Standard Admission Policy
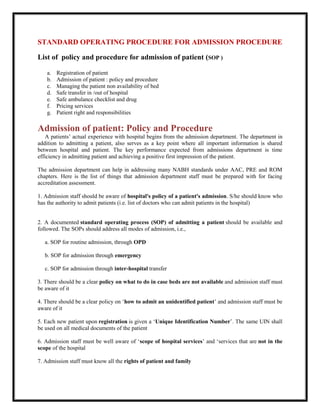
- 1. STANDARD OPERATING PROCEDURE FOR ADMISSION PROCEDURE List of policy and procedure for admission of patient (SOP ) a. Registration of patient b. Admission of patient : policy and procedure c. Managing the patient non availability of bed d. Safe transfer in /out of hospital e. Safe ambulance checklist and drug f. Pricing services g. Patient right and responsibilities Admission of patient: Policy and Procedure A patients’ actual experience with hospital begins from the admission department. The department in addition to admitting a patient, also serves as a key point where all important information is shared between hospital and patient. The key performance expected from admissions department is time efficiency in admitting patient and achieving a positive first impression of the patient. The admission department can help in addressing many NABH standards under AAC, PRE and ROM chapters. Here is the list of things that admission department staff must be prepared with for facing accreditation assessment. 1. Admission staff should be aware of hospital's policy of a patient's admission. S/he should know who has the authority to admit patients (i.e. list of doctors who can admit patients in the hospital) 2. A documented standard operating process (SOP) of admitting a patient should be available and followed. The SOPs should address all modes of admission, i.e., a. SOP for routine admission, through OPD b. SOP for admission through emergency c. SOP for admission through inter-hospital transfer 3. There should be a clear policy on what to do in case beds are not available and admission staff must be aware of it 4. There should be a clear policy on ‘how to admit an unidentified patient’ and admission staff must be aware of it 5. Each new patient upon registration is given a ‘Unique Identification Number’. The same UIN shall be used on all medical documents of the patient 6. Admission staff must be well aware of ‘scope of hospital services’ and ‘services that are not in the scope of the hospital 7. Admission staff must know all the rights of patient and family
- 2. 8. A general consent should be taken from all patients getting admitted 9. Admitting staff must know the scope of general consent and must explain it to patient before getting his/her signature 10. A written estimate of cost must be given to patient at the time of admission. This can be given by admitting staff after coordinating with admitting doctor and accounts department and should be as per standard pricing of hospital services. Alternatively, hospital can assign this responsibility to any other department, such as accounts. In any case written estimate should be given before patient takes admission decision. 11. Admission staff should well understand ‘confidentiality of patients’ information’ and must know rules for protecting information 12. At the time of admission following information must be shared with patient and family a. Categories of rooms/beds available with rates and facilities. b. Whether the category of bed will affect other treatment cost or not c. Additional chargeable services (such as ordering additional meals, use of internet etc.) that are applicable d. Name of admitting doctor e. Visit schedule of doctor f. Hospital’s policy on patients’ belongings g. Visitor timing and restrictions h. Meal timings and whether outside meals are allowed i. Rules and regulations of hospital applicable to patient and family, such as no smoking, no littering, restricted entry etc. (It is better that a printed document stating all such rules should be given to patient) 13. In case patient has a health insurance, necessary information for insurance processing must be provided either through admission department or by TPA desk 14. Following information must be shared with patient by the admitting doctor, before admission. (Admission department can coordinate to ensure that these information are provided) a. Diagnosis or provisional diagnosis b. Clinical reason for admission and plan of care (and indication if the plan of care is likely to change with further investigation) c. Approximate cost of treatment (can be facilitated by admission or accounts department) d. Expected duration of stay
- 3. e. Urgency or non-urgency of admission 15. All patients getting admitted must be educated on patients’ rights and responsibilities. This can be done through several ways such as display, or by handing over a patient rights booklet or by verbally explaining the rights to patients 16. Patient should be informed about complaint registration and redress mechanism of the hospital Quality Indicators 1. Average time taken per admission 2. Average waiting time of patients for admission 3. % of admission for which general consent not taken 4. % of admission for which written estimate of cost not given 5. % of complaints that indicate lack of information required to be given at the time of admission Admission of patient: Policy and Procedure Admission of patient is one of the main process followed in any hospital. It is the first step in providing healthcare to a patient as an in-patient. By admitting a patient, hospital undertakes a high level of responsibility for the care and well-being of the patient and hence it is essential to have relevant policy and procedure for admission in place to avoid any problems later on. It also ensures that the patients are admitted uniformly irrespective of their ethnicity, religion, caste, gender, financial class etc. This post describes relevant points that should be considered while formulating a policy and procedure of admission. (Also read - Registration of patient - Policy and Procedure) Admission Policy Right to admit a patient – Only those doctors (full time or on contract) who have been given privileges of admitting the patient in the hospital can recommend patient for admission. This is also applicable in case of patients from emergency. In case of patient being transferred from another facility the admission shall be ordered by a doctor having admission privileges. An updated list of such doctors shall be maintained at the admission department. Request for admission by any other doctor or from directly from patient or family members or by any other staff of the hospital shall not be considered. Responsibility of care – The doctor who orders for admission shall be considered as the primary doctor of the patient and he/she will be responsible for the medical care of the patient till the discharge or transfer of patient to any other doctor. Hospital shall be responsible for providing all facility and services necessary for patient’s stay and provision of medical care. Information to patient – Every patient shall be provided with all the necessary information before admission for him/her to make an appropriate decision. These information include following · Patients’ rights and responsibilities (A copy of patients’ rights shall be given) · Type of accommodation available along-with its amenities and charges for the same · Doctors round timing and how to contact doctors when required · Provision of food, timing and whether or not food from outside is allowed
- 4. · Number of attendant who will be allowed to stay with the patient and arrangement for the attendant · Visitors timings and rules related to visiting patients · Keeping of valuables in the hospital · Payment timings and mode of payments (In case of insurance patient details related to insurance payments) · Code of conduct during stay Cost estimate – Each patient at the time of admission shall be provided with an estimate of total cost of treatment, based on hospital's pricing policy. This shall be estimated with the help of the admitting doctor and by referring to the schedule of charges. The cost estimate shall be given to the patient in written. A disclaimer shall be made that the estimate may vary by certain percentage and may change significantly in case there is a change in treatment plan. In such cases a revised estimate will be given to the patient. General consent – A written general consent shall be obtained from each patient upon admission. This shall be as per the general consent policy. Standard general consent form shall be used for obtaining the consent. Non-availability of beds – In case the bed is not available in the category chosen by the patient the policy on ‘managing during non-availability of beds’ shall be followed Identification of patient - Appropriate Idnetification mechanism of the patient shall be created as per patient identification policy In case of an un-identified patient (for eg. Patient is sub-conscious or mentally unstable) admission shall be done by generating a temporary identification details. This shall be corrected as soon as identity gets established. Behaviour with patient – During the entire admission process the admitting staff shall be courteous, helpful and maintain good behaviour towards the patient. Patient shall be given sufficient opportunity to ask questions and clarify doubts. Rude behaviour or neglect of patient shall not be tolerated and can lead to penal action. Privacy and confidentiality – The communication between patient and admitting staff shall be carried out with sufficient privacy. All information collected from patient shall be kept confidential. Non-discrimination – The admission policy and process shall be uniformly applied to all patient seeking admission. No discrimination shall be done on the basis of patient’s ethnicity, religion, caste, gender, financial class and any other background of the patient. Admission Procedure 1. Admission process of a patient shall be carried out at the admission desk/admission chamber. The process starts as soon as the patient arrives to the desk with the admission order from the doctor. 2. Check the written admission order brought by the patient and ensure that it is from a doctor who has the admission privileges granted by the hospital. In case, patient do not have the appropriate written order, admission shall not be done and patient shall be appropriately guided. 3. Obtain necessary details of the patient. This can be done through the Unique ID number of the patient which was generated during registration. Additional details shall be obtained by asking the patient to fill up the admission form. In case of unidentified patient a temporary identification shall be provided for the purpose of completing admission.
