Heart classification (internal medicine)
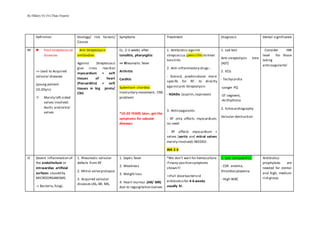
- 1. By Hillary Vo (Vo Thao Duyen) Definition Etiology/ risk factors/ Causes Symptoms Treatment Diagnosis Dental significance RF Post-streptococcal diseases => Lead to Acquired valvular diseases (young patient: 10-20yrs) Mainly left-sided valves involved: Aortic and mitral valves Anti-Streptolysin antibodies: Against Streptococci give cross reaction myocardium + soft tissues of heart (Pancarditis) + soft tissues in big joints/ CNS Cc. 2-3 weeks after tonsilitis, pharyngitis: => Rheumatic fever Arthritis Carditis Sydenham chordea: Involuntary movement, CNS problem! *10-20 YEARS later, get the symptoms for valvular diseases 1. Antibiotics against strepcoccus (penicillin) to treat tonsilitis 2. Anti-inflammatory drugs : - Steroid, prednisolone: more specific for RF, to directly againstanti-Streptolysin - NSAIDs (aspirin,naproxen) 3. Anticoagulants: - RF only affects myocardium; no need - RF affects myocardium + valves (aortic and mitral valves mainly involved):NEEDED: INR 2-3 1. Lab test Anti-streptolysin titre (AST) 2. ECG - Tachycardia -Longer PQ -ST segment, -Arrthythmia 3. Echocardiography Valvular destruction Consider INR level for those taking anticoagulants! IE Severe inflammation of the endothelium or intracardiac artificial surfaces caused by MICROORGANISMS -> Bacteria,fungi, 1. Rheumatic valvular defects from RF 2. Mitral valveprolapse 3. Acquired valvular diseases (AS, AR, MS, 1. Septic fever 2. Weakness 3. Weight loss 4. Heart murmur (AR/ MR) due to regurgitation (valves *We don’t wait for hemoculture if many positivesymptoms shown!!! =>Full dosebactericid antibioticsfor 4-6 weeks usually IV. 1. Lab: (unspecific) - ESR: anemia, thrombocytopenia - High WBC Antibiotics prophylaxis are needed for dental and high, medium risk group
- 2. By Hillary Vo (Vo Thao Duyen) mycoplasma… Vegetation on the valves,parietal endocardium,chordae or catheters, pacemaker electrodes… “Think of heart first, then other organs (microbes from heart embolizes to other places” MR) 4. Hypertrophic cardiomyopathy 5. Previous IE 6. Congenital valvular diseases (cyanotic) 7. Prosthetic heart valve (high risk) 8. Central venous catheters 9. IV drug users 10. 50% has no risk factors 11. Pacemaker 12. ASD, VSD (low risk) Others are medium risk! *Mortality 100% die with no treatment 20-30% die with antibiotics can’t close) 5. Cardiac failure(rarely pericarditis) 6. Abdomen: splenomegaly due to bacteria activity increasemakes spleen enlarge (SEPSIS) 7. Microembolized from vegetation to: - kidney (focal GN): hematuria - Skin: petecchiae - Brain: stroke, MI, pulmonary embolism (paradoxical embolismto the brain due to ASD, VSD) 1. Antibiotics A. Before hemoculture: combined broaded spectrum: - Cephalosporins - Aminoglycosides - Vancomycin (for staphy => Because staphy is resistant to penicillin!) B. After hemoculture: targetted antibioticstherapy 2. Surgery (Done in caseof antibioticsdoes not work): prosthetic valvereplacement (20% die) 3. If prosthetic valve undergo IE early:100% reoperation 4. If prosthetic valve undergo IE lately:30% reoperation - high CRP - Hematuria - Bacteremia (due to sepsis) 2. Hemoculture (specifc diagnosis) 3x2 during 2x24 hours: => Culture minimum 3 times per day - Never use 1 set of culture, 2 sets of cultureneeded - Culture in 2 days -Culture 24 hrs before antibioticstreatment (broad spectrum) *Microbiology: 1/ Strepto: 50% 2/ Staphy: 20-25% 3/ Gram (-): 5-10% Taken: 1. Prior to intervention (1h) 2. Orally 3. Singlebig dose
