Rheumatology.pdf
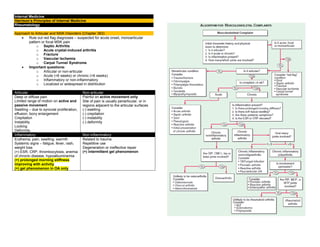
- 1. Internal Medicine Harrison’s Principles of Internal Medicine Rheumatology Approach to Articular and MSK Disorders (Chapter 363) Rule out red flag diagnoses – suspected for acute onset, monoarticular pattern or focal MSK pain o Septic Arthritis o Acute crystal-induced arthritis o Fracture o Vascular Ischemia o Carpal Tunnel Syndrome Important questions: o Articular or non-articular o Acute (<6 weeks) or chronic (>6 weeks) o Inflammatory or non-inflammatory o Localized or widespread in distribution Articular Non-articular Deep or diffuse pain Limited range of motion on active and passive movement Swelling – due to synovial proliferation, effusion, bony enlargement Crepitation Instability Locking Deformity Painful on active movement only Site of pain is usually periarticular, or in regions adjacent to the articular surfaces (-) swelling (-) crepitation (-) instability (-) deformity Inflammatory Non-inflammatory Erythema, pain, swelling, warmth Systemic signs – fatigue, fever, rash, weight loss (+) ESR, CRP, thrombocytosis, anemia of chronic disease, hypoalbuminemia (+) prolonged morning stiffness improving with activity (+) gel phenomenon in OA only Related to trauma Repetitive use Degeneration or ineffective repair (+) intermittent gel phenomenon
- 2. Clinical History Younger age group SLE, reactive arthritis Middle age group Fibromyalgia RA Elderly age group OA Polymyalgia rheumatica Men Gout Spondyloarthritis Ankylosing spondylitis Women RA Fibromyalgia Osteoporosis SLE African American Sarcoidosis SLE Whites Polymyalgia rheumatic Giant cell arteritis Granulomatosis with polyangiitis Familial aggregation Ankylosing spondylitis Gout Heberdon nodes of OA Onset Abrupt onset Septic arthritis,Gout Indolent onset OA, RA, fibromyalgia Evolution Chronic OA Intermittent Crystal-induced, Lyme arthritis Migratory RF, gonococcal, viral arthritis Additive RA, Psoriatic arthritis Evolution Chronic (>6 weeks) OA, RA, fibromyalgia Acute (<6 weeks) Infectious, crystal-induced, reactive Extent or Distribution Mono articular (1 joint) Crystal-induced, infectious Oligoarticular (2-3 joints) Poly articular (4 or more joints) OA, RA (symmetric as well) Asymmetric and polyarticular Spondyloarthritis, reactive arthritis, gout, sarcoid Symmetric or asymmetric Polyarticular or oligoarticular OA, psoriatic arthritis Upper extremities RA, OA Lower extremities Gout, reactive arthritis Axial skeleton OA, ankylosing spondylitis RA of the cervical spine Diseases with MSK co-morbidities Diabetes mellitus Carpal tunnel syndrome Renal insufficiency Gout Depression or insomnia Fibromyalgia Myeloma Low back pain Cancer Myositis Osteoporosis Fracture Glucocorticoids Osteonecrosis Septic arthritis Diuretics or chemotherapy Gout Rheumatic Review of Systems Fever SLE, infection Rash SLE, psoriatic arthritis Nail abnormalities Psoriatic arthritis, reactive arthritis Myalgias Fibromyalgia, statin-induced, drug-induced Weakness Polymyositis, neuropathy Eye involvement Behcet, sarcoidosis, Spondyloarthritis Gastrointestinal Scleroderma, IBD Genitourinary Reactive arthritis, gonococcemia Nervous system Lyme disease, vasculitis
- 5. Osteoarthritis (Chapter 364) Most common type of arthritis Joints commonly affected by arthritis: Definition Defined as joint failure → hyaline articular cartilage loss present in a focal and initially nonuniform manner → thickened subchondral bony plate, outgrowth of osteophytes at the joint margin, stretching of the articular capsule, snynovitis, weakness of the muscles bridging the joint Joint Protective Mechanisms and their Failure Joint protectors – joint capsule, ligaments, muscles and tendons, afferent sensory nerves, underlying bone Charcot arthropathy – severe and rapidly progressive OA developing when minor injury occurs in the presence of posterior column peripheral neuropathy Joint capsule and ligaments Fixes range of motion Synovial fluid lubrication Hyaluronic acid, lubricin Bridges the joint Muscles and tendons Cartilage and its Role in Joint Failure Two most important macromolecules in cartilage: Type 2 collagen Provides cartilage tensile strength Aggrecan Proteoglycan macromolecule linked with hyaluronic acid molecule, with highly negatively charged glycosaminoglycans Through electropulsion → gives cartilage compressive stiffness OA cartilage o (+) gradual depletion of aggrecan o (+) unfurling of the tightly woven collagen matrix o (+) loss of type 2 collagen Risk Factors 2 major factors contributing to OA development: o Joint vulnerability o Joint loading Systemic Risk Factors Age Most potent risk factor for osteoarthritis Rare in <40 yearsold >50% in >70 years old Aging increases joint vulnerability – less responsive in matrix synthesis, thinner cartilage with age, weaker bridging muscles, slower nerve conduction, stretching of ligaments Older women Especially in their sixth decade Probably hormonal loss Heritability and genetics Highly heritable disease, but joint specific (+) polymorphism with GDF5 gene Race Knee OA is more common among Chinese Risk Factors in the Joint Environment Joint anatomy 3 uncommon developmental abnormalities occurring in utero or in childhood: Congenital dysplasia Legg-Perthes disease Slipped capital femoral epiphysis Others: acetabular dysplasia, femoroacetabular impingement Major injuries Fracture through the surface Avascular necrosis Tears of ligamentous and fibrocartilaginous structures Meniscal tears Joint misalignment
