INTUSSUCEPTION.pptx
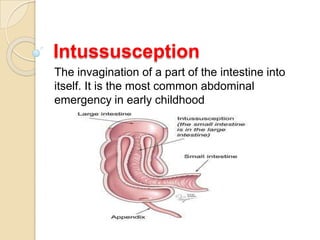
- 1. Intussusception The invagination of a part of the intestine into itself. It is the most common abdominal emergency in early childhood
- 3. EPIDEMIOLOGY Is the most common cause of intestinal obstruction in infants between 6 and 36 mnths of age. 60 % of children are younger than one year old, and 80 % are younger than two. Intussusception is less common before 3mo and after 6yr of age. Most episodes occur in otherwise healthy and well-nourished children. male:female ratio of 3:2.
- 4. PATHOGENESIS Occurs most often near the ileocecal junction (ileocolic intussusception). Ileo-ileo-colic, jejuno-jejunal, jejuno-ileal, or colo-colic. The intussusceptum, a proximal segment of bowel, telescopes into the intussuscipiens, a distal segment, dragging the associated mesentery with it. This leads to the development of venous and lymphatic congestion with resulting intestinal edema, which lead to ischemia, perforation, and peritonitis.
- 7. Idiopathic Approximately 75 % of cases are idiopathic because there is no clear disease trigger or pathological lead point most common in children between 3mo and 5yr of age.
- 8. Influence of viral factors illustrated by the following observations: ⚫ Has a seasonal variation, with peaks coinciding with seasonal viral gastroenteritis. ⚫ Associated with some forms of rotavirus vaccine. ⚫ 30 % experience viral illness (URTI, otitis media, flu-like symptoms) before the onset of intussusception. ⚫ A strong association with adenovirus infection . ⚫ Viral infections, including enteric adenovirus, can stimulate lymphatic tissue in the intestinal tract, resulting in hypertrophy of Peyer patches in the lymphoid-rich terminal ileum, which may act as a lead point for ileocolic intussusception . treatment with glucocorticoids has been suggested to prevent recurrence.
- 11. Other enteric infections Bacterial enteritis (Salmonella, E. Coli, Shigella, or Campylobacter). Most cases of intussusception occurred within the first month after the bacterial enteritis.
- 12. Lead point A lead point is a lesion or variation in the intestine that is trapped by peristalsis and dragged into a distal segment of the intestine, causing intussusception. A Meckel diverticulum, polyp, tumor, hematoma, or vascular malformation can act as a lead point for intussusception.
- 13. Underlying disorders 25 % of cases( a pathological lead point), which may be focal or diffuse. Such triggers greater in children younger than 3MO or older than 5Yr. Meckel diverticulum, polyps, small bowel lymphoma, duplication cysts, vascular malformations, inverted appendiceal stumps, parasites (eg, Ascaris lumbricoides), Henoch-Schönlein purpura, cystic fibrosis, and hemolytic- uremic syndrome. Meckel diverticulum is the most common, followed by polyps, and then either duplication cysts or Henoch-Schönlein purpura.
- 14. The mechanisms leading to intussusception : ⚫ Meckel diverticulum, polyps, duplication cysts, lymphomas, areas of reactive lymphoid hyperplasia, or other focal abnormalities of the intestinal tract act as lead points, dragging the intestine into a distal segment of intestine. ⚫ With Henoch-Schönlein purpura, a small bowel wall hematoma acts as the lead point. Intussusception typically occurs after resolution of the abdominal pain. ⚫ cystic fibrosis( thick inspissated stool may act as the lead point). ⚫ celiac disease ( dysmotility and excessive secretions or bowel wall weakness). ⚫ Patients with Crohn disease ( inflammation and stricture formation).
- 17. ⚫ Postoperative — (usually jejuno-jejunal or ileo- ileal) is thought to be caused by uncoordinated peristaltic activity and/or traction from sutures or devices. Affected patients typically do well for several days and may even resume oral intake before developing symptoms of mechanical obstruction. The diagnosis can be difficult to establish because intussusception may be confused with postoperative paralytic ileus. Evaluation with ultrasonography or (CT) scanning can establish the diagnosis, monitor for spontaneous reduction, and help to predict which children are likely to need surgical reduction. Because most cases of postoperative intussusception occur in the small intestine, contrast enemas do not usually contribute to the diagnosis.
- 19. CLINICAL MANIFESTATIONS sudden onset of intermittent, severe, crampy, progressive abdominal pain, accompanied by inconsolable crying and drawing up of the legs toward the abdomen. The episodes usually occur at 15 to 20 min intervals. They become more frequent and more severe over time. Vomiting may follow episodes of abdominal pain. Initially, emesis is non-bilious, but it may become bilious as the obstruction progresses. Between the painful episodes, the child may behave relatively normal and be free of pain. As a result, initial symptoms can be confused with gastroenteritis. As symptoms progress, increasing lethargy develops, which can be mistaken for meningoencephalitis. A sausage-shaped abdominal mass may be felt in the right side of the abdomen. In up to 70 %of cases, the stool contains gross or occult blood. The stool may be a mixture of blood and mucous, giving it the appearance of currant jelly.
