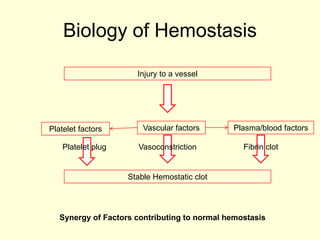
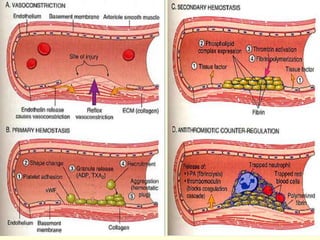
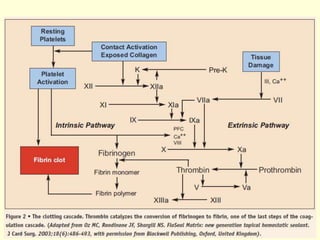
(1) Hemostasis involves three synergistic factors - platelet plug formation, vasoconstriction, and fibrin clot formation. Secondary hemostasis specifically refers to the activation of the coagulation cascade and formation of a permanent fibrin plug.
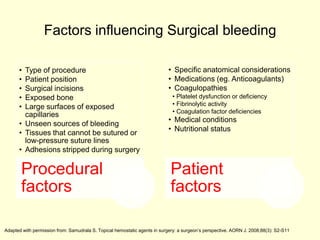
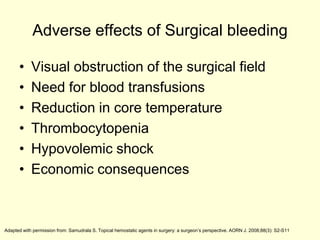
(2) Surgical bleeding can be arterial, venous, or oozing and is influenced by patient factors like medications and coagulopathies as well as procedural factors. Excess bleeding can adversely impact the surgical field and patient.
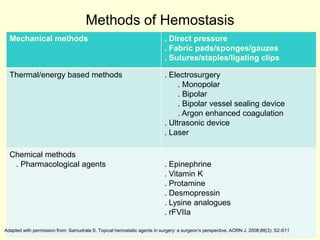
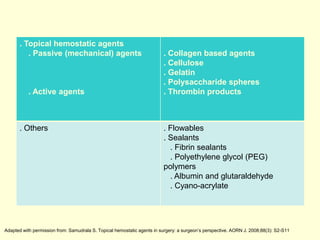
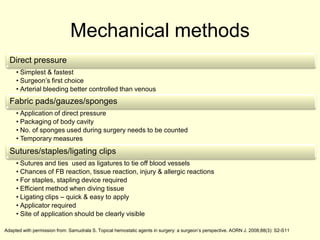
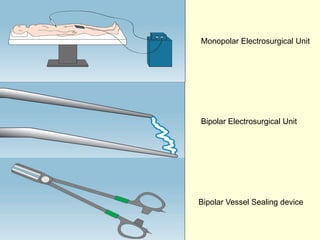
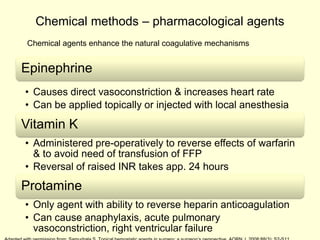
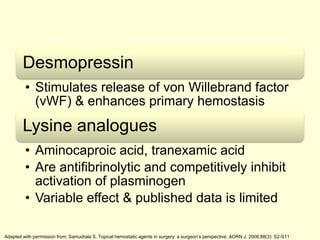
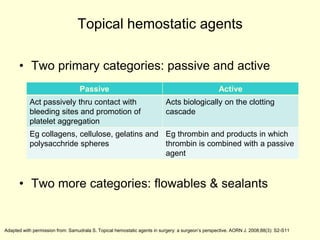
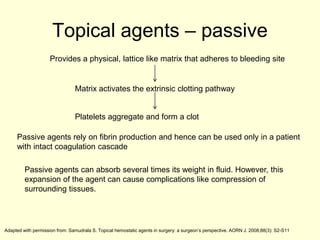
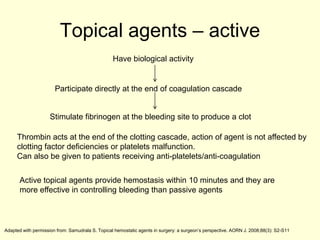
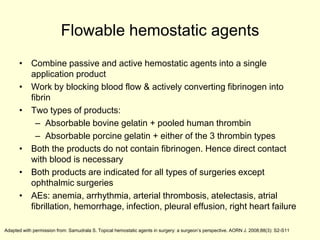
(3) Methods to achieve hemostasis include mechanical methods like direct pressure, sutures and staples, and chemical methods like pharmacological agents and topical hemostatic agents. Topical agents can be passive, promoting cl