- 6. Varus knees – cartilage loss in the medial or inner knee Valgus knees – cartilage loss in the lateral compartment Weakness of the quadriceps – knee OA Loading Factors Obesity 3-6 times body weight is transmitted across the knee during a single-leg stance Well-recognized and potent risk factor for OA (esp. knee) Precedes the development of disease More potent in women Adipokines may also be contributory Repeated Use of Joint and Exercise Seen in occupational use and leisure time physical activities Farmers – hip OA Miners – knee and spine OA Heavy carrying – knee OA Elite runners – knee and hip OA Recreational runners – hip OA Pathology Non-uniform loss in cartilage in a focal disease Thickening of the subchondral bony plate Osteophyte formation – outgrowth of new cartilage that ossifies o Important radiographic hallmark of OA Stretching of the capsule → edematous and fibrotic Sources of Pain Likely occurs from structures outside the cartilage (aneural): o Synovium, ligaments, joint capsule, muscles, subchondral bone Severity of X-ray changes correlate poorly with pain severity Presence of MRI synovitis correlates with presence and severity of knee pain Clinical Features Joint pain o During or just after joint use and then gradually resolves o As disease progresses, pain becomes continuous and even becomes bothersome at night Morning stiffness o Usually brief (<30 minutes) Knee symptoms o Most common cause of chronic knee pain in patients >45 years o (+) knee buckling – from weakness of muscles crossing over the joint Buckling, catching, locking Anterior crucial ligament or meniscal tear Needs to be evaluated after a knee injury Pain during knee flexion (>35 degrees) From the patellofemoral compartment Prolonged morning stiffness with many joints affected Inflammatory arthritis Pain medial and distal to the knee Anserine bursitis Common cause of knee pain, responsive to glucocorticoid injection Prominent nocturnal pain in the absence of end-stage OA Merits diagnostic work-up Hip symptoms o Can be detected by loss of internal rotation by passive movement, pain isolated to an area lateral to the hip joint (trochanteric bursitis) Diagnostics No blood tests are routinely indicated for workup of patients with OA, unless symptoms and signs suggest inflammatory arthritis Examination of synovial fluid >1000 WBC/uL – presence of inflammatory arthritis or crystal-induced arthritis (with presence of crystals) X-rays Indicated when joint pain and physical findings are atypical of OA, or if pain persists after initiation of pain treatment Radiographs may be normal in early disease as they are insensitive to cartilage loss and early findings MRI Not indicated as part of diagnostic workup Almost never warrant change in therapy Goal of Treatment Goal of treatment: To alleviate pain and minimize loss of physical function Most effective mode of treatment: nonpharmacological treatment Non-pharmacological Treatment Goals of treatment: o Avoiding painful activities – simplest treatment o Improving strength and conditioning of muscles bridging the joints o Unloading the joint via use of braces or splint to redistribute load or unloading joint during weight bearing with a cane or crutch Exercise o Inactivity leads to increased risk for CVD and obesity o Weakness in muscles have multiple etiologies: Decline in strength with age Disuse muscle atrophy due to limitation of movement Diminishing muscle use due to alteration of gait Due to arthrogenous inhibition o Weakness in a muscle makes joint more susceptible to further damage and pain o Exercise lessens pain and improves physical function o Major challenge – adherence to program o Strongest predictor of success – personal history of successful exercise
- 7. Effective Exercise Non-effective Exercise Aerobic exercises Resistance training Low-impact exercises (water aerobics) Tai chi – effective for knee OA Exercise with caloric restriction Range-of-motion exercises Isometric exercises Correction of misalignment o Via bracing for willing patients who can learn to put them on correctly and on whom they do not slip o Acupuncture o Surgery Pharmacological Treatment Serves as an important adjunct therapy for OA Acetaminophen (Paracetamol) Up to 1 gram TID Initial analgesic of choice for patients with OA Prolongs half-life of warfarin NSAIDs Most popular drugs to treat osteoarthritic pain Either topically or orally 30% greater pain alleviation than high-dose paracetamol Important to take low-dose aspirin and iburprofen/naproxen at different times to limit drug interaction – may increase bleeding and GI complaints Side effects: GI complaints (should be taken after meals) If with high-risk, take PPIs Others: edema, renal