- 5. 4. Allocation of bed/room – Inform the patient about various categories of accommodation available, its features and cost. Help the patient in selecting an appropriate accommodation of his/her choice. In case the chosen category is not available, follow the policy and procedure of ‘Managing during non-availability of beds’ 5. Information provision – Provide all information to the patient as described in the policy above. Patient information booklet that contains all necessary information, along with patients’ rights shall be handed over to the patient 6. Cost estimate provision – The admission staff in consultation to the doctor should work out an estimate of the total cost that would be incurred to the patient, as per hospital's pricing policy. This cost estimate shall be given to the patient in written. A copy of this estimate, duly signed by the patient shall be retained as an evidence. 7. Taking general consent – General consent shall be taken from the patient after provision of information and cost estimate and after final confirmation of admission. This should be done as per general consent policy and in the standardized format 8. Registering the admission– Patient’s admission shall be registered/recorded in the system as per the patient’s choice of accommodation and availability of beds. 9. Generation of Patient identifier - Patient identifier shall be generated which includes Patient ID band and patient's identification labels (sheet of stickers with printed patient identification details) shall be generated. This shall be as per patient identification policy and procedure. 10. Generation of medical record – A medical record shall be generated for the patient which should have patient details and basic formats within it. If the patient is an existing patient, who has been admitted in past, the previous medical record number shall be stated on the new medical record file created. 11. Payment of advance – Patient/family member shall be asked to pay the required advance amount at the billing counter and submit the receipt back. 12. Sending patient to ward - After successful payment, patient shall be directed towards the appropriate ward. An attendant should to escort the patient, if needed. The medical record and patient identifier (ID band and the identification labels) shall also be sent to the ward by the hands of attendant. 13. Internal communication – Immediately after admission information shall be sent to the ward in- charge and to the accounts department 14. In the ward – The ward in-charge upon receiving the information shall allocate a primary nurse for the patient. As soon as the patient arrives, primary nurse shall help the patient to get into the room/bed. She should then make an entry in the ward’s admission/discharge register and sends an information of new admission to the medical officer on duty and the admitting doctor. 15. In case of any unforeseen event the Hospital Administrator shall be contacted who will take appropriate decision as per situation.
- 6. Managing patients during non-availability of beds A patients’ actual experience with hospital begins from the admission department. The department in addition to admitting a patient, also serves as a key point where all important information is shared between hospital and patient. The key performance expected from admissions department is time efficiency in admitting patient and achieving a positive first impression of the patient. The admission department can help in addressing many NABH standards under AAC, PRE and ROM chapters. Here is the list of things that admission department staff must be prepared with for facing accreditation assessment. 1. Admission staff should be aware of hospital's policy of a patient's admission. S/he should know who has the authority to admit patients (i.e. list of doctors who can admit patients in the hospital) 2. A documented standard operating process (SOP) of admitting a patient should be available and followed. The SOPs should address all modes of admission, i.e., a. SOP for routine admission, through OPD b. SOP for admission through emergency c. SOP for admission through inter-hospital transfer 3. There should be a clear policy on what to do in case beds are not available and admission staff must be aware of it 4. There should be a clear policy on ‘how to admit an unidentified patient’ and admission staff must be aware of it 5. Each new patient upon registration is given a ‘Unique Identification Number’. The same UIN shall be used on all medical documents of the patient 6. Admission staff must be well aware of ‘scope of hospital services’ and ‘services that are not in the scope of the hospital 7. Admission staff must know all the rights of patient and family 8. A general consent should be taken from all patients getting admitted 9. Admitting staff must know the scope of general consent and must explain it to patient before getting his/her signature 10. A written estimate of cost must be given to patient at the time of admission. This can be given by admitting staff after coordinating with admitting doctor and accounts department and should be as per standard pricing of hospital services. Alternatively, hospital can assign this responsibility to any other department, such as accounts. In any case written estimate should be given before patient takes admission decision. 11. Admission staff should well understand ‘confidentiality of patients’ information’ and must know rules for protecting information
- 7. 12. At the time of admission following information must be shared with patient and family a. Categories of rooms/beds available with rates and facilities. b. Whether the category of bed will affect other treatment cost or not c. Additional chargeable services (such as ordering additional meals, use of internet etc.) that are applicable d. Name of admitting doctor e. Visit schedule of doctor f. Hospital’s policy on patients’ belongings g. Visitor timing and restrictions h. Meal timings and whether outside meals are allowed i. Rules and regulations of hospital applicable to patient and family, such as no smoking, no littering, restricted entry etc. (It is better that a printed document stating all such rules should be given to patient) 13. In case patient has a health insurance, necessary information for insurance processing must be provided either through admission department or by TPA desk 14. Following information must be shared with patient by the admitting doctor, before admission. (Admission department can coordinate to ensure that these information are provided) a. Diagnosis or provisional diagnosis b. Clinical reason for admission and plan of care (and indication if the plan of care is likely to change with further investigation) c. Approximate cost of treatment (can be facilitated by admission or accounts department) d. Expected duration of stay e. Urgency or non-urgency of admission 15. All patients getting admitted must be educated on patients’ rights and responsibilities. This can be done through several ways such as display, or by handing over a patient rights booklet or by verbally explaining the rights to patients 16. Patient should be informed about complaint registration and redress mechanism of the hospital Quality Indicators 1. Average time taken per admission
- 8. 2. Average waiting time of patients for admission 3. % of admission for which general consent not taken 4. % of admission for which written estimate of cost not given 5. % of complaints that indicate lack of information required to be given at the time of admission ERA LUCKNOW MEDICAL COLLEGE AND HOSPITAL ERA UNIVERSITY 226003 TOPIC: DATE: VENUE: TRAINING TO BE ATTENDED BY : TRAINNER BY : Registration of patients in hospital – Policy and Procedure Registration is a process by which a patient’s name and identity are enrolled into the records of the hospital. This is required in order to provide services of the hospital to the patient and to keep a track of various services that are availed by each patient. This is also the first step to generate a medical record of the patient in which all medical details of the patient are documented. Registration is done with the following objectives 1. To collect basic details of patient related to identity, contacts and demography 2. To create a unique identification number for each and every patient 3. To enter patient’s name in the hospital’s system 4. To generate a record of the patient for documenting further processes related to him/her To ensure that registration process is carried out smoothly and its objectives are met, a hospital must have a well-defined and documented policy and procedure for carrying out registration of patients. The guidelines given below can help in formulating a relevant policy and procedure for registration. Who should be registered All first time patient to the hospital who wants to avail the services of the hospital must be registered. This includes patients who come to OPD or Emergency or transferred in from another hospital. However, in following situations registration shall not be done 1. If the patient is already registered with the hospital and registration details in available 2. If the healthcare service required by the patient is not available in the hospital
