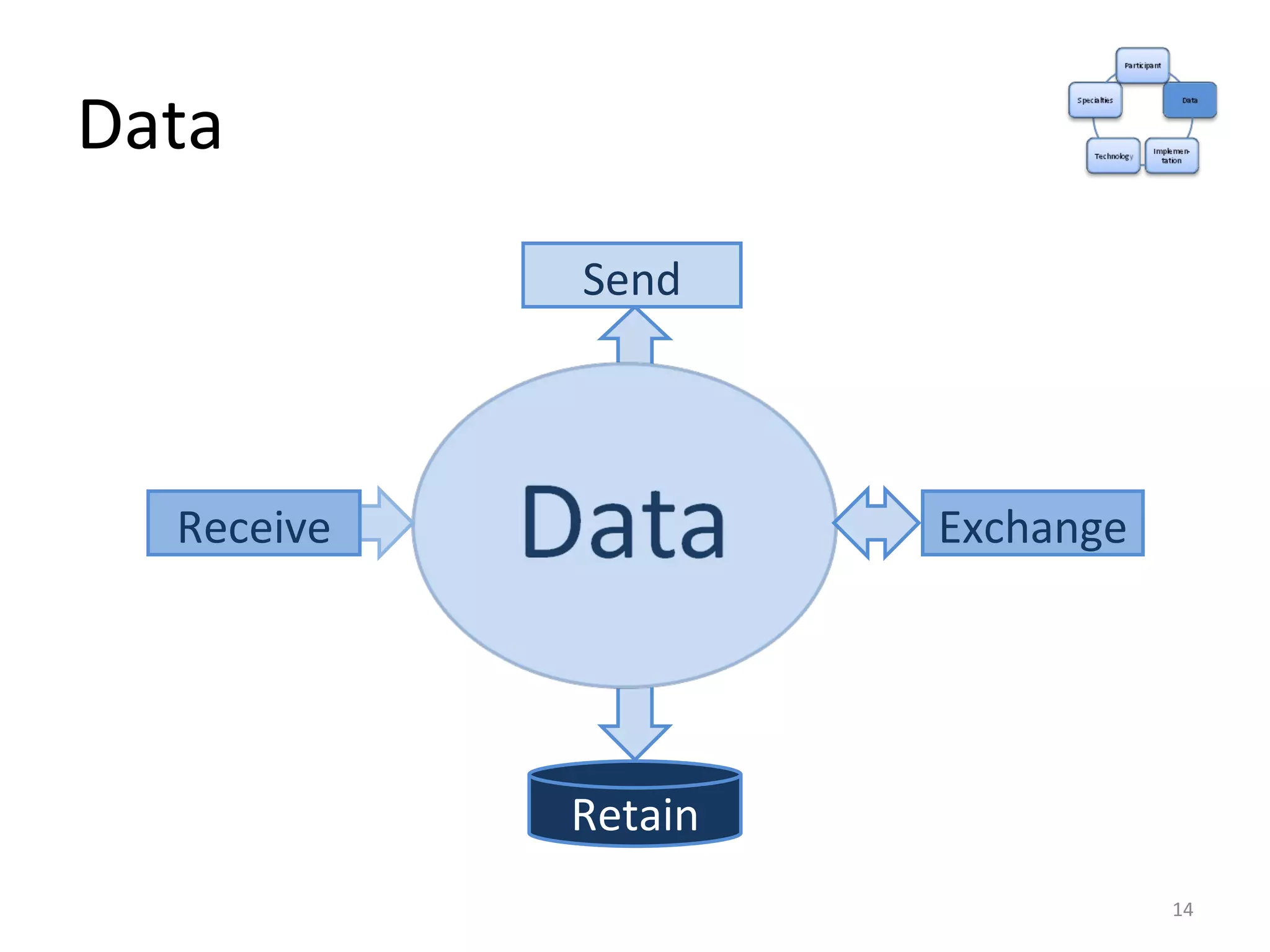
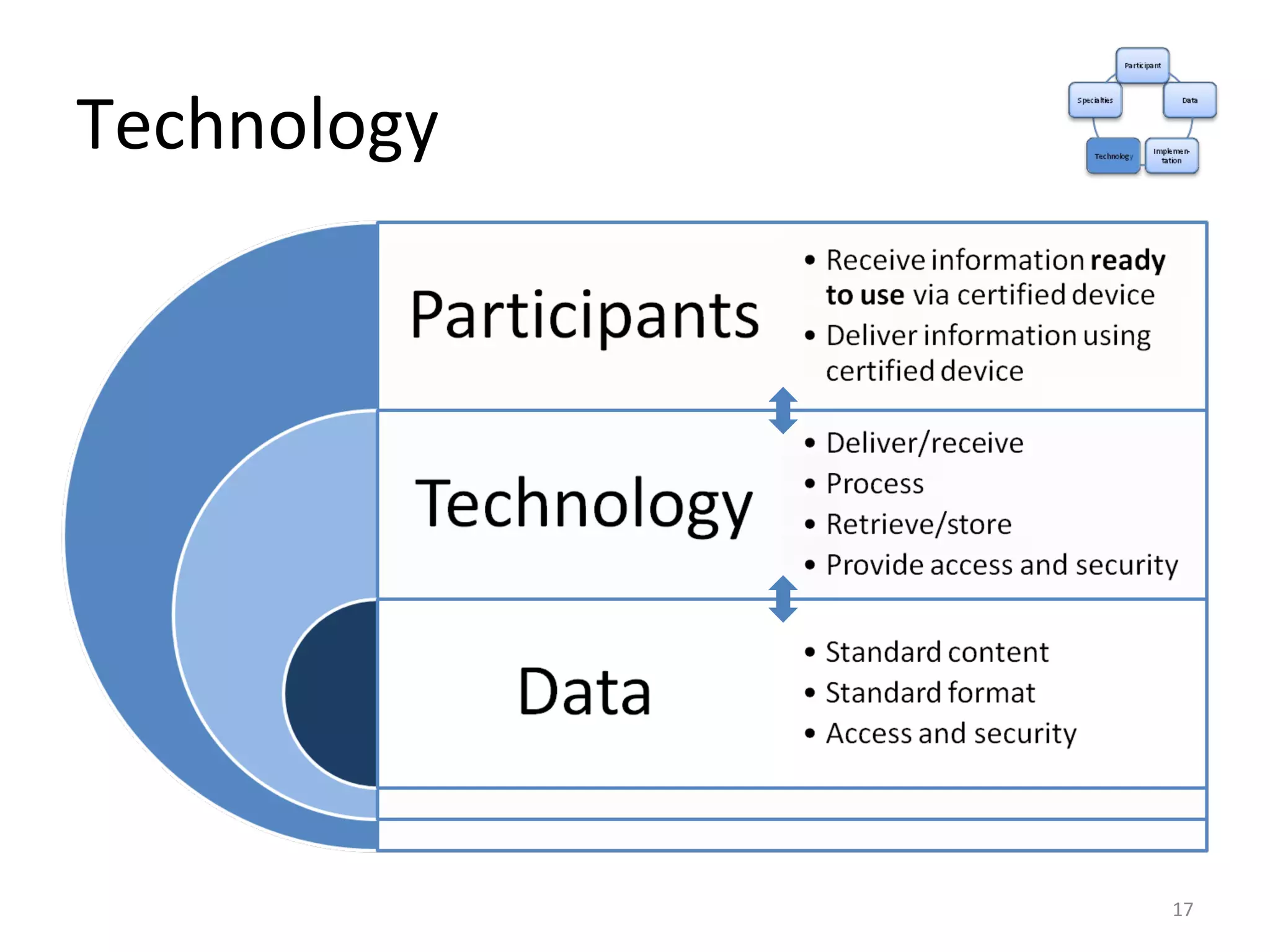
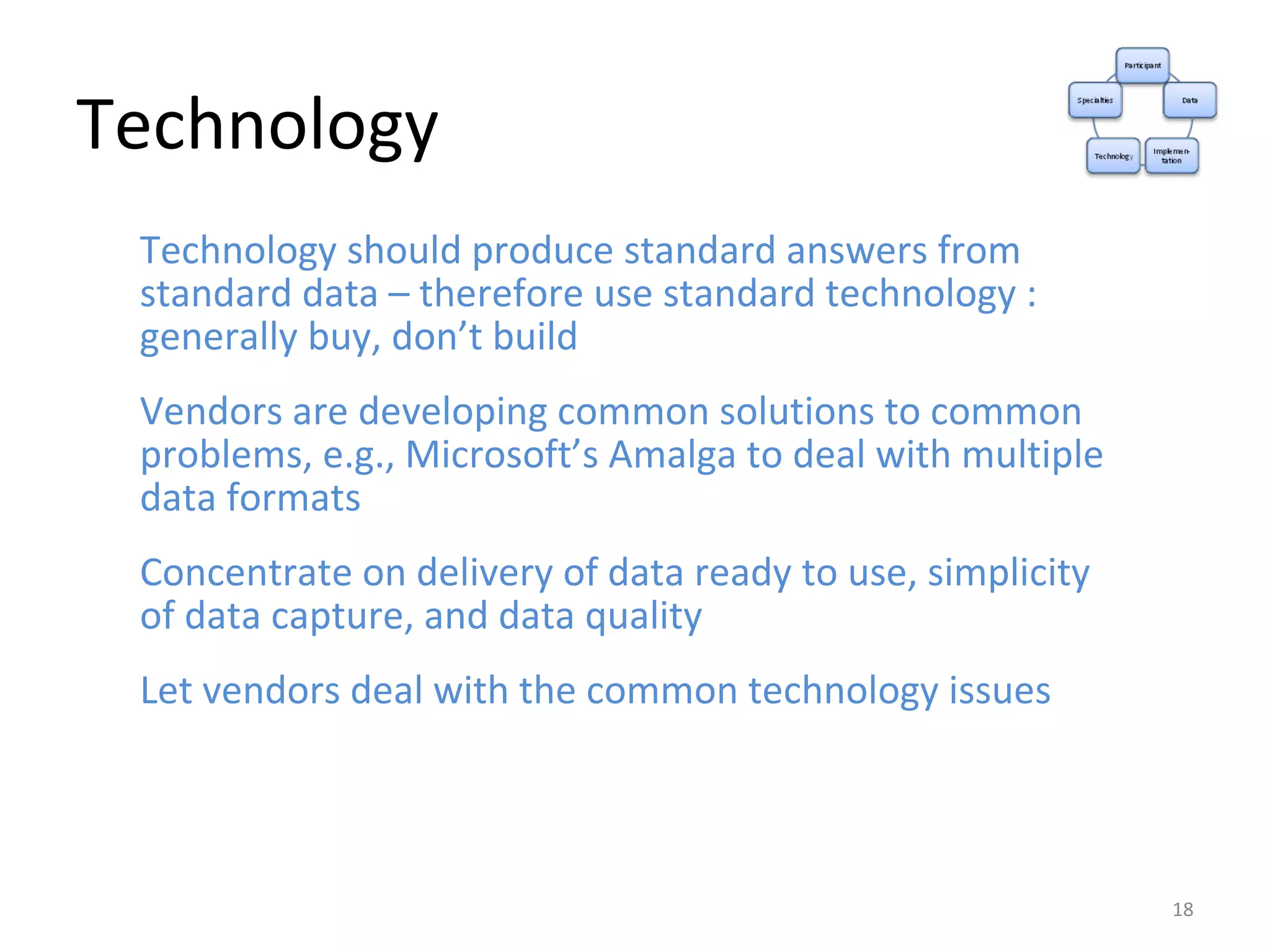
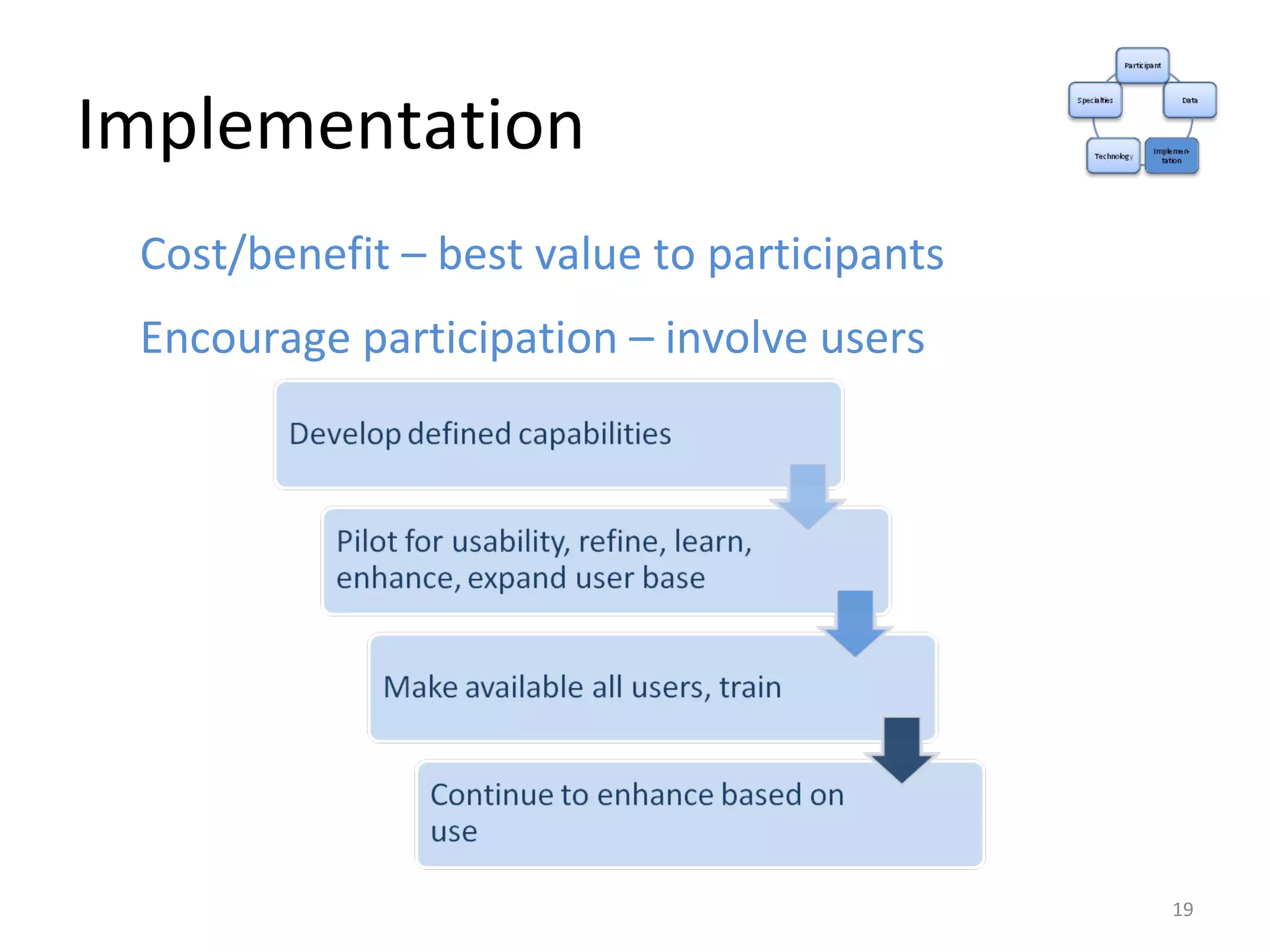
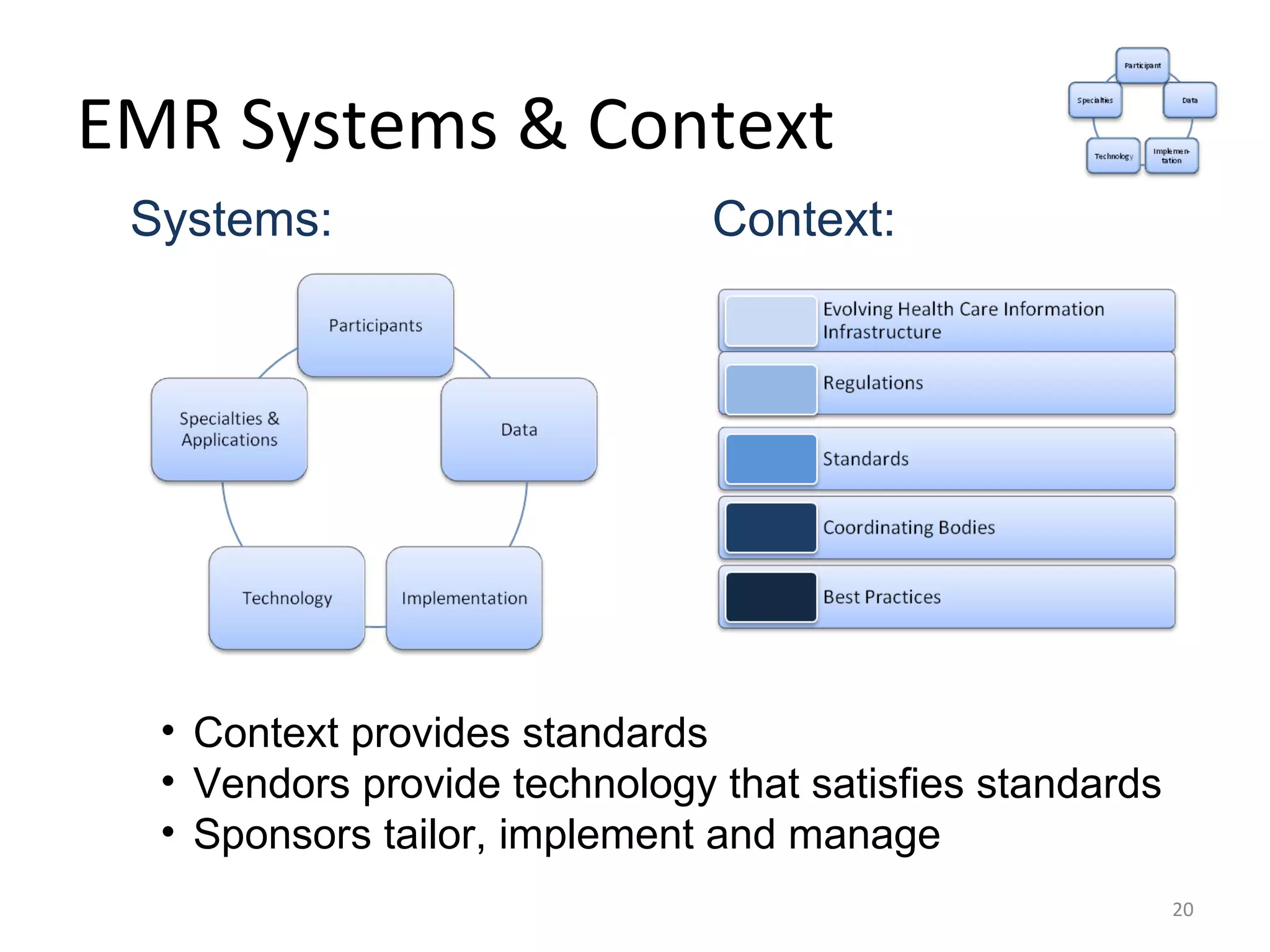
The presentation discusses the planning, management, and enhancement of electronic medical records (EMR) systems within the context of a nationwide health information infrastructure, highlighting the significance of the Health Information Technology for Economic and Clinical Health (HITECH) Act which incentivizes the adoption of certified EMRs. It reviews the current implementation status of EMR systems across hospitals and emphasizes the importance of interoperability and data management among various healthcare participants. The document also reflects on the challenges and policies related to data access, sharing, and the necessary technology to support EMR systems.
![We have worked in the white space of organizations … including HIPAA, Y2K, ERP, mergers and the implementation of evolving regulations The white spaces of organizations occur on organization charts between internal departments, in contractual ambiguity and regulatory complexity. They are places where functional misunderstandings occur, communication falters, roles change, priorities conflict, rewards are unclear, risks are unknown, and managers sometimes see threats to their careers that outweigh the opportunities. We work in those white spaces to define problems so they can be solved, design solutions so they can be implemented, and structure implementation so it can be managed. Hal Amens [email_address]](https://image.slidesharecdn.com/emr-anatomy-090526122324-phpapp01/75/Anatomy-of-an-EMR-System-21-2048.jpg)