insufficiency (used with caution for CKD III) NSAIDS with increased CVD risk – diclofenac, rofecoxib Allowed NSAIDs – Naproxen (with high GI toxicity), salsalate, ibuprofen, celecoxib Topicals – lesser efficacy, less GI and systemic side effects but may cause skin irritation Intraarticular injections – glucocorticoids May be used temporarily (less than 3 months) for pain alleviation since synovitis is correlated with joint pain severity Subsequent injections may cause minor amounts of cartilage loss with unimportant clinical consequences Hyaluronic acid injections Can be given as treatment but with controversy on efficacy over placebo Opioid analgesics Has modest efficacy Duloxetine Has modest efficacy Glucosamine Chondroitin Recommended against OA Surgery Arthroscopic menisectomy Indicated for acute meniscal tears in which symptoms such as locking and acute pain are clearly related temporally to a knee injury that produced the tear High tibial osteotomy For patients with knee OA to the medial compartment Total knee or hip arthroplasty Highly efficacious operations that relieve pain and improve function in majority of patients Failure rates of 1% per year (higher in obese patients) Success rates higher in hips > knees Timing of knee or hip replacement is critical Cartilage regeneration, abrasion arthroplasty (chondroplasty) Not found to be efficacious in OA May be efficacious when OA has not yet developed Ineffective surgical plans Arthroscopic debridement and lavage Partial menisectomy
- 8. Gout and Other Crystal-induced Arthropathies (Chapter 365) Gout Metabolic diseases mostly affecting o Middle-aged to elderly men o Postmenopausal women Due to increased body pool of urate with hyperuricemia → deposition of MSU crystals in joints and CT tophi with risk for deposition in the kidney interstitium or uric acid nephrolithiasis Clinical Features Involved joints MTP1, tarsal joints, ankles, knees, finger joints (usually in the elderly) First episode Begins at night with dramatic joint pain and swelling – mimicking cellulitis Precipitating events Dietary excess, trauma, surgery, excessive ethanol ingestion, hypouricemic therapy, serious medical illnesses – MI and stroke Presentation in women Represents 5-20% of the population (+) osteoarthritis and arterial hypertension → mild renal insufficiency (+) receiving diuretics Laboratory Diagnosis Needle aspiration of acutely or chronically involved joints or tophaceous deposits Confirms presumptive diagnosis (+) negative birefrigent needle-shaped crystals in compensated polarized light intracellularly and extracellularly Synovial fluid leukocyte counts More than 2,000 to 60,000/uL Culture If suspected to have septic arthritis Serum uric levels Can be normal or low at the time of an acute attack – inflammatory cytokines can be uricosuric and effective initiation of hypouricemic therapy can precipitate attacks Serum urate levels Almost always elevated at some time Important to use follow the course of hypouricemic therapy 24-h uric acid Useful in assessing risk of stones, elucidating overproducers or underexcretors of uric acid – to decide if uricosuric therapy is appropriate Excretion of >800 mg uric acid per day on regular diet – suggests overproduction of purine Other tests Urinalysis Serum creatinine Hemoglobin WBC count Liver function tests Serum lipids To assess possible pathologic sequelae of gout and other associated diseases requiring treatment and as baselines because of possible adverse effects of gout treatment Radiographic features X-ray (+) cystic changes, well-defined erosions with sclerotic margins (with overhanging bony edges) (+) soft tissue masses – advanced chronic tophaceous gout Ultrasound (+) double contour sign overlying articular cartilage Dual-energy CT (+) presence of urate crystals Treatment Acute Gouty Arthritis NSAIDs and colchicine – may be poorly tolerated and dangerous in the elderly, especially in the presence of renal insufficiency and GI disorders Ice pack applications and rest of involved joints can be helpful Oral colchicine Traditional and effective treatment if used early in an attack Regimens: 0.6 mg given every 8 hours with subsequent tapering 1.2 mg followed by 0.6 mg in 1 hour with subsequent day dosing depending on response Temporarily discontinued promptly at the first sign of loose stools, and symptomatic treatment of diarrhea must be given Oral NSAIDs Effective in 90% of patients With resolution of signs and symptoms after 5-8 days Most effective are those with short-half-lives: Celecoxib (800 mg – 400 mg 12 hour after, then 400 mg BID) Diclofenac (50 mg TID) Ibuprofen (800 mg TID) Naproxen (500 mg BID) Indomethacin (25-50 mg TID)