- 3. By Hillary Vo (Vo Thao Duyen) 4/ Fungi: 1% 5/ Culture (-): 10% 3. Echocardiography (specific) -Transesophageal echo: more detailed than transthoracal. - Vegetations are visible after 2 weeks. AS During systolic period, obstruction to the outflow of blood Pressure gradient appears between LV and aorta. => LVH because the heart try to pump more! => LV dilated => LVF (irreversible) 1. RF 2. IE 3. Degenerative valve destruction (atherosclerosis) 1. No complaints for a long period 2. Dyspnoe 3. Angina 4. Syncope 5. Lately LVF 6. Physical symptoms: auscultation:ejection click, mid-systolic murmur above the aorta. = Crescendo-Decresendo murmur => Radiate to neck/carotid In caseof SEVERE AS: Do artificial/ prosthetic valve implantation 1. Mechanical (Lifelong anticoagulantswith coumarin) Target INR: 3-4.5 2. Biological: Target INR: 2-3 or no anticoagulantsneeded NB: 1. ECG: LVH 2. Chest X-ray: cardiomegaly 3. Look at the sizeof stenosis and pressure gradient: normally low, if gradient appear => AS Normal value: 5cm2, <5mmHg Mild:>1.5cm2, <25 Moderate: 0.7-1.5, 25-50mmHg Severe: <0.7, >50 Antibiotic prophylaxis for IE prevention. Anticoagulant therapy (heparin and warfarin) due to prosthetic valve replacement
- 4. By Hillary Vo (Vo Thao Duyen) arteries 7. BP: 100/80mmHg 8. Pulsus tardus et parvus (slowand small) Coumarin: Stops the growth of thrombin Heparin: Reduces the size of thrombin 4. Angiography + ventriculography before surgery AR Duringdiastolicperiod, blood regurgitates from the aorta into the LV => LVH in chronic AR for long accommodation period. => Angina pectoris AS = AR 1. Auscultation: Decrescendo diastolic murmur above the aorta but on the left sideof intercostal space(ICS) 2. BP: 180/ 40mmHg 3. Pulsus celer et altus (fast and high) 4. Complaints: Weakness, dyspnoe 1. Mechanical prosthetic heart valvereplacement 2. Pharmaco: - ACE inhibitors:Captopril - Nitrates: => Lower BP => VD: reduce preload before surgery 1. ECG: LVH 2. Echocardiography: Doppler echo for regurgitation 3. CT Coronarography: needed only in caseof IHD M S Duringdiastolicperiod, obstruction to the BF between LA and LV BF back to lung/ pulmo embolism-> pulmo pressureincrease: pulmonary hypertension -> RVH => RF exclusively => cause commissural fusion on mitral valves => MS Physical signs: 1st sound is accentuated on the apex. - Mid-diastolic murmur on the apex - Opening snap (hardly open) Atrial fibrillation: 1. Moderate or severe form: Catheter balloon dilation or surgery (commissurotomy or artificial replacement) 2. In case of atrial fibrillation: lifelongoral anticoagulation 1. ECG: LAH, RVH 2. Echocardiography 3. Size and pressure gradient: Normal value: 4-6cm2, <2 mmHg
- 5. By Hillary Vo (Vo Thao Duyen) peripheral edema LA can’t hypertrophy => become abnormal => atrial fibrillation Tachy/ Brady/ Normocardia 3. In caseof Tachycardia: beta blocker 4. Diuretics Mild:>1.5, <5 Moderate: 1-1.5, 5-10 Severe: <1, >10 M R During systolic period, Open of AV valve. Volume loading to LV then LA. Heart try to pump more => LVH => LV dilation => no blood supply to endocardium => Angina pectoris => LVF => Pulmonary hypertension => Pulmo congestion => pulmonary edema 1. RF 2. IE 3. Degenerative disorders 4. Mitral valveprolapse 5. Cardiomegaly (Valves are okay but increase the space) 6. MI, or IHD =>Rupture of papillary muscle Physical signs: Holosystolic murmur on the apex. Radiates to axilla! In case of LVF => artificial valve replacement 1. ECG: LAH, LVH 2. Echo: Doppler echo 3. Coronarography: necessary in case of surgery Antibiotic prophylaxis before dental intervention
