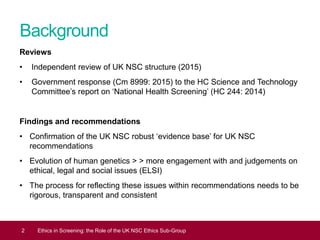
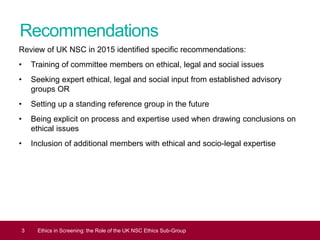
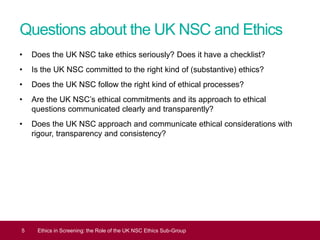
The UK NSC Ethics Sub-Group was formed to improve the consideration of ethical issues in screening recommendations. It aims to develop a checklist of ethical considerations and a rigorous methodology for integrating ethics. While the UK NSC takes ethics seriously, reviews found it needs more explicit and transparent processes when ethical acceptability determines recommendations. The Sub-Group seeks to ensure ethics are addressed with consistency, transparency and involving relevant expertise.