- 9. Intramuscular or oral glucocorticoids Oral: prednisone 30-50 mg/day as initial dose → gradually tapered with resolution of attack May be effective in polyarticular gout Intraarticular: triamcinolone acetonide 20-40 mg, or methylprednisolone 25-50 mg Anakinra IL-1 antagonist Has an essential role on the inflammasome Used when other treatments have failed or contraindicated Hypouricemic Therapy Ultimate control – correction of hyperuricemial Normalized serum uric acid: <300-360 umol/L (5.0 – 6.0 mg/dL) o To prevent recurrent gouty attacks and eliminate tophaceous deposits Considered when hyperuricemia cannot be corrected by: o Control of body weight o Low-purine diet o Increase in liquid intake o Limitation of ethanol use o Decreased use of fructose-containing foods and beverages o Avoidance of diuretics Indications o Increased number of acute gouty attacks o Serum uric acid of >535 umol/L (>9.0 mg/dL) o Willingness to commit to lifelong therapy o Presence of uric acid stones o Presence of tophi or chronic gouty arthritis Not initiated during acute attacks, but after patient is stable Low-dose colchicine has been initiated to decrease risk of flares o Colchicine prophylaxis in doses of 0.6 mg one to two timed daily – should be given along with Hypouricemic therapy until patient is normouricemic and without gouty attacks for 6 months, or as long as tophi are present o Not used in patients in dialysis, given in lower doses to patients with renal disease or with P glycoprotein or CYP3A4 inhibitors (clarithromycin) Probenecid Uricosuric agent used in patients with good renal function who underexcrete uric acid <600 mg/day Urine volume is maintained by ingestion of 1500 mL water/day Regimen 250 mg BID → gradually to 3 g per day Not effective in those with serum creatinine levels of >2 mg/dL - May require allopurinol or benzbromarone Benzbromarone Uricosuric agent more effective for patients with CKD Lesinurad New uricosuric agent that can be used as an adjuvant at 200 mg/day to a xanthise oxidase inhibitor Others with mild uricosuric Losartan, amlodipine, fenofibrate effects Allopurinol Xanthine oxidase inhibitor Most commonly used Hypouricemic agent Best drug to lower serum urate in overproducers, urate stone formers, patients with renal disease Regimen Single morning dose of 100 mg (up to 800 mg as needed) Adjusted initial dose depending on creatinine clearance (10 mL/min = 100 mg) Toxicity among: (+) penicillin and ampicillin allergies (+) thiazide diuretic users Asians with HLA-B*58:01 Serious side effects: TEN, systemic vasculitis, bone marrow suppression, granulomatous hepatitis, renal failure With mild cutaneous reactions Can shift to uricosuric agent, desentiziation to allopurinol, use of febuxostat Febuxostat Xanthine oxidase inhibitor (40-80 mg OD) Does not require dose adjustments with mild-moderate renal disease Pegloticase Pegylated uricase Available for patients who do not tolerate or fail full doses of other treatment IV 8mg every 2 weeks can dramatically lower serum uric acid to up to 50% Other Cyrstal-induced arthritis Calcium pyrophosphate deposition (CPPD) disease Definitive Diagnosis (+) rhomboid or rodlike, weakly positive or nonbirefrigent with polarized light Others: (+) linear calcifications Calcium apatite deposition disease (basic calcium phosphate disease) Definitive Diagnosis: (+) seen in EM – 1-20 um shiny intra or extracellular nonbirefrigent globules or aggregates (+) purplish in Wright’s stain (+) bright red in alizarin red S. Others: (+) intra or periarticular calcifications with or without erosive, destructive, or hypertrophic changes Calcium oxalate disease Definitive Diagnosis: (+) bipyramidal and small polymorphic crystals in light microscopy Primary oxalosis – rare metabolic disease Secondary oxalosis – mainly due to chronic renal failure, more common than primary
- 10. Rheumatoid Arthritis (Chapter 351) Most common form of chronic inflammatory arthritis Clinical Features Increases between 25 and 55 years of age, plateaus until 75 years and declines after Undifferentiated inflammatory arthritis – too few affected joints to be classified as RA; if diagnosed later as RA: o Higher number of tender and swollen joints o Tests positive for RF and anti-CCP antibodies o Higher scores for physical disability Early morning stiffness Lasting more than 1 year, eases with physical activity Earliest involved joints Small joints of the hands and feet: Wrists, MCP, PIP joints DIP joint involvement Manifestation of coexistent osteoarthritis Flexor tendon tenosynovitis Frequent hallmark of RA → decreased range of motion → reduced grip strength and trigger fingers Ulnar deviation Subluxation of the MCP joints with subluxation of the proximal phalanx to the volar side of the hand Swan-neck deformity Hyperextension of the PIP Flexion of the DIP Boutonniere deformity Flexion of the PIP Hyperextension of the DIP Z-Line deformity Subluxation of the MCP1 Hyperextension of the IP1 Piano-key movement of the ulnar styloid Subluxation of the distal ulna – because of inflammation of the ulnar styloid and tenosynovitis of the extensor carpi ulnaris Flat feet (pes planovalgus) Chronic inflammation of the ankle and midtarsal region Atlantoaxial involvement May cause compressive myelopathy and neurologic dysfunction Rarely affects thoracic and lumbar spine TMJ involvement Not associated with significant symptoms Extraarticular Manifestations May develop in 40% of patients – even before onset of RA Most likely develop among patients: o