- 6. By Hillary Vo (Vo Thao Duyen) Angina pectoris Stable Unstable = NSTEMI Prinzmetal/ Variant angina= STEMI Silent ischemia Myocardial infarction Definition: Chest pain because of episodic myocardial ischemia = Effort angina = warm up angina 1. Pain after minor exertion (short walk or shaving) 2. Relieved at rest 3. Dangerous in the morning 4. GERD-induced angina 5. Retrosternal pain 6. Lasts typically 2-5 min 7. If lasts longer than 20 mins => CHECK FOR ACS: Acute coronary syndrome = Crescendo pattern 1. Pain atrest/ or minor exertion 2. Then increase frequency of pain => plaquedisruption => acute obstruction in coronary artery 3. Partof ACS = Vasospasmic angina 1. Coronary artery spasm due to smooth muscles constrict => transmural ischemia 2. Maybe due to VC (TXA2…) 3. Happen anytime Obstructive CAD, but assymptomatic Acute MI: Result from acute obstruction to a coronary artery from sudden disruption of atherosclerotic plaque. Risk factors: 1. Hypercholestemia 2. DM 3. Smoking 4. Hypertension Range severity: 1. Unstableangina 2. NSTEMI 3. STEMI 4. SCD: sudden cardiac death
- 7. By Hillary Vo (Vo Thao Duyen) Morphology 1. Thick fibrous cap 2. Blocked by atherosclerotic plaque 3. 70% stenosis 4. No thrombus formation 1. Thin fibrous cap 2. Blocked by atherosclerotic plaque+ thrombus => If plaquenot rupture, keep unstableangina => if plaque ruptures, become MI! 3. 75-80% blocked? 1. May or may not have atherosclerosis 2. Transmural ischemia Atherosclerotic present in elder or in DM patient Complete obstruction of LAD, circumflex artery ST segment Depression Depression (more) Or sloping=> Non-persistent! Elevation Changes duringactivity Elevation Symptoms 1. Dyspnoe 2. Fatique, faint 3. Nausea, vomit 4. Sweating 5. Sense of impending doom: cảm giác có điều gì chẳng lành sắp xảy ra 6. Pain radiates to Similar to angina
- 8. By Hillary Vo (Vo Thao Duyen) shoulder, left arm, neck, jaw, back Physical signs: 1. 3rd and 4th heart sounds 2. Systolic murmur due to MR (rupture of papillary muscles) 3. Pulmonary congestion Treatment 1. Beta blockers: decrease BP and contractility 2. Nitroglycerin (contains nitrates/ isosorbide dinitrate):Venous and coronary vasodiation 3. CCB: Nifedipine, amlodipine 4. Antiplatelet drugs: clopidogrel: inhibitADP receptors on platelet 1. Bed rest with ECG monitoring 2. Same as stableangina (Must have CCB) 3. PCI or CABG = PERCUTANEOUS CORONARY INTERVENTION or Coronary artery bypass surgery/ graft 1. Nitroglycerine 2. CCB 1. Same as stable angina 2. Lipid loweringstatins 1. Oxygen therapy 2. ECG monitoring 3. General treatment: - Relieve stress - Reverse ischemia if possible(after 20-40 mins -> irreversible) 4. Aspirin (home treatment/ emergency): to slow down the blood clot to prevent secondary MI
- 9. By Hillary Vo (Vo Thao Duyen) => Best treatment for angina: Beta blockers + nitroglycerins Q. How to differentiate between angina and MI? Give nitroglycerine sublingually in thefirst2 mins => If pain won’t be relieved => MI 4. After stent, take aspirin + clopidogrel for at least1 year 5. Specific treatment *If we can’t do PCI: immediate fibrinolysis (streptokinase) (preferably <30 min after MI) *PCI := angiography with stent through femoral or transradical access (goal therapy): preferbly < 60 mins 6. If there are more than 1 blocked artery => do CABG! Through internal thoracic artery to coronary artery!