- 9. 3. If the patient unknown to the hospital is brought in dead condition. In this case brought in dead policy must be followed When shall the registration be done Registration shall be done as a first step before any healthcare service is provided to the hospital. However, in a medical emergency situation where care needs to be provided urgently, registration can be done simultaneously or later as per the situation. Such cases shall be handled in the hospital’s emergency department and urgency shall be determined based on Triage process How shall the registration be done Registration shall be done by asking the patient to fill up the registration form, in which basic details of the patient is required to be filled. Help shall be provided to the needy patient in filling up the registration form. The form shall be signed by the patient (or thumb impression taken). The details from registration form shall be entered into the registration module of HIS. Once the information is saved, the computer will generate a unique identification number (UIN). This UIN along with name, address and date of birth of patient shall be printed, signed and handed over to the patient. Applicable fee of registration must be collected from the patient for which the receipt must be issued. The registration form that was filled and signed by the patient must be stored securely in the registration file. In the case of a minor patient, the parent/guardian of the patient must sign on the registration form Information to be collected at the time of registration Following information must be collected from the patient through registration form · Name · Date of Birth · Gender · Name of guardian (in case the patient is a minor) · Relationship with the patient · Address · Contact number · Email address · Occupation · Health Insurance details (If applicable) · Referring doctor’s name (if applicable) · For contacting during emergency o Name of person o Relationship o Contact number
- 10. Information to be provided to a patient getting registered Patient getting registered must be informed that this is a one-time registration and will remain valid for the lifetime. He/she should be told about the unique identification number and that it can be used to access the hospital’s services in future. He/she shall also be informed about how his/her registration details can be retrieved other than UIN. Registering an unidentified patient In case an identified patient is brought to the hospital (such as an unconscious patient brought by strangers), an incomplete registration shall be done by entering the name as ‘Unidentified’ followed by a serial number. For example, first unidentified patient shall be written as ‘unidentified-1’ next one as ‘unidentified-2’ and so on. A UIN will still be generated for that patient and healthcare services can be provided. The incomplete registration shall be completed as soon as identification details of the patient become available. Retrieving the details of a registered patient UIN can be used for retrieving the details of the patient in any department of the hospital. However, if the patient has forgotten his/her UIN, the same can be retrieved from the HIS, by entering other details of the patient such as name, date of birth, contact number etc. Confidentiality of information The information collected at the time of registration is private information of the patient and shall be kept confidential. This is an important part of fulfilling patients' rights. The information shall only be used for the purpose of providing healthcare services. The access of the patients’ information will only be given to specific departments and staff. This data shall not be revealed to anyone from outside of the hospital. In certain circumstances, such as legal authorities requesting for information, the facility head (or a designated authority) shall take the decision. Modifications in details collected during registration Once the registration is completed, any modification in the information collected shall generally not be done. However, in certain cases, such as spelling mistake in the name, or a correction required for insurance claim processing, the facility head (or a designated authority) shall take a decision on a case to case basis, after assessing the evidence for modifying information. If modifications are made, a track of all modifications shall be maintained. Registration record As the registration is for the lifetime the registration details shall be saved and stored for the lifetime in HIS. The registration form filled and signed by patient shall be stored for at least one year after which it can be discarded through shredding.
- 11. ERA LUCKNOW MEDICAL COLLEGE AND HOSPITAL ERA UNIVERSITY 226003 TOPIC: DATE: VENUE: TRAINING TO BE ATTENDED BY : TRAINNER BY : Patients’ Rights and Responsibilities in hospital Patients and their family has certain defined rights which hospitals and medical practitioners need to fulfill. Some of these rights are legally enforceable and a patient can approach consumer court or higher court, if those rights are infringed. Other rights are derived on ethical ground and can affect the image of healthcare provider and its relationship with patient community. Besides legalities, almost all healthcare accreditation program gives a lot of importance to protection of patients’ rights and not fulfilling the same may lead to denial of accreditation. While it is important for healthcare providers to fulfill the rights of patients, some of these rights are complex to understand because of the unique and complex scenarios that occurs in healthcare frequently. This post attempts at simplifying those rights with respects to its scope and intent and guide the healthcare providers on what needs to be done to fulfill them. The rights discussed here have been referred from charter of patients’ rights by consumer guidance society of India, code of ethics regulation by MCI and NABH accreditation standards. Right to be explained about his/her health problems and treatments This is one very important right which also has high significance in legal matters. It requires that a patient is informed and explained about all such thing which will enable him/her to take an informed decision about his/her healthcare. This could be further divided in following o Patient shall be explained about his/her disease or health condition in detail. This means that patient is made aware of his/her diagnosis, whether provisional or final, with an explanation of the diagnosis in a simplified language that the patient can understand. This also includes informing patient about reason why a specific diagnostic test is being ordered for him/her. o Patient shall be explained about the proposed treatment for his/her condition, including the side-effects and expected benefit from it. o Patient shall also be explained about the alternatives to the proposed treatment (if any), including its risks and expected benefits o Patient shall be informed about the progress in his/her health condition and change, if any, in the proposed plan of care How to fulfill this right? The most important part of fulfilling this right is to have a strong policy and procedure of obtaining a written consent from patients. The consent taking process should be specified to ensure that patient receives all required information. A general consent should also be taken from patient in written Importance of fulfilling this right must be emphasized and its legal implications must be explained to all doctors