History of cigarette smoking o Early onset of significant physical disability o (+) RF and anti-CCP antibodies Constitutional symptoms Weight loss, fatigue, malaise, depression, cachexia Presence of fever >38.3 C – suspect for Vasculitis or infection Subcutaneous nodules Firm non-tender, adherent to the periosteum, tendonds or bursae More common (30-40%) in those with highest levels of disease activity, disease-related shared epitope (SE), (+) RF, radiographic evidence of joint erosions Locations: forearm, sacral prominences, Achilles tendon Others: lungs, pleura, pericardium, peritoneum Sjogren syndrome (10%) (+) keratoconjunctivitis sicca (dry eyes) (+) xerostomia (dry mouth) Pulmonary manifestations Most common pulmonary manifestation - pleuritis (+) pleuritic chest pain, dyspnea (+) pleural friction rub, effusion (exudative) Insterstitial lung disease – with high disease acitivity, smokers – diagnosed via CT scan Usual interstitial pneumonia (UIP), non-specific interstitial pneumonia (NSIP) – main histological and radiologic patterns of ILD Poor prognosis (10% risk for mortality) Favors more than idiopathic ILD More responsive to immunosuppressive therapy Caplan syndrome (+) pulmonary nodulosis (+) pneumoconiosis (+) silica exposure (+) rheumatoid arthritis Cardiac Pericardium – most common site of involvement MR – most common valvular abnormality in RA Vasculitis Mostly seen in the following: - Long-standing disease - Positive for RF, anti-CCP - Hypocomplementemia Sensory polyneuropathies (Mononeuritis multiplex) may occur Hematologic Normochromic, normocytic anemia – MC hematologic abnormality Felty’s syndrome (occurs in late stages of RA) Neutropenia, splenomegaly, nodular RA T-cell LGL May have similar presentation with Felty May occur early in disease Lymphoma DLBCL – most common lymphoma
- 11. Associated Conditions CVD – most common cause of death in RA o Due to chronic inflammation Osteoporosis – more common in RA patients Hypoandrogenisms Epidemiology TNF-alpha Major cytokine in RA HLA-DRB1 HLA associations PTPN22 Non-MHC gene with strong risk for RA Smoking Most reproducible environmental risk factor for RA Porphyromonas gingivalis EBV Associated infections with RA Pathology Pathologic hallmarks Synovial inflammation and proliferation (pannus) Focal bone erosions Thinning of articular cartilage Most common inflammatory infiltrate T cells – driving chronic inflammatory response Diagnosis Clinical diagnosis of RA is largely based on the following: o Clinical presentation of chronic inflammatory arthritis o Laboratory and radiographic results Anti-CCP (ACPA) Has greater specificity for RA diagnosis than RF Laboratory Features Serum IgM RF Found in 75-80% of patients with RA Also found in: Primary Sjogren, SLE, type II mixed essential cryoglobulinemia Subacute BE, hepatitis B and C 1-5% in healthy population ACPA Same sensitivity with IgM RG 95% specificity (more useful in diagnosis) Most predictive for predicting worse outcomes SF analysis WBC count – 5,000-50,000 WBC/uL (vs <2,000 in osteoarthritis) Predominance of neutrophil Purpose Most useful in confirming an inflammatory athritis while excluding infection or crystal-induced arthritis Joint imaging Purpose not only for diagnosis, but also for tracking progression of joint damage MRI, UTZ – preferred diagnostic modalities X-ray Periarticular osteopenia – initial radiographic finding Other findings: ST swelling, symmetric joint space loss, subchondral erosions (MCPs, PIPs, MTPs – lateral aspect of 5 th MTP – most common target) MRI Offers greatest sensitivity for detecting Synovitis and joint effusions, and early bone and bone marrow changes UTZ Can detect more lesions than X-ray but operator-dependent Clinical Course Natural history is mainly affected by: o Age of onset, gender, genotype, phenotype, comorbid conditions 10% patients Will undergo spontaneous remission within 6 months Especially Seronegative patients IHD Most common cause of death Shortening of median life expectancy 7 years less in men 3 year less in women Risk factors With systemic EA involvement, low functional capacity, low socioeconomic status, low education, chronic prednisone use Joint inflammation Main driver of joint damage, most important cause of functional disability in earlier stages
- 12. Treatment of RA Development trends in management of RA (1) Emergence of methotrexate as DMARD of first choice for early RA (2) Development of novel biologicals that can be used alone or in combination with methotrexate (3) Proven superiority of combination DMARD regimens over methotrexate alone Medications used in RA o NSAIDS o Glucocorticoids o Conventional DMARDs o Biological DMARDs NSAIDs Presently considered as adjunctive agents for management of uncontrolled symptoms by other measures Toxicities – gastritis, PUD Glucocorticoids May be used in low-to-moderate doses to achieve rapid disease control before onset of fully effective DMARD therapy 1-2 week bursts of steroids for management of acute disease flares Chronic administration of prednisone – to control disease activity in patients with inadequate