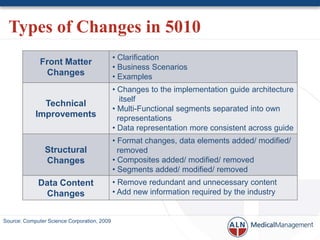
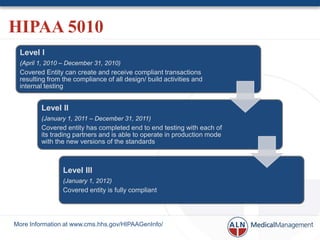
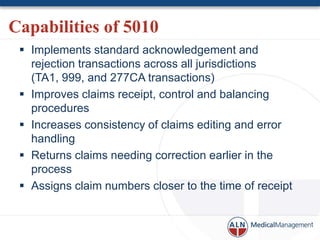
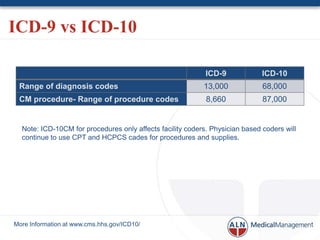
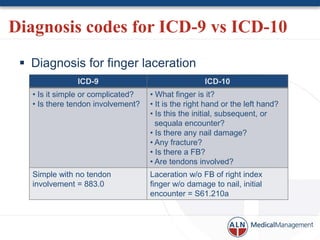
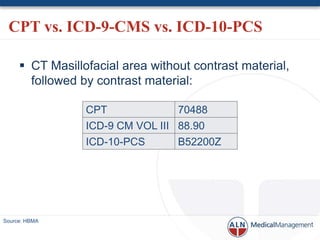
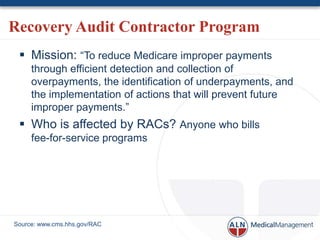
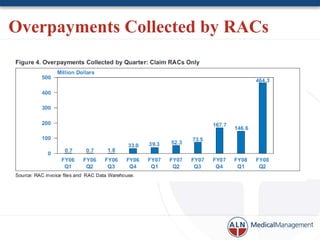
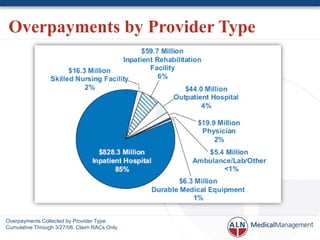
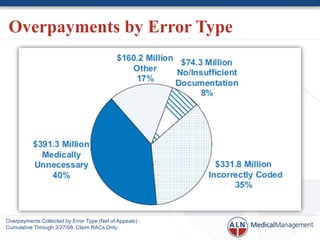
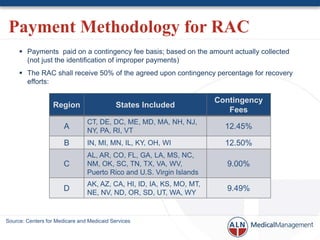
The document discusses recent changes in revenue cycle management (RCM) and the coding and compliance landscape, highlighting updates related to HIPAA 5010 and the transition from ICD-9 to ICD-10. It outlines improvements in transaction processes, the increased complexity of coding with ICD-10, and the role of recovery audit contractors in addressing payment inaccuracies. The document emphasizes the need for enhanced RCM performance and interoperability in managing both clinical and financial data.