- 12. Special situations pertaining to this right o In situations where the patient is not competent to make decisions, such as patient is unconscious, mentally unstable or of minor age, this right should be fulfilled by informing the patients’ family member (next of the kin) or guardian or custodian (like jailer in case of prison inmate, custodian of the orphanage etc.) who would be taking decision on patient’s behalf. o If the patient is not competent to make decision and is also not accompanied by a family or custodian (for eg. In case of unidentified patient brought in an unconscious stage and needs a surgery for which a consent is required), two doctors can jointly give consent in good faith of the patient. This consent also must be documented. Right to be involved in decision making process about his/her own care This right flows from the earlier right of being explained about illness and treatment. This requires that after explaining all relevant details about illness and treatment, patient’s views and preferences should be taken into consideration and treatment plan should be modified accordingly. For example, if a patient with knee joint problem who has been proposed knee replacement surgery, wants to avoid it for as long as possible, the treatment plan should be modified to provide relief from symptoms for as long as possible before actual knee replacement is carried out. This also gives following additional rights to the patients Right to take a second opinion (and even multiple opinions) Right to refuse treatment at any point of time Right to get discharged against medical advice (DAMA) How to fulfill this right? o This being a part of the earlier right, incorporating this requirement in the informed consent policy will be required to fulfil it. o Besides this, informing patients that they have these right is also an effective way to honour this right o A policy and process on handling DAMA should be there in place Right to know his/her doctor’s credentials If asked by the patient, it would be obligatory on part of the hospital or the doctor to provide the full credentials of the doctor who would be treating the patient. The details of doctors that could be asked include, qualifications, institute from where obtained, specialization, years of experience and any other professional details. However, the information that are irrelevant to doctor’s professional credibility or are private information about the doctor may be denied. For example, details of past patients treated by the doctor, HIV status of the doctor, his/her family or residential details are irrelevant and may be denied to the patient. How to fulfill this right? o Have a credentialing system through which updated credentials of each doctor empanelled with the hospital is maintained. o A brief profile of all the doctor highlighting important credentials should be maintained on website, brochure or pamphlets which can be handed over to the patient who request for it Right to know an estimate of the cost of the treatment Cost of treatment is an important information for patient to decide whether or not they would like to get that treatment done. It is obligatory on the part of healthcare provider to provide as best estimate of the cost of proposed care, as possible and at right time. If there is any change of care plan which can affect the cost, patient should be again informed about the cost implications. How to fulfill this right?
- 13. o Written estimate must be given to all patient at the time of admission. The hospital must fix responsibility to someone for working out estimate and communicating the same to patient. Hospital should also have a standardized pricing of services for all its patients. o Have a standardized form in which estimate can be given with important details. o Have a system in place to ensure that change of estimate is communicated to the patient on time o Have a system in place to communicate daily or interim bill with the patient o Evaluate the estimates being given by comparing the same with the final bill amount and make improvements in the process Right to confidentiality of personal and health related details All data and information collected from patient, whether personal or related to his/her healthcare should be kept confidential and used only for the purpose of providing healthcare. There could be numerous situations which could lead to breach in confidentiality. Such as, keeping medical records in open where any one can easily access it, displaying identity of the patient outside the room or by providing information about patient on phone to anyone without confirming his/her relation with patients etc. How to fulfill this right? o Having a detailed policy on confidentiality specifying all precautions that must be taken to ensure confidentiality o Restricting access of medical records only to the healthcare providers and to the patient. Access to others should be given only with patients’ explicit consent o Policy of not disclosing patients details over phone or to any-one else other than those identified as the patients’ family members or guardian o Control and safeguards on accessing information on HIS o Use of patients’ information for publicity, promotion of hospital etc. should be done only with explicit consent of the patient o Staff should be oriented that patients’ details should not be discussed in public areas or with people who are not related to the patients’ treatment o Ensuring that patients’ details are not displayed or kept in areas where it could be seen or accessed by unauthorized personnel. Examples include displaying patients full name in waiting areas or discarding filled registration forms in general waste bins etc. o Maintaining medical and other records of patients in a secured area and destroying these records in a manner that prevents its unauthorized retrieval of information from it. For example medical records should be shredded after its retention period and not sold off as scrap papers. Right to be respected for special preferences, spiritual and cultural needs Patients may have certain personal preference based on his/her belief system or living habits. Some examples include, eating only vegetarian or Jain food, wearing certain ornaments that they might consider lucky to them or listening to a specific chants every day. Similarly, patients may have spiritual and cultural needs. For example, praying and worshipping requirement as per the patient’s religion, following of rituals specially on occasions of birth or deaths, or observing some religious practices on occasion of festivals etc. The hospital must respect these individual preferences, habits, spiritual and cultural needs and should try to accommodate or allow as many of them as possible. However, restrictions can be put on those practices which has a reasonable risk to the health and safety or if it can cause inconvenience to other patients in the hospital or if it can affect the functioning of the hospital. How to fulfill this right? o Sensitize your staff through regular sensitization program, on respecting patients’ preferences, spiritual and cultural needs
- 14. o Have clear policy on what kind of needs could be honoured. For example, can patient be allowed to have non-vegetarian food in hospital? What kind of rituals will be allowed to be performed in case of births and deaths? Etc. · Have a guideline for staff on how to respond in case of patients’ expressing their spiritual, cultural or preferential needs. · Unique situations arising, should be brought to a multidisciplinary committee, who should then discuss and issue directives. (Refer list of committees required in a hospital) · Identify what needs are frequently expressed by your patients and have arrangements for fulfilling them. Some examples could be designating a prayer room, availability of a Pundit, Chaplain or Moulvi to attend to dying patients, provision for preparing Jain food in kitchen etc. Right to privacy and dignity during medical procedures While performing healthcare functions, such as examination, investigations and treatment, there could be situations where patients’ privacy and dignity could get compromised. For example, undressing whole or a part of body for physical examination, conduction of PV examination, provision of certain therapies etc. Similarly, situations such as patient discussing his/her disease with doctor or being counselled for family planning etc. requires privacy. Hospitals must ensure that adequate privacy is provided in needed situation and patients’ dignity is maintained throughout his/her care. How to fulfill this right? o Having adequate infrastructure arrangement for privacy, such as bed side curtains in multi-bed ward doors and windows that can be closed when privacy has to be provided, providing adequate change rooms where needed and restricted entries in areas of privacy such as labour room, procedure room etc. o Clear policy on situations where visual and hearing privacy must be rendered to patients o Guidelines to doctors, nurses and technicians on how to provide adequate privacy including hearing privacy o Privacy and dignity shall also be maintained during restraint of a patient Right to protection from neglect or abuse: There are instances of patients being abused or neglected in healthcare settings. For example, delay in attending the patient despite being urgently called by patient/relative, talking rudely to patient if he/she frequently calls for help or harassing the patient for procedural matters. This right requires that healthcare organizations put into place measures to prevent and to deal with such happenings. This right also entails that patients are not discriminated on the basis of their background or setting in which they are receiving care and are provide medical care as per their clinical condition How to fulfill this right? o Having a clear policy documented and communicated to staff conveying the message of ‘No tolerance to abuse or neglect of patients’. The policy must explain what constitute abuse/neglect with examples o Having a mechanism for capturing such events. Patient feedback, anonymous feedback from staff, monitoring rounds etc. can be some of them o Having a disciplinary policy and procedure in place to investigate and decide repercussions, when an occurrence of any abuse/neglect comes to notice. · Making a policy on provision of uniform care to all patients and specifying elements that must be the part of uniform care. Right to complain and receive the response on their complaints Patients can voice there complain to an appropriate authority and can expect a response on their complaint