response to DMARD therapy Low-dose prednisone Can retard progression of joint disease Must be balanced with side effects Intraarticular injection of intermediate steroid (triamcinolone acetonide) For rapid control of inflammation in a limited number of affected joints Must ensure that inflammation is not infectious Osteoporosis Important long-term complication of steroids Peptic ulcer No published guidelines for GI protection Conventional DMARDs Hydroxychloroquine, sulfasalazine, methotrexate, Leflunomide Has delayed onset of action – 6-12 weeks Methotrexate DMARD of choice for RA treatment MOA – stimulates adenosine release → anti-inflammation Leflunomide Inhibitor of pyrimidine synthesis Similar clinical efficacy as methotrexate Hydroxychloroquine Not a true DMARD; no retardation in RA progression Sulfasalazine Has shown to retard RA progression Radiographically Others Not used anymore Minocycline, gold salts, penicillinamine, azathioprine, cylclosporine Biological DMARDs Anti-TNF – first approved biological DMARDs for RA Anti-TNF Infliximab – chimeric (mouse-human) monoclonal antibody Adalimumab, golimumab – human monoclonal antibody Certolizumab pegol – pegylated Fc-fragment of human monoclonal antibody Etanercept – soluble fusion protein (TNF receptor 2 in convalent linkage with Fc portion of IgG1) Can be used in combination therapy or monotherapy (latter 4) Contraindication Active infection History of hypersensitivity with these agents Chronic hepatitis B infection Class III/IV CHF Screening for latent TB is important (PPD, IFN-gamma) Anakinra Recombinant form of naturally occurring IL-1 receptor antagonist Has limited use in RA Indications (for syndromes dependent on IL-1 production) Neonatal-onset inflammatory disease Muckle-Wells syndrome Familial cold urticaria Systemic juvenile-onset inflammatory arthritis Adult-onset Still’s disease Abatacept Soluble fusion protein consisting of extracellular domain of human CTLA4 linked to modified human IgG portion MOA – inhibits co-stimulation of T cells by blocking CD28- CD80/CD86 inreractions Can be used in combination therapy Rituximab Chimeric monoclonal antibody against CD20 Indications Refractory RA in combination with methotrexate More effect on seropositive patients Adverse effects Increased risk for infection PML Tocilizumab Humanized monclonal antinody against IL-6 Adverse effects Increased infection, increased LDL cholesterol
- 13. Small molecule inhibitors For RA resistant to conventional and biologic DMARDs Tofacitinib Small-molecule inhibitor of JAK1 and JAK3 Adverse effects Elevated liver enzymes, neutropenia, increased cholesterol, elevated serum creatinine Treatment of Extraarticular Manifestations RA-ILD Challenging, some DMARDs (methotrexate, Leflunomide) can cause pulmonary toxicity Treatment High-dose steroids + adjunctive immunosuppressants (azathioprine, Mycophenolate mofetil, rituximab) Management Considerations Pregnancy Up to 75% of female RA patients – overall improvement during pregnancy, but will flare after delivery Flares during pregnancy Low-dose prednisone Hydroxychloroquine Sulfasalazine Safest DMARDs to use during pregnancy Elderly Conventional and biological DMARDs – equally effective and safe in younger and older population Methotrexate May need renal adjustments Not prescribed when serum creatinine >2 mg/dL SLE (Chapter 349) 90% are women of child-bearing age HLA associations HLA-DRB1 HLA-DR3 HLA-DQA2 HLA-CR2 HLA-FCGR2A/B Genes for lupus nephritis HLA-DR3, STAT4, APOL1 (African Americans) FCGR2A, ITGAM, IRF5, IRF7, TNFSF4 (Ox40L), DNAse1 Pathology Skin biopsy Deposition of Ig at dermal-epidermal junction (DEJ) (also in normal skin) Injury to basal keratinocytes Inflammation by T cells in the DEJ and around blood vessels Renal biopsy Pattern and severity of injury are important for diagnosis and selecting best therapy Requires aggressive immunosupression (steroids + another drug) Class III Class IV Class V accompanied by III and IV Not required Class I and II, or with extensive irreversible changes Blood vessel pathology Leukocytoclastic vasculitis – most common pattern of vasculitis Lymph biopsy Usually performed to rule out infection or malignancies Nonspecific diffuse chronic inflmmation Diagnosis Based on characteristic clinical features and autoantibodies Classification of Nephritis (International Society of Nephrology and Renal Pathology Society Class I Minimal mesangial LN Class II Mesangial proliferative LN Class III Focal LN Class IV Diffuse LN Class V Membranous LN Class VI Advanced Sclerotic LN