- 20. ⚫ ⚫ ⚫ classically ( pain, a palpable sausage-shaped mass, and currant-jelly stool) is seen in less than 15 % of patients at the time of presentation. 20 % of young infants have no obvious pain. 1/3 of patients do not pass blood or mucus, nor do they develop an abdominal mass. Many older children have pain alone without other signs or symptoms. Occasionally, the initial presenting sign is lethargy or altered consciousness alone, without pain, rectal bleeding, or other symptoms that suggest an intraabdominal process. This clinical presentation primarily occurs in infants and is often confused with sepsis. Thus, intussusception should be considered in the evaluation of otherwise unexplained lethargy or altered consciousness, especially in infants. An intussusception is sometimes discovered incidentally during an imaging study performed for other reasons or for nonspecific symptoms. If these intussusceptions are short and if the patient has few symptoms, they may not require intervention
- 21. DIAGNOSIS ⚫ Depends on the clinical suspicion for intussusception (typical or atypical presentation) and experience radiologists. ⚫ Patients with a typical presentation (sudden onset of intermittent severe abdominal pain with or without rectal bleeding) or characteristic findings on radiography, may proceed directly to nonoperative reduction using hydrostatic (contrast or saline) or pneumatic (air) enema, performed under either sonographic or fluoroscopic guidance. In these cases, the procedure is both diagnostic and therapeutic. ⚫ If diagnosis is unclear at presentation. In this case, initial workup may include abdominal ultrasound or abdominal plain films. If the study supports the diagnosis of intussusception, nonoperative reduction is then performed.
- 22. Ultrasonography Is the method of choice to detect intussusception. The sensitivity and specificity approach 100 % in the hands of an experienced. US is better than fluoroscopic in detect pathological lead points , monitor the success of a reduction , not expose the patient to radiation ⚫ The classic ultrasound image is a "bull's eye" or "coiled spring" lesion representing layers of the intestine within the intestine (picture 2). In addition, a lack of perfusion in the intussusceptum detected with color duplex imaging may indicate ischemia. US can diagnose the rare ileo-ileal intussusception and identify the lead point of intussusception 2/3of cases .
- 24. ⚫US features for small bowel intussusception include location of the intussusception in the paraumbilical or left abdominal region and/or lesion size ≤3 cm; in such cases, evaluation with a CT scan may help to confirm the location of the intussusception and whether there is a lead point. In small bowel intussusceptions, the length of the intussusceptum, as measured by ultrasound or CT, helps determine prognosis and management.
- 25. Abdominal plain film Plain radiographs of the abdomen are less sensitive and less specific than ultrasonography for the diagnosis of intussusception, but are often performed as part of the evaluation of patients with abdominal symptoms. Radiographic features include signs of intestinal obstruction, massively distended loops of bowel with absence of colonic gas (picture 3).
- 27. Other findings may be seen: ⚫ A target sign, consisting of two concentric radiolucent circles superimposed on the right kidney, represents peritoneal fat surrounding and within the intussusception. This finding appeared in 26 % of patients. ⚫ A soft tissue density projecting into the gas of the large bowel (representing the intussusception) is called the "crescent sign." ⚫ An obscured liver margin ⚫ Lack of air in the cecum, which prevents its visualization ⚫ pneumoperitoneum suggests that bowel perforation has occurred. ⚫ The presence of air in the cecum on at least two views had high sensitivity for excluding intussusception with a low clinical suspicion . ⚫ more than 20 % of patients with intussusception had negative plain films.
- 28. CT scan However, CT cannot be used to reduce the intussusception and can be time-consuming in children who may require sedation. Thus, CT generally is reserved for patients in whom the other imaging modalities are unrevealing, or to characterize pathological lead points for intussusception detected by ultrasound.
- 29. TREATMENT Stable patients with a high clinical suspicion and/or radiographic evidence of intussusception and no evidence of bowel perforation should be treated with nonoperative reduction. ⚫ Surgical treatment is indicated in acutely ill or perforation. radiographic facilities and expertise to perform nonoperative reduction are not available. nonoperative reduction is unsuccessful, or for evaluation or resection of a pathological lead point. intussusception limited to the small bowel (ileo-ileal, jejuno-ileal, or jejuno-jejunal).