- 15. How to fulfil this right? o Have an adequate mechanism in place for patients to loge complaint without any apprehension. Some of the mechanisms include, having complaint drop boxes at various locations, displaying a phone number and/or email id on which complaints can be sent, capturing complaint through feedback mechanism etc. o There should be a designated authority who should receive all complaints for review and further processing o Each complaint must be processed through relevant department/authority or committee. o A response must be sent to the patient about the action taken or not taken with reasons, within a defined timeframe Right to die with dignity The right to die with dignity is the latest addition in rights of a patient (and for all citizens). This has come in effect with legal approval of Passive Euthanasia and Advance directives. Please refer the linked post for getting details of scope and conditions related with this right. ERA LUCKNOW MEDICAL COLLEGE AND HOSPITAL ERA UNIVERSITY 226003 TOPIC: DATE: VENUE: TRAINING TO BE ATTENDED BY : TRAINNER BY : TYPE OF TRAINING : Safe transfer of unstable patient from hospital One of the critical task that hospitals have to frequently undertake is to transfer a critically ill or unstable patient from one hospital to another. Transfer of such patient are likely to induce various physiological changes, which may adversely affect the health of patient even leading up- to death. Hence, such transfers shall be undertaken with great care and as per evidenced-based guidelines. Following are the key elements and guidelines for safely executing transfer for an unstable patient. Criteria for identifying unstable patients A patient whose physiological status is in fluctuation and for whom emergent treatment and/or surgical intervention are anticipated, is considered as an unstable patient. Hospital should use clinical criteria to identify an unstable patient. Following criteria can be used as reference for developing hospital’s own criteria Patients with one or more of below condition shall be considered as unstable patient Glasgow coma scale <= 14 Pulse < 60 or > 120 beats per minute Systolic blood pressure > 190 mmhg Following comorbid condition if present increases the risk of unstability Age > 55 years History of coronary artery disease History of COPD History of liver disease
- 16. Respiratory rate < 12 or > 24 breaths per minute Poor gas exchange, with oxygen saturation < 90% Temperature < 92°f (< 33°c) Paralysis Hoarseness or inability to talk Laboured respirations Severe pain External haemorrhage Combative Severe deformity involving spine, neck, chest or extremities Penetrating wound from head to popliteal fossa History of coagulation disorder History of mental illness Current insulin-dependent diabetes mellitus Current anticoagulation therapy Current pregnancy Neonates Decision to transfer: The decision to transfer the patient shall be taken by a senior consultant level doctor after discussing with patient's relatives about the benefits and risks involved. The decision of transfer shall only be taken if benefits of transferring the patient outweigh the risks involved in transferring. A written informed consent shall be taken from patient/family before the transfer Communication with receiving facility: The facility where the patient is being transferred shall be informed prior to shifting. It is always preferable that the consultant doctor of the transferring facility speaks to the consultant doctor of the receiving facility. Complete information on patient's clinical condition, treatment being given, reasons for transfer, mode of transfer and timeline of transfer, shall be shared with the receiving facility in a written document. Pre-transfer stabilization and preparation: Patients should be properly stabilized and prepared before transferring to prevent any adverse event or deterioration in patient’s clinical condition during transfer. The patient should be adequately resuscitated and stabilized to the maximum extent possible. Following points can be used as a checklist for pre-transfer stabilization 1. Airway – If compromise in airway is suspected during transfer of patient, endotracheal tube intubation shall be done. 2. Breathing – Arterial blood gas values should be optimized and breathing should be adequately controlled. In patients suspected of pneumothorax, chest drain shall be inserted. 3. Circulation – Control for external haemorrhage. Ensure that cross matched blood is available during transport, if required. Haemorrhagic shock shall be adequately treated 4. Neurological status – In case of patients with head injury their Glasgow coma scale should be adequately monitored and documented. Patient shall also be protected from cold by provision of blankets during transfer.
- 17. Mode of transfer Mode of transferring the patient shall be selected as per the clinical condition of the patient. Following guidelines shall be taken into consideration. 1. Patients with non-life threatening condition can be transported in a Basic Life-Support Ambulance. 2. Patients with life-threatening conditions or patients who may endotracheal intubation, cardiac monitoring, defibrillation, administration of intravenous fluids or vasopressors, during transfer, shall be transported using Advances Life-Support Ambulance 3. Patients on life support system, i.e. ventilator can be transported in a mobile ICU ambulance, if available 4. In some extreme cases, where patients clinical condition is critical and time is a big factor, use of air ambulance shall be considered, if available. However, feasibility of air transfer shall be ascertained with respect to environment, and patient’s condition. If the patient, due to his/her condition can undergo sudden decompensation during air transfer, the same shall be avoided Checklist for Ambulance Accompanying the patient It is recommended that two competent personnel accompany the unstable patient during transfer. The accompanying person shall be suitably trained in patient transfer, advanced cardiac life support, airway management and critical care. It is also recommended that a physician shall accompany the patient, however, if this is not possible then provision for contacting the concerned physician shall be there. For deciding who should accompany, the patient can be categorized into 4 levels · Level 0 – Patients who can be managed at the level of ward, usually do not require any specially trained person to accompany · Level 1 – These are patients who are at risk of deterioration during transfer, but can be managed in acute care setting. Such patient shall be accompanied by a paramedic or a nurse · Level 2 – These patients require observation or intervention for failure of single organ system and must be accompanied by trained and competent personnel · Level 3 – These are patients with advanced respiratory care requirement during transfer with support of at-least two failing organs. These patients shall be accompanied by a competent doctor along-with nurse or paramedic Equipment and Drug The ambulance transporting the patient shall be equipped with necessary equipment, monitoring devices, medicines and consumables. All the monitoring needs to be established before the commencement of transfer along with the starting of infusion drugs. There should be one person responsible for patient transfer, who shall ensure availability of all these. Documentation and record In all stages of transfer, documentation shall be clearly done. Patient's condition, reason to transfer, names and designation of referring and receiving clinicians, details and status of vital signs before the transfer, clinical events during the transfer and the treatment given, shall be recorded in patients’ medical files. Handing over shall also be documented and things handed over along with the patient, such as medical files, clinical reports, films etc. shall also be recorded.
- 18. Quality improvement Any untoward incident happening during transfer shall be recorded and reported to appropriate authority. Each such incident shall be investigated and proper corrective and preventive actions shall be taken. Periodic audit of transfer process shall be done and the transfer records shall be reviewed. Reference: Kulshrestha A, Singh J. Inter-hospital and intra-hospital patient transfer: Recent concepts. Indian journal of anaesthesia. 2016 Jul;60(7):451. ERA LUCKNOW MEDICAL COLLEGE AND HOSPITAL ERA UNIVERSITY 226003 TOPIC: DATE: VENUE: TRAINING TO BE ATTENDED BY : TRAINNER BY : TYPE OF TRAINING : Consent for hospital (IPD cases) General Consent and Informed Consent in Hospitals General consent is an umbrella consent taken for conducting those patient care processes which do not pose any significant risk of harm to patient. For example, physical examination, collection of blood sample, Intravenous administration of fluids etc. are less risky processes when compared to surgery, anaesthesia etc. and can be done by taking a general consent from patient. The reason it is called as a general consent is because under one consent, the hospital can do multiple patient care processes that are within the scope of general consent. Even though it is called as general consent, it has to be informed to the patient about the scope its scope, before he/she gives consent. In OPD patients, general consent can be considered as implied for all non-risky OPD based procedures and written consent may not be required. However, in patients being admitted, general consent must be documented with patients’ signature. A standard general consent form can be used for this purpose. The scope can cover consent for… · Admitting the patients in an intermediate care ward/room (Scope does not cover admission of patient to ICU for which a separate informed consent should be taken) o Physical examination and clinical assessment o Conduction of routine laboratory tests, as per doctor’s order. o Conduction of imaging tests such as X-ray, Echo, ECG etc. For o Minor surgical procedures such as abscess draining, wound cleaning, stiches etc. o Fracture reduction closed and cast application o Any other investigation or procedure that are considered to be less risky as per the current knowledge in medical science o Disclosing medical information and basic details of patient to healthcare providers o Disclosing patients’ information, diagnosis, treatment and bills to insurance companies or to payer of bills, if required, on behalf of the patient. Patient will be informed before this.
- 19. Following points must be ensured with regard to general consent General consent should be taken in written with patients’ signature at the time of admission. The consent should be taken before admitting the patient. Scope of general consent must be explained to patient. It should also be informed that in case of clinical procedure that is not covered under general consent, a separate informed consent will be taken It should also be informed that patient may withdraw consent 6. Informed consent on the other hand is required for conducting clinical processes that can have significant risk of patient harm, such as surgery, blood transfusion, radiation therapy etc. Informed consent should be specific to the clinical process that is required to be done and patient must be informed about the risks, benefits and alternatives of the clinical process, before he/she gives consent. As informed consent is taken for risky processes, it is extremely important to provide brief the patient thoroughly before he/she makes a decision. Standard informed consent forms may be used for documenting the consent of patient/family. However, as informed consent is generally specific to the clinical procedure, separate informed consent forms may be required for different procedures. Informed consent stands as the most important document in case of medical lawsuits. Hospitals must list out the clinical procedures for which ‘Informed Consent’ should mandatorily be obtained. A sample list of procedures for which informed consent should be taken is given below. 1. Abdominal, pleural or pericardial drainage and drainage tube insertion 2. Administration of investigational drugs 3. Advanced directives for ‘Do Not Resuscitate (DNR)’ 4. Any surgical procedure 5. Ascites tapping / Abdominal paracentesis 6. Blood transfusions (physician only) 7. Bone marrow biopsy and /or aspiration 8. Central line placement 9. Chemotherapy – any route 10. CT guided or US guided FNAC 11. CT scan with contrast 12. Fine Needle Aspiration for Cytological studies (FNAC) 13. Foley’s catheterization 14. HIV testing 15. Immune therapy, intravenous or sub-cutaneous 16. Incisional, excisional, punch or shave biopsy 17. Intubation 18. Lumbar puncture 19. Major or minor surgery which involves an entry into the body either through an incision or through the use of natural openings 20. Nasogastric tube insertion 21. Non-operative procedures which involve more than a slight risk of harm to patients, or which involve the risk of a change in patient's body structures 22. OCD / Direct Laryngoscopy / Bronchoscopy / Cystoscopy / Colonoscopy / Sigmoidoscopy 23. Participation in clinical research protocols 24. Procedures involving general anaesthesia, or moderate or deep sedation, whether or not entry into the body is involved 25. Procedures utilizing radium, x-rays, or isotopes
- 20. 26. Sterilization 27. Thoracentesis 28. Transfusion of blood or any other blood products Consent taking process – It’s important that the informed consent is valid and hence following things must be ensured before taking consent from patient (or family) 1. Ensure that the patient is in right frame of mind to understand and interpret the information and able to make decision regarding consent. Patient should be conscious, not intoxicated, not in unsound state of mind and is 12 years or above 2. Ask if he/she would like to incorporate family members in decision making. This is the right of every patient 3. Explain the medical procedure for which consent is being required. Give as much information as required for the patient to be able to make decision. Following should necessarily be explained to patient a. Name of the procedure b. Purpose of the procedure or expected benefits of it c. Probability of expected result d. Name of the person who will perform the procedure e. Possible complication that may result due to the procedure f. Alternative treatments and their probable effects g. Prognosis of the disease if procedure not performed h. Risks involved in the procedure i. Any other relevant information 4. Patient and/or family should be explained in a language and manner that they can understand 5. Consent should be taken by the person who is going to perform the procedure or a member of his/her team 6. Consent should be taken before procedure is performed and within a reasonable time limit (either on the same day or on previous day). It should also be explained to patient that he/she may withdraw the consent any time before the procedure is initiated 7. If for some reason, the procedure could not be performed after taking consent, and is postponed to a later date, a fresh consent should be obtained from patient on the day or a day prior to the actual performance of procedure 8. If the patient has to undergo the procedure multiple time for lifelong or long time, for eg. Blood transfusion in Thalassemia patient, Haemodialysis, a fresh consent should be taken every time. However, this consent could be verbal. Once in six months (at a minimum) or whenever there is fresh information to be provided to the patient a fresh written consent shall be taken. 9. Consent should be taken in written by asking patient to sign the consent form which consist necessary information pertaining to the procedure, risks, benefits, alternatives and who will perform procedure 10. At-least one independent witness should be there when consent is being taken from the patient and his/her signature should also be taken on consent form 11. If the patient is illiterate his/her thumb impression should be taken along with the signature of two independent witnesses. 12. In case the patient is less than 18 years but above 12 years of age, signature of a parent/guardian should also be taken along with the signature of the child 13. Person taking the consent should also sign on the consent form Consent forms – This is the most important document for informed consent is the consent form. Separate forms may be required for separate clinical procedure. The form must contain sufficient details about the procedure to be performed, risks, benefit expected, alternatives available, risk if procedure not performed and likely complications if any. The form must also have place for identifiers, dates and signature of relevant parties. Click on the links below to get sample consent forms 1. Informed consent form – for common surgical procedures
- 21. 2. Informed consent form for Anaesthesia 3. Informed consent form for Blood or Blood Products Transfusion 4. Informed consent form for HIV testing 5. Informed consent form for Intensive Care 6. Informed consent form for Chemotherapy 7. Informed consent form for Dialysis 8. Advance Medical directive form ERA LUCKNOW MEDICAL COLLEGE AND HOSPITAL ERA UNIVERSITY 226003 TOPIC: DATE: VENUE: TRAINING TO BE ATTENDED BY : TRAINNER BY : TYPE OF TRAINING : Pricing of Hospital Services A Hospital offers a large number of clinical services and some non-clinical services as well. Patients availing these services can be Out-Patient, Emergency Patient or In-Patient. In-patient can further be of categorized as per their choice of accommodation, such as deluxe, semi-deluxe or general ward patient. Justified charging of services and facilities availed by different categories of patients can be confusing at times, as it requires a clear understanding of what services or components to be charged and how to differ the charges for different category of patient. In this post, a simplified explanation of how to price hospital services to charge it to patient, is presented. This will also help hospitals in developing a comprehensive document on hospital’s tariff and relevant policies for billing. In addition, you may also like to check this post on 'How much does it cost to run a hospital?' For pricing various services of a hospital, services can be grouped under following head. 1. OPD services 2. Emergency services 3. IPD services 4. ICU services 5. Surgical services 6. Medical/Surgical Procedures 7. Diagnostic services 8. Use of Medical Equipment 9. Materials and Consumables 10. Packaged services 11. Other services and facilities A brief description of each of these services group along-with how are they charged is described below.
- 22. 1. OUT-PATIENT SERVICES Most of these services are generally availed by an out-patient and includes following 1. First consultation fee – This fee can differ from specialist to specialist or from clinic to clinic and consultation fee of each specialist doctor/clinic should be specified. However, hospital can choose to have a policy of standardized rates. For example all speciality consultation at Rs. 500/- and Super-speciality consultation at Rs. 800/- 2. Follow up consultation fee – This can either be same as first time consultation fee or lesser. Many hospital also offer one free follow up consultation, if follow up is done within one week. This can also vary with individual specialist’s choice, if hospital allows for consultant specific pricing. 3. Day Care bed charges – Day care services are generally managed under OPD. The beds in day care are charged at per hour basis and for maximum of 12 hours. 4. Medical certificates – A rate for issuance of various types of medical certificates, such as fitness certificate, sickness certificate etc. can be specified 5. Medical/Surgical procedures, use of equipment and diagnostic services – These services, if used by OPD patient, should be charged as per their standard tariff for OPD patients. 6. Materials and consumables – These should be charged as per actual, not exceeding the MRP. 2. EMERGENCY SERVICES Patients’ seeking certain hospital services on emergency services can be charged on following components. 1. Emergency consultation fee: Generally charged at 1.5 to 2 times of first time consultation fee, specified in OPD. Another practice is to charge a fix fee for emergency (like Rs. 500/-) in addition to the first time consultation fee specified in OPD. Hospital should preferably not charge the patient for repeat visit to emergency if the patient is returning within specified duration (say 72 hours), with same presenting complaints. 2. Triage bed charges – Per hour basis 3. Emergency ward / Observation unit – Per hour basis. Maximum duration should be specified 4. Ambulance Charges – Ambulance services can be charged for per kilometre distance, with a fixed minimum charge. ALS and BLS ambulance can be charged at different rate. For example ALS ambulance at Rs. 35 per km, subject to minimum Rs. 2000 and BLS ambulance charged at Rs. 25 per km, subject to minimum Rs. 1200/-. If doctor or paramedical staff has to accompany the patient, there charges can be added additionally. 5. Medical/Surgical procedures, use of equipment and diagnostic services – These services, if used by emergency patient, should be charged as per their standard tariff for emergency patients. 6. Materials and consumables – These should be charged as per actual, not exceeding the MRP. 7. Note - As per the law, patients must be given life-saving treatment by the hospital, irrespective of payment 3. IN-PATIENTS SERVICES Following charges will be applicable on the patients getting admitted in hospital for any treatment 1. Accommodation charges – Per day charge, as per category of accommodation 2. Nursing charges – per day charge for each category of accommodation
- 23. 3. Assessment charges – This charge is applied toward detailed clinical assessment of the patient and the regular re-assessments during the duration of hospitalization 4. Consultant’s visit charges (professional charges) – Per visit charge of the consultant. This could vary from consultant to consultant, or hospital may choose to standardize the rates and differentiate the rates only on the basis of specialists and super-specialists consultant. The fee charged by a referred doctor should also be considered under this head. 5. Junior doctor’s visit fee – Per visit charge of the junior doctor. 6. Off hour visit charges – If the specialists visit is required outside the working hour of the doctor, a separate fee is charged, which is higher than the normal visit charge 7. Drug administration charges – This can be linked to the total medicine issued to the patient, for example 5% of the total cost of the medicine issued to the patient. Some hospital provide this as a part of nursing charges. 8. Medical Record Charges – To create and maintain the individual medical record of the patient (generally charged about 300-500 rs.) 9. Visitor Pass and Attendant Pass – Generally the visitor and patient’s attendant pass is issued free of cost, however, if the same is lost, a fee of Rs. 100 to Rs. 300 can be charged for re-issuing the same 10. Insurance claim support fee – A fixed or variable fee can be charged for carrying out insurance claim process or cashless process, if the patient is insured. This cost covers the photocopying and stationary cost and cost of the manpower involved in this. 11. Materials and consumables – These should be charged as per actual, not exceeding the MRP. 12. Medical/Surgical procedures, use of equipment and diagnostic services – These services, should be charged as per their standard tariff applicable for the category of accommodation in which the patient is admitted. Note – Hospital should have a policy on what charges will be applicable in case, the patient changes the category of accommodation during hospitalization period. Many hospital, charge the applicable price of the service for the category of accommodation in which the patient was admitted when the service was rendered. Some hospital, however, charge the services at the rate of highest category of accommodation in which the patient was admitted irrespective of category of accommodation in which the patient was staying when the service was rendered. Hospital also should have a policy on what charges should be applicable, if the category of accommodation required by patient is not available and hospital is offering another category temporarily, with an understanding of shifting the patient to his/her desired category as soon as it becomes available. Practice is that the patient is charged for the lower of the category sought and category offered, till the time patient is not transferred to the desired category. 4. ICU SERVICES These are applicable in case the patient had to avail intensive care services 1. Accommodation charge – Per day accommodation in ICU. This could differ depending upon type of ICU, like ICU, CCU, Burns ICU, Neonatal ICU, HDU etc. 2. Nursing Charges, Assessment charges, Consultant visit charges should be specified as is done in IPD, However the charges in ICU can be different and generally priced similar to one of the higher category of accommodation. 3. Ventilator Charges – Per hour and per day ventilator charges to be specified 4. Oxygen charges – Per hour and per day Oxygen charges to be specified. Oxygen charges are generally not applied for patients on ventilator
- 24. 5. Monitor charges – Per and per day basis 6. Other equipment charges – As per standard tariff of equipment used applicable to ICU category 7. Note – The hospital can have a policy on whether the patient be required to vacate the IPD accommodation when shifted to ICU. In case, IPD accommodation is retained, charges applicable for the same should be specified. Hospital can chose to charge at a higher price for retaining IPD accommodation, to discourage non-medical use of their rooms. 5. SURGICAL SERVICES Patient who undergo major surgeries as a part of their treatment, has to pay certain charges towards the surgical services availed by them. These charges typically include surgeon’s fee, operation theatre charges, Anaesthesiologist’s fee and materials cost. 1. Surgeon’s fee – The surgeon’s fee (primary surgeon) can differ from surgeon to surgeon and as per the level of surgery. Depending upon the risk and complexity, surgeries are classified into different levels. Surgeon’s fee is often linked to the level of surgery, with higher level demanding higher fee. 2. Assistant surgeon’s fee – If assistant surgeon is required, then a fee relative to the primary surgeon’s fee can be charged. For eg. 20% of the primary surgeon’s fee 3. Anaesthesiologist fee – This can be fixed, depending upon the type of anaesthesia. However, with increasing role of anaesthesiologists in patient safety, expertise and commitment of anaesthesiologist is becoming more and more important. Hence, there is a trend of linking the anaesthesiologist’s fee to the primary surgeon’s fee. Generally 25% to 35% of surgeon’s fee is charged as Anaesthesiologist’s fee. 4. Operation Theatre Charges – Operation theatre can be charged at an hourly rate and can vary with the type of operation theatre. Another way of charging operation theatre is as a percentage of Surgeon’s fee. Generally 75% to 100% is charged towards OT charges. 5. Charges in case of multiple procedure or multiple surgeon in one sitting – In surgeries that involves multiple procedures in one go, or requires more than one surgeon, a policy is necessary to determine the charges. Many hospital follow the rule on following lines In multiple procedures in one sitting, the procedure with highest surgeon’s fee is charged at 100%, second highest procedure at 50% and third procedure onwards at 25% of their tariff. Other linked charges, such as OT charges, Anaesthesia charges are calculated on the basis of total fee calculated for the primary surgeon In procedure involving two or more surgeons, the second or third surgeon’s fee is determined at a percentage of primary surgeon (like 25%). Other linked charges are only calculated on the basis of primary surgeon’s fee. 6. Surgical materials – The instruments and sterile packs used for surgery is generally covered under the operation theatre charges. However, things like stents and implants used in patient is charged as per actual cost, not exceeding the MRP. 6. MEDICAL/SURGICAL PROCEDURES A large number of medical procedures are carried out in hospitals. A standard tariff for each procedure (speciality wise) should be developed and used while billing a patient. For each procedure, the tariff applicable in OPD, Emergency, day care, ICU and IPD can vary and should be specified. Within IPD the tariff generally differs between categories of accommodation, with lower category charged at basic price and higher category are charged at premium price. 7. USE OF MEDICAL EQUIPMENT
- 25. Various type of equipment can be used on patient during his/her hospitalization, such as Alpha bed, CPAP, Incubator, Nebuliser, Syringe pump, water bed etc. For each equipment, the charges should be specified as per time use, per day or per hour, as applicable for the equipment. The charge can be different for OPD, Emergency, Day care, ICU, and various categories of IPD patients. 8. DIAGNOSTIC SERVICES A standard tariff should be available for all the tests available under Laboratory and Imaging department. Like medical procedures and equipment charges these can also differ for OPD, Emergency, Day care, ICU, and various categories of IPD patients. In addition, an additional fee can also be charged for carrying out a procedure bed-side, such as bed-side X-ray. 9. MATERIALS AND CONSUMABLES Various materials and consumables used on patient can be charged as per actual (not exceeding MRP), if not already included in package price or any other head. Generally the materials charges are not linked to the patient’s category of accommodation 10. PACKAGED SERVICES It is a trend to develop a package of certain services and offer it at a fixed price. Very commonly packages are developed for surgical treatments and for health check-ups. Surgical packages - These package price generally covers, all basic services that is required by patient to undergo surgery such as accommodation for specified number of days, medical assessment, investigations, surgery, basic drugs etc. It is important to clearly describe the inclusions and exclusions in the package, and conditions under which additional charges will become applicable. Health Check-up Packages. Health check-up is a highly sought after services from the hospital. A hospital can design various type of health check-up packages and specify a fixed price for the same. Inclusion and exclusion must be mentioned in such packages. 11. OTHER SERVICES AND FACILITIES Following are the other services and facilities that are offered by hospital and can be charged to patient, as per hospital’s policy. 1. One time registration fee – This is charged to the patient who has come to the hospital for the first time. This is to register the basic details and maintain the unique ID of the patient in hospital records. About 100 to 200 Rs. Can be charged for this. Some hospital also chose to offer free registration to patient. 2. Food for patients – Charges for routine food, special food, different types of restricted diets etc. 3. Food for patient’s attendant and visitors –According to type of food requested 4. Cafeteria charges – Item-wise prices 5. Telephone charge – For use of STD/ISD/Local calling using hospital’s phone 6. Internet Charges – Generally offered complimentary through WiFi 7. Mortuary charges – Per hour/Per day basis 8. Fee of allied health professionals – Physiotherapist, Dietitian, Occupational Therapists, etc. 9. Check this post on '6 things that can increase your hospital bill' to understand how hospital services pricing affects the cost to patient. Prepared by Dr.Anjalatchi Muthukumaran Vice principal
- 26. Era college of nursing