- 14. Manifestations MSK Intermittent polyarthritis in hands, wrists, knees – most common Joint pain – most common reason to increase dose of steroids Ischemic necrosis of bone – diagnosed for persistence of pain in single joint (treated with systemic steroids) Myositis – usually drug-induced (steroids > antimalarials) “rhupus” – combined SLE and RA presentation Cutaneous Discoid lupus erythematosus (20%) – most common chronic dermatitis in lupus (+) roughly circular with slightly raised, scaly Hyperpigmented erythematous rims (+) depigmented atrophic centers (where all dermal appendages are destroyed) Treatment – topical or locally injected steroids + systemic antimalarials Photosensitive, slightly raised erythema, scaly on face – most common acute SLE rash; “butterfly rash” Subacute CLE – similar to psoriasis (+) Ro (SS-A) antibodies Renal Nephritis – most serious manifestation of SLE Class IV – most severe, and most severe type of LN DPGN – ESRD within 2 years (if untreated) Can lead to atherosclerosis CNS Cognitive dysfunction (memory difficulties, reasoning) - Most common manifestation of diffuse CNS lupus Seizures Treatment – both antiseizure and immunosupression Psychosis Can be the predominant form of SLE Must be distinguished from glucocorticoid-induced psychosis Myelopathy Tx: high-dose steroids Pulmonary Pleuritis with or without pleural effusion – most common pulmonary manifestation Tx: NSAIDS → steroids if more severe Life-threatening conditions Interstitial fibrosis Shrinking lung syndrome Intraalveolar hemorrhage Cardiac Pericarditis – most common cardiac manifestation More serious manifestations – myocarditis, Libman-Sacks (MR, AR) Vascular occlusions Cerebral event results from clotting Tx: long-term anticoagulation if treatment of choice Higher SLE MI events in women <49 years Risk factors for atherosclerosis Male, older, hypertension, dyslipidemia, diabetes, dysfunctional pro inflammatory HDL, repeated high scores for disease activity, high cumulative or daily doses of steroids, high levels of homocysteine and leptin Hematologic Normochromic, normocytic anemia – most common manifestation Leukopenia (lymphopenia) Thrombocytopenia GI Vomiting, diarrhea, diffuse abdominal pain (autoimmune peritonitis, and/or intestinal vasculitis), elevated liver enzymes Tx: aggressive immunosuppression with high-dose steroids for short- term control Ocular Sicca syndrome, nonspecific conjunctivitis – common in SLE, rarely threaten vision
- 15. Retinal vasculitis, optic neuritis – serious manifestations and blindness can develop over days to weeks Glaucoma, cataract – complications of steroids Laboratory Tests (1) To establish or rule out diagnosis (2) Follow the course of disease (3) Identify adverse effects of therapies Autoantibody Testing ANA – most important autoantibodies to detect (positive in >95% patients) Anti-Ro/SS-A Indicates increased risk for neonatal lupus, sicca syndrome, and SCLE Standard Tests for Diagnosis Screening using the following: o CBC, PC, urinalysis o May detect abnormalities contributing to diagnosis and influence management decisions Tests for Following Disease Course UA, hemoglobin levels, PC, serum creatinine, albumin For hematuria, proteinuria Identification of markers for disease activity See Table Management of SLE Aim is to achieve low-level disease activity o Mild symptoms on the lowest possible doses of medications o Usually achieved in 30-50% of SLE patients within a year Conservative Therapies for Management of Non-Life-Threatening Disease For patients with SLE autoantibodies, fatigue and pain without organ involvement Goal Management via suppression of symptoms Anagesics, antimalarialas are mainstay First issue with NSAIDs Increased risk for NSAID-induced aseptic meningitis, elevated serum transaminases, hypertension, renal dysfunction Second issue with NSAIDs All NSAIDs (particularly COX-2 inhibitors), increases MI risk Issue with hydroxychloroquine Must have annual eye examination for potential retinal toxicity At least 750 ng/mL – blood level needed for optimal response in active SLE NSAIDs Arthritis/arthralgias Antimalarials – hydroxychloroquine, chloroquine, quinacrine Dermatitis Arthritis Fatigue DHEA May reduce disease activity Belimumab For fatigue, rash, and/or arthritis Mostly effective with robust clinical activity: SLEDA ≥10 Positive anti-DNA Low serum complement Topical sunscreens Antimalarials Topical steroids and/or Tacrolimus Lupus dermatitis (systemic steroid with or without Mycophenolate mofetil, azathioprine, belimumab – sever or unresponse LD)
- 16. SLEDAI Widely used measure of SLE disease activitiy >3 Clinically active disease Life-threatening Management of SLE Systemic Steroids (0.5-1 mg/kg PO daily, 500-1000 mg IV daily) Methylprednisolone sodium succinate for 3 days → daily (0.5-1 mg/kg) prednisone Mainstay treatment for any inflammatory life- threatening or organ-threatening manifestations of SLE Management of LN (induction therapy) Steroids + Cylocphosphamide or mycophenolate mofetil (azathioprine is effective, but associated with more flares) African Americans, hispanics – mycophenolate Whites, Asians – cyclophosphamide or mycophenolate Mycophenolate toxicity diarrhea Cyclophosphamide toxicity Amenorrhea, leukopenia, nausea Responses to treatment Steroid – within 24 hours Cyclophosphamide, mycophenolate – 3-16 weeks Management of LN (maintenance therapy) Mycophenolate > azathioprine Cyclophosphamide – less safe Cyclophosphamide toxicity Ovarian failure Tx – GnRH agonist prior to each monhly cyclophosphamide Special Conditions Crescentic LN Treatment Either: High-dose cyclophosphamide High-dose mycophenolate Membranous LN (INS V) Treatment ACE-I or ABRs is recommended But usually none, unless with nephrotic proteinuria Pregnancy and Lupus Rates of fetal loss is higher in SLE o High disease activity, antiphospholipid antibodies (lupus anticoagulant), hypertension, and/or active nephritis Mainstay for active flares Hydroxychloroquine + lowest effective doses of prednisone/prednisolone + azathioprine (if failure to suppress activity) HCQ – reduces chance of subsequent fetus with heart block Dexamethasone – prevents progression of heart block SLE + antiphospholipid antibodies + prior fetal losses LMW heparin + low-dose aspirin Warfarin is teratogenic Adverse effects of prenatal steroids (primarily betamethasone) LBW CNS developmental abnormalities Predilection to adult metabolic syndrome Category A (no evidence of teratogenicity in humans) Steroids Category C (may be teratogenic in animals, no good evidence in humans) Cyclosporine, Tacrolimus, rituximab Category D (benefits > risks of teratogenicity) Azathioprine, hydroxychloroquine, mycophenolate, cyclophosphamide Category X Methotrexate Lupus and APAS Treatment Warfarin Target INR (2.0-2.5) for 1 episode of venous clotting Target INR (3.0-3.5) for recurrent clots or arterial clotting (CNS) Lupus (TTP, HUS) Treatment Diagnosis Identification of schistocytes, elevated LDH, anti-ADAMS13 Treatment Plasmapheresis – life-saving Concomitant steroid therapy – recommended by authorities
- 17. Lupus dermatitis Mainstay treatment Topical steroids + antimalarials (hydroxychloroquine) - Effective in reducing lesion severity and relatively safe Systemic retinoic acid - For recalcitrant cases Extensive, pruritic, bullous, ulcerating Systemic steroids with tapering → (hydroxychloroquine, retinoids, belimumab) Reports of success with Tacrolimus Dapsone or thalidomide Tacrolimus Increased risk for malignancies Thalidomide Extreme dangers for fetal deformities Peripheral neuropathy Associated Malignancies NHL Cancers of thyroid, lung, liver, vulvar/vaginal tissues Death Leading causes in 1 st decade of disease Systemic disease activity Renal failure infections After 1 st decade of disease Thromboembolic events Drug-induced Lupus Definition (+) positive ANA associated with Fever, malaise, arthritis/arthralgias, myalgias, serositis, and/or rash Features Predominant in whites Usually appear during therapy with certain medications, biologicals Less female predilection Rarely involved kidneys, brains Rarely associated with anti-dsDNA Commonly associated with anti-histones Usually resolves after discontinuation of medication Frequent suspects Antiarryhtmias Procainamide, disopryamide, propafenone Antihypertensive Hydralazine Several ACE-I and beta blockers Antithyroid PTU Antipsychotics Lithium, chlorpromazine Anticonvulsants Carbamazepine, phenytoin Antibiotic Isoniazid, minocycline, nitrofurantoin Antirheumatic Sulfasazaline Diuretic HCT Antihyperlipidemia Lovastastin, simvastatin Biologics IFN and TNF inhibitors PEARLS Approach to MSK diseases Focal, monoarthritis in acute onset Trauma/Fracture Gout Vascular ischemia Carpal tunnel syndrome Septic Arthritis Osteoarhthritis Most potent risk factor for OA Age Polymorphism in this gene is involved in formation of osteoarthritis GDF5 gene What joint is usually more involved in OA among Chinese Knees Important radiographic hallmark of OA Osteophytes MRI finding which correlates with severity of knee pain Presence of MRI synovitis Most common cause of chronic knee pain in patients >45 years Knee OA Amount of WBC in synovial fluid which accounts the presence of inflammatory or crystal-induced arthritis >1000 WBC/uL Never indicated as part of diagnostic workup Furthermore, it almost never warrant change in therapy MRI Mainstay treatment for osteoarthritis Non-pharmacological Initial choice of treatment for OA Acetaminophen (high-dose) The use of these agents were banned in the treatment of OA Chondroitin Glucosamine Gout and Other Crystal-Associated Arthritis Excretion of this amount of uric acid per day on a regular diet suggests overproduction of purine >800 mg/day Ultrasound manifestation of gout (+) double contour sign Severe hyperuricemia requiring Hypouricemic therapy >9 mg/dL (>535 umol/L) Underexcretor of uric acid <600 mg/day Other medications with mild uricosuric effects Losartan Amlodipine Fenofibrate Contraindications of colchicine use Dialysis patients (+) P glycoprotein (+) CYP3A4 inhibitors - clarithromycin Rheumatoid Arthritis Temperature before one must suspect for Vasculitis or infection in RA patients >38.3 C Main histological and radiologic patterns of ILD Usual interstitial pneumonia Non-specific interstitial pnuemonia Most common cause of death in RA CVD Associated conditions with RA CVD
- 18. Osteoporosis hypoandrogenisms Has greater specificity for RA diagnosis than RF ACPA Initial radiographic finding in patients with RA Periarticular osteopenia Delayed onset of actions of conventional DMARDs 6-12 weeks SLE Most important autoantibody to test for SLE ANA Achievement of low-level disease SLE activity 30-50% patients within a year