- 30. Nonoperative reduction ⚫ using hydrostatic or pneumatic pressure by enema has high success rates in children with ileocolic intussusception, and is the treatment of choice for a stable child and radiologic facilities are available. contridication ;long duration of symptoms and/or suspected bowel perforation. ⚫ Patient should be stabilized and resuscitated with IVF, and the stomach decompressed with a nasogastric tube. Because there is a risk of perforation during nonoperative reduction, the surgical team should be notified and steps should be taken to ensure that the patient is fit for surgery. ⚫ Antibiotics administered before attempting nonoperative reduction because of the risk of perforation.
- 31. ⚫ After successful reduction, a temperature higher than 38ºC because of bacterial translocation or the release of endotoxin or cytokines. risk to develop recurrent intussusception in the near term, possibly because of residual bowel inflammation, which may itself act as a lead point. Patient should be observed in the hospital for 12 to 24 hours. Nasogastric suction usually is maintained until bowel function has returned and the patient has had passage of a bowel movement. Feedings then are advanced as tolerated.
- 32. Fluoroscopic or sonographic guidance Reduction is typically performed under fluoroscopic guidance, using either hydrostatic (contrast) or pneumatic (air) enema. Has high success rates (80 to 95 %) and is an appropriate choice if the treating physicians have more experience with this technique than with ultrasound-guided reduction.
- 34. Successful reduction ; 1. free flow of contrast or air into the small bowel. Reduction is complete only when a good portion of the distal ileum is filled with contrast. 2. Relief of symptoms and disappearance of the abdominal mass. A characteristic sound also may be appreciated with auscultation. 3. In occasional patients, the contrast material does not reflux freely into the small bowel even with a complete reduction, however a successful reduction is suggested by lack of a filling defect in the cecum (apart from the ileocecal valve), and clinical resolution of symptoms and signs. A post-reduction filling defect in the cecum commonly is seen, probably the result of residual edema in the ileocecal valve. However, this finding cannot be distinguished from a focal lead point by radiologic examination alone. As a result, a repeat study or even laparotomy may be indicated if there is any concern of a focal lead point.
- 35. ⚫ Barium a water-soluble contrast enema is preferred because of the risk of perforation before or during the procedure. reduce the risk of electrolyte disturbances and peritonitis in patients in whom perforation has occurred. sonographic guidance, and is now the intervention of choice for ileocolic intussusception in many institutions. ⚫ air or saline enemas. Signs of successful reduction with saline include the disappearance of the intussusception and the appearance of water and bubbles in the terminal ileum. ⚫ Ultrasound-guided have a success rate of 80 to 95 % for most types of intussusception, which is comparable to those of fluoroscopic techniques. The main advantage of ultrasound-guided reduction is avoidance of radiation exposure and improved detection of pathological lead points as compared to fluoroscopic techniques.
- 36. Hydrostatic technique — The standard method of reduction is to place a reservoir of contrast 1 meter above the patient so that constant hydrostatic pressure is generated. With experience (and depending upon the clinical status of the patient), a physician may undertake a more aggressive reduction. When hydrostatic reduction is performed under ultrasonographic guidance, normal saline is used for the enema.
- 37. Pneumatic technique — Air reduction techniques have gained popularity as an alternative to the hydrostatic methods, and can be used under either ultrasonographic or fluoroscopic guidance (picture 5). Air enemas reduce the intussusception more easily, and may be advantageous if perforation occurs.
- 39. The technique begins with insertion of a Foley catheter into the rectum. Fluoroscopy or ultrasound is used to monitor the procedure. Air is then instilled until the intussusceptum is pushed back gently, taking care to avoid excessive pressure. A sphygmomanometer can be used to monitor colonic intraluminal pressure (typically not to exceed 120 mm Hg) to aid in reduction. Carbon dioxide can also be used instead of air. It has the advantage of being absorbed rapidly from the gut, is associated with less discomfort, and is less dangerous than air, which potentially could cause an air embolism (although air embolisms have not been reported). ⚫ Reflux of air into the terminal ileum and the disappearance of the mass at the ileocecal valve usually indicates reduction (picture 6A-B). If fluoroscopy is used, water-soluble contrast material can be instilled to confirm the reduction, or the air reduction can be repeated if the completeness of reduction is questioned.
- 42. Risk and complications ⚫ perforation of the bowel 1 %. on distal side of the intussusception, often in the transverse colon, and commonly where the intussusception was first demonstrated by radiographic studies. Risk factors ; age younger than 6mo. long duration of symptoms (eg, 3 days or longer). evidence of small bowel obstruction. use of higher pressures during the reduction. Should not be attempted in prolonged symptoms or any signs of peritoneal irritation or free peritoneal air. ⚫ The pneumatic reduction provides an advantage if perforation occurs, because air is generally less harmful. When perforation is noted with air reduction, the colonic wall tears are smaller than those observed with the hydrostatic contrast techniques, and peritoneal pathology tends to be minimal. Needle decompression of the abdomen may be necessary if the excess air in the peritoneal cavity compromises the patient's respiratory status.