- 10. By Hillary Vo (Vo Thao Duyen) 7. Morphine 8. Others are sameas stable + ACE inhibitors: antithrombotic (rtPA...) 9. Thrombolytic drugs: Fibrin specific: tPA Fibrin non-specific: streptokinase *Indication:ST elevation, LBBB *Absolute contraindication:
- 11. By Hillary Vo (Vo Thao Duyen) Aortic dissection, intracranial tumor, pericarditis,previous stroke Diagnosis 1. ECG (ST) 2. Stress ECG to distinguish between stableand unstable -Negative stress test: target HR reached without ECG alteration. 3. Angiography is done after positivestress test is confirmed 4. Nuclear cardiology *Differential diagnosis 1. GI: GERD 2. Other cardiac disorders: Pericarditis,mitral valve prolapse,ventricular tachycardia 1. ECG 2. Stress ECG: -Positivestress test: ST depressed 3. Cardiac markers Troponin, CK-MB: negative (wolf in the sheep’s cloth) 4. Angiography ECG 1. ECG -ST elevation to * 1mm in two or more limb leads * >2mm in two or more precordial leads - LBBB - Muscle nerosis: Q wave enlargement 2. Cardiac markers -CK-MB peak 24h, decline 2-3 days - Troponin T,I, LDH: peak 24-48hrs, decline in 7-10 days - myoglobulin: not specific for MI
- 12. By Hillary Vo (Vo Thao Duyen) No echocardiogram for ischemia and MI! 3. Coronary catherization and angiography (invasive cardiac imaging) Complication of MI: Cardiac failure: Failureof systolic or diastolicfunctions can be in rightor left or both, happens duringmajor, minor exerciseor even in rest
- 13. By Hillary Vo (Vo Thao Duyen) Symptoms depends on onset (acute, chronic),causes,localization (left,right) Etiology Symptoms Treatment Diagnosis LVF (Acute LVF = cardiac asthma) *Blood/fluid go back to lung 1. IHD 2. Valvular disorders 3. Primary cardiomyopathies:dilative, hypertrophic or restrictive 4. Secondary cardiomyopathies: Hypertension, alcoholic,myocarditis 5. Congenital cardiac disease 6. Cor pulmonale Main causes of Acute LVF: 1. MI 1. Hypertensive crisis (exceed 150mmHg) or 180/110mmHg 2 forms: LVF and acute LVF *LVF: 1. Congestion in the lung(still okay) 2. Shortness of breath 3. Dyspnoe after exercise, even in rest 4. Orthopnoe (feel worse while in supine position, but feel better when stand up) 5. Paroxysmal nocturnal dyspnoe *Acute LVF = Cardiac asthma Cardiac asthma: is not a type of asthma, it’s a type of coughing and wheezing that occurs with left heart failure 1. Pulmonary edema (acute form) due to severe and acute pulmonary congestion (Pulmonary hypertension) 1. Non-drug therapy Salt and water restriction: to decreaseBP 2. Drug therapy -Diuretics: decrease fluild buid up *Furosemide: specific for heart failure treatment (For hypertension,use thiazidemore) *Spironolacton:(aldosteroneantagonist) *triamteren -Beta blocker: Slower HR and lower BP -ACE inhibitors:(Captopril) improve coronary circulation by decreasingBP and plasma volume -Nitrates: VD - Digitalis: stronger, longer muscle contraction 1. Physical examination (according to the symptoms) 2. Chest x-ray 3. Echocardio graphy 4. ECG 5. Lab data Differential diagnosis: 1. Pulmo diseases 2. Obesity 3. Renal or liver failure 4. Circulatory
- 14. By Hillary Vo (Vo Thao Duyen) => excess fluid in bronchial tree => Pink foam from the mouth, Crackles over the lung => V/Q mismatch => Hypoxia, cyanosis “Pinky nằm ngủ” 3. Invasive,surgical interventions - Artificial heartvalve - Pacemaker - Coronary bypass (CABG) - Cardiac transplant failure of both legs (If just 1 leg => not cardiac failure!!! RVF *Blood/ fluid go back to body 1. Primarily: from - chronic lungdisorders (Cor pulmonale) - MS - ASD, VSD, pulmonary stenosis 2. Secondary: followed by LVF 1. Peripheral edema: edema of lower limbs or in sacral region 2. Abdomen: Splenomegaly, hepatomegaly 3. Ascites (fluid in peritoneal space) 4. Pleural effusion??? 5. Kidney: Nocturnal urination 6. Dilated jugular vein *Usually appear all together* Same
- 15. By Hillary Vo (Vo Thao Duyen) 3. If the cause come from pulmonary embolism(PE)--> From (PE) => ACUTE RIGHT VENTRICULAR FAILURE - Hypotension (Due to decreased SV => decreased CO => decreased BP) - Hypoxia - Cyanosis - Tachycardia - Severe chest pain - In acute cor pulmonale:COPD --> RVF --> eventually lead to LVF From PE: