Histology of oral mucous membrane and gingiva
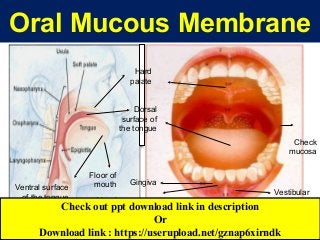
- 1. Oral Mucous Membrane Gingiva Alveolar mucosa Vestibular fornix Labial mucosa Check mucosa Hard palate Dorsal surface of the tongue Ventral surface of the tongue Floor of mouth Check out ppt download link in description Or Download link : https://userupload.net/gznap6xirndk
- 2. Functions of the oral mucosa Protection Sensation Secretion Thermal regulation?
- 4. Histological structure Oral Mucosa Consists of 2 major components:- Oral Epithelium Lamina Propria
- 5. CLICK HERE TO DOWNLOAD THIS PPT https://userupload.net/gznap6xirndk
- 6. Histological Structure Lamina propria Divided into 2 layers:- Superficial zone of loose C.T adjacent to epithelium & surrounding epithelial ridges- papillary layer & A deeper zone of denser C.T called reticular layer because of the net like appearance of its fiber bundles Differences between the 2 layers are not clear cut & it is the relative concentration & arrangement of fibers
- 7. Histological Structure Lamina propria Lamina Propria may be:- Directly attached to periosteum of alveolar bone or Overlay the Submucosa Submucosa is formed of C.T; the nature of this C.T. determines whether mucous membrane is loosely or firmly attached to underlying structure. Submucosa contains glands, B.Vs, nerves & adipose tissue.
- 9. Oral Mucous Membrane Classification 1-Keratenized mucosa ( Masticatory mucosa( (A( Gingiva (B( Hard palate 2-Non-keratenized mucosa (Lining mucosa( )A) Firmly attached )B) Loosely attached I- Soft palate II-lip III-cheek IV-ventral S tongue I- Floor of mouth II-Vestibule III-alveolar mucosa3-Specialized mucosa Dorsal surface of tongue
- 10. Oral Mucous Membrane Classification I- Masticatory mucosa (Keratinized mucosa) a. Gingiva b. Mucous membrane covering hard palate II-Lining mucosa (Non-keratinized mucosa) Present in areas not subjected to high levels of friction but is mobile & distensible 1. Firmly attached to underlying muscles a. Lip b. Cheek. c. Inferior surface of the tongue. d. Soft palate 2. Loosely attached to underlying structures as bone, fascia or muscle a. Alveolar mucosa. b. Vestibular fornix. c. Floor of the mouth. • III- Specialized mucosa Covering dorsal surface of tongue
- 11. Keratinized & non-Keratinized mucosa Stratum basal Stratum spinosum Stratum intermedium Stratum granulosum Stratum superficial Keratohyaline Gs. Keratenized epithelium Non-keratenized epithelium Stratum cornium
- 15. CLICK HERE TO DOWNLOAD THIS PPT https://userupload.net/gznap6xirndk
- 19. 1.Thickening of adjacent cell membrane 2. A pair of attachment plaque 3.Tonofilaments 4. Extracellular structure Desmosomes
- 20. Hemi-Desmosomes & Basal Lamina
- 22. The Keratinized oral epithelium comprises the following undernoted layers except one. Which one is the exception? A.The basal cell layer B.The spinous cell layer (prickle cell layer) C.The granular cell layer D.The intermediate layer E.The cornified layer
- 23. Keratinized Epithelium Cells are arranged in 4 layers:- Basal (stratum basal), Spinous (stratum spinosum), Granular (stratum granulosum) & Cornified (stratum cornium). Basal cell layer Cells are cuboidal or columnar & are arranged in a row on a B.M. Cells are attached to each other by a cellular junction & also to B.M Spinous cell layer Several rows of polyhedral cells of different shape & size & larger than basal cells. Basal cells & spinous cells constitute more than 1/2 thickness of epithelium. Cells of spinous layer are joined together by intercellular bridges giving the cells a prickly appearance Granular cell layer Lies above prickle cell layer & is made up of several rows of flattened epithelial cells. The cells contain large no. of small granules called keratohyaline granules. Cornified layer In K.E is the final stage in maturation. Cells are termed epithelial squames; these are cells that shed, necessitating the constant turnover of epithelial cells
- 25. CLICK HERE TO DOWNLOAD THIS PPT https://userupload.net/gznap6xirndk
- 26. • The prickle cell layer (spinous) in keratinized oral epithelium is located between the:- A.Basal layer & granular layer B.Granular layer & keratinized layer C.Superficial layer & intermediate layer D.Keratinized layer & intermediate layer E.Keratinized layer & superficial layer
- 28. Keratinocytes Constitute the major part of epithelial cells The cells are arranged in different layers During maturation they either change to keratin or share in keratin formation These cells have the following criteria:- Always present in sheets & attached to each other by one or more type of cellular junctions Cytoplasm of these cells is stained with H & E Cytoplasm contains the tonofilaments
- 29. Non-keratinocytes Present in both keratinized & non-keratinized epithelium & have the following criteria:- 1- Appear as clear cells by ordinary H&E stain, they need special stains 2- Present as scattered cells & not in sheets 3- A clear hallows around their nuclei 4- Their cytoplasm is free from tonofilaments 5- No cellular junctions 6- Do not play any role in synthesis of keratohyaline granules or keratin
- 30. 1-Pigment cell (Melanocyte, blast) 2- Langerhan’s cell 3- Merkel’s cell Shape Small body with long slender & branched process Contain melanin granules (melanosomes( Similar in shape Contain granules (Langerhan’s granules( Do not have long processes Contain small membrane bounded granules Location Basal & parabasal layers High level cell and may be found at lower levels. Basally in epithelium H&E Stain Not stained so- called (Clear dentritic cell( Not stained so-called (Clear dentritic cell( Not stained so- called (Clear but not dentritic cell( Special stain DOPA reaction (for tyrosinase enzyme( Gold chloride
- 31. Origin Neural crest cells Bone marrow Neural crest cells Cell junction No tonofilaments No desmosomes No tonofilaments No desmosomes Little tonofilaments Little desmosomes Nerve cell seen to be associated with the cell with synapse-like cleft Function Pigmentation If melanosomes engulfed by epithelial cell called (Melanophore( or by C.T. cell (Melanophage( Neural element. Degenerated melanocyte Intra epithelial Macrophage Regulatory cells (control epith. Cell division & differentiation( Uptake & processing of antigen in contact allergic reaction Responding to touch 4-Inflammatory cells They are transiant cells
- 33. Melanin pigmentation of basal keratinocytes
- 34. Pigmented Basal Keratinocytes & dentritic processes of Melanocytes
- 36. Keratinized Mucosa Masticatory Mucosa During mastication, parts of oral mucosa are subjected to forces & pressure Gingiva Hard Palate
- 37. Macro-Anatomy of Gingiva Free gingiva Free gingival groove Interdental papilla Attached gingiva Mucogingival junction Alveolar mucosa
- 39. Interdental Papilla & Gingival Col Gingival col( non- keratenized(
- 40. Histology of Gingiva Stratified squamous keratenized epithelium Lamina propria Epithelial rete peg C.T papilla Tall Numerous Slender Irregular No submucosa
- 41. Gingival fibers Dento-gingival group Alveolo-gingival group Circular group Dento-periosteal group
- 42. Macro-Anatomy of palate Incisive papilla Palatine gingiva Antero-lateral area (fatty zone( Postero- lateral area (glandular zone( Rugae area Median palatine raphe Soft palate Uvula
- 44. Histology of Hard Palate Submucosa Fatty zone Glandular zone Epithelial rete pegs are tall & numerous Mucosa
- 45. Non-Keratinized Mucosa Lining Mucosa Present in areas not subjected to high levels of friction but is mobile & distensible Firmly attached to underlying muscles Soft Palate Lip Cheek Ventral Surface of tongue Loosely attached to underlying structures as bone, fascia or muscle Floor of mouth Vestibule Alveolar Mucosa
- 46. Soft palate Oral sideNasal side Respiratory epithelium
- 47. Lip
- 48. Lip Vermilion border Mucous side Skin side
- 50. Skin
- 51. Skin appendages Hair follicle Sebaceous gland Sweat glands
- 55. Specialized Mucosa Dorsal Surface of Tongue
- 59. Tongue Papillae 1. Filliform Papillae 2.Fungiform Papillae 4. Folliate Papillae 3.Circumvallate Papillae Taste bud
- 62. Taste bud 3.Neuroepithelial cell 1.Outer supporting cell 2.Inner supporting cell Taste pore
- 64. Lingual Tonsil Weber salivary gland (Pure mucous)
- 65. Lingual tonsil
- 67. Histogenesis of Dento-Gingival Junction 1 2 3 4 Desmolytic enzymes Epithelial plug 1ry D.G.J (from Reduced E. E.) 2nd D.G.J. (from oral E.)
- 68. Histology of Dento-Gingival Junction Basal cell layer External basal lamina Lamina propria Superficial flat cells Hemidesmosomes Internal basal lamina
- 70. Stages of Passive Eruption Anatomical Crown Clinical Crown Coronal end (E) Apical end CEJ 1 year before shedding in 1ry teeth & in permanent- Till 20-30 yrs First stage
- 71. Second stage Anatomical Crown Clinical Crown Coronal end (E) Apical end (C). Persist till 40 years
- 72. Third stage Anatomical CrownClinical Crown Coronal end (C.E.J.) Apical end (C) Transitory stage
- 73. Fourth stage Anatomical CrownClinical Crown Coronal end (C) Apical end (C) Persists till tooth loss
- 75. CLICK HERE TO DOWNLOAD THIS PPT https://userupload.net/gznap6xirndk
Editor's Notes
- The oral mucous membrane is structurally & functionally a transitional zone between the skin & mucosa of the G.I.T & exhibits features of both. It resembles intestinal mucosa in that it is bathed in fluid & its epithelial cells have a high rate of turnover. It is similar to skin in that it possesses a stratified epithelium which is keratinized in many places & prevents diffusion across it in both directions. Organization of the oral mucosa The oral cavity consists of 2 parts; an outer vestibule bounded by lips & cheeks & the oral cavity proper separated from the vestibule by the alveolus bearing the teeth & gingiva. The superior zone of oral cavity proper is formed by hard & soft palate. The floor of mouth & base of tongue form the inferior border. Posteriorly, the oral cavity is bounded by pillar of fauces & tonsils.
- Functions of the oral mucosa 1-Protection The oral mucosa separates & protects deeper tissues & organs in oral region from the environment of oral cavity. The oral mucosa shows a number of adaptations of epithelium & C.T to withstand the mechanical forces (compression, stretching, shearing & surface abrasion) applied on it during mastication. It also provides a barrier to microorganisms, toxins & various antigens. 2-Sensation The sensory function of oral mucosa is important because it provides information about events within the oral cavity, whereas, the lips & tongue perceive stimuli outside the mouth. In the mouth, receptors respond to temperature, touch & pain; the tongue also has taste buds. Certain receptors in the oral mucosa respond to the taste of water & signal the satisfaction of thirst. Reflexes such as swallowing, gagging, retching & salivation also are initiated by receptors in oral mucosa. 3- Secretion The major secretion associated with the oral mucosa is saliva, produced by major & minor salivary glands. The saliva maintains a moist & lubricant surface of oral mucosa. Also it provides a buffering action as well as secreting some antibodies. Sebaceous glands frequently are present in oral mucosa but, their secretions are insignificant. 4- Thermal regulation In some animals, such as dog, considerable body heat is dissipated through the oral mucosa by panting; for these animals the mucosa plays a major role in the regulation of body temperature. However, the human oral mucosa plays practically no role in regulating body temperature.
- Histological structure Histologically, the human oral mucosa consists of 2 major components:- The oral epithelium Lamina propria, a C.T. supporting layer. Both of these 2 layers are separated by a well-defined B.M. & attached either directly to underlying structures or through a submucous layer. 1- The oral epithelium Is ectodermal in origin & formed of St. Sq. Epith. The epithelium is keratinized in certain areas & non-keratinized in others:- Keratinized oral epithelium. Non-keratinized oral epithelium. II- Lamina propria The lamina propria is divided into 2 layers, superficial zone of loose C.T. adjacent to epithelium & surrounding epithelial ridges, the papillary layer & a deeper zone of denser C.T. called reticular layer because of the net like appearance of its fiber bundles. The differences between these 2 layers are not clear cut & it is the relative concentration & arrangement of fibers rather than any absolute difference that enables these regions to be distinguished. The papillary layer contains fine collagen fibers arranged as a loose open network. In region of B.M, these fibers are associated with reticular fibers; while at the junction with subjacent reticular layer they merge into thicker collagen bundles. In reticular layer the collagen fibers are coarser & closely packed; they are arranged in laminae. The reticular zone is always present, while the papillary zone may be absent in some areas where the papillae are either very short or lacking alveolar mucosa. Cellular elements found in Lamina Propria of oral mucosa are Synthetic cells: fibroblasts secreting fibers & ground substance & fat cells concerned with the synthesis & storage of fat. Defensive cells: are macrophages, mast cells & variable numbers of inflammatory cells derived from circulating leucocytes. Undifferentiated Mesenchymal cells The constituent cells of vascular & lymphatic channels & of neural elements. The lamina propria may be directly attached to the periosteum of alveolar bone or it may overlay the submucosa. The submucosa is formed of C.T; the nature of this C.T. determines whether mucous membrane is loosely or firmly attached to underlying structure. It contains glands, B.Vs, nerves & adipose tissue. The larger arteries are divided into smaller branches, which enter the lamina propria where they divide again to form a subepithelial capillary network in the papillary layer beneath epithelium. The veins originating from the capillary network course back along the path taken by arteries, a rich network of lymph vessels accompanies B.Vs. The sensory nerves tend to be more concentrated toward anterior part of mouth. The nerve fibers are myelinated as they traverse the submucosa but lose their myelin sheath before splitting into their end. Sensory nerve endings of various types are found in papillae some of the fibers enter the epithelium, where they terminate between the epithelial cells as free nerve endings. Junction of Epithelium & Connective Tissue A complex arrangement links epithelial & C.T. components of oral mucosa. In the light microscope, a layer 1-2 µm thick is seen on the lamina propria side of the junction. This is termed the B.M. In the E. microscope, the layer appears much thinner & is then termed the basal lamina. This thicker appearance in the light microscope is due to the inclusion of some sub-epithelial collagen fibers which in this region have staining properties similar to those of the basal lamina.
- Classification of the oral mucosa Considerable structural variations are shown by oral mucosa in different regions. The 3 main types of mucosa could be identified according to their primary function, Masticatory mucosa, Lining mucosa & Specialized mucosa. I-Masticatory mucosa (Keratinized mucosa) During mastication, parts of oral mucosa are subjected to forces & pressure, these are a) Gingiva b) Mucous membrane covering the hard palate. II-Lining mucosa (Non-keratinized mucosa) Present in areas not subjected to high levels of friction but is mobile & distensible. It serves a protective lining & subdivided into: Firmly attached to the underlying muscles Lip. Cheek. Inferior surface of the tongue. Soft palate Loosely attached to the underlying structures as bone, fascia or muscle Alveolar mucosa. Vestibular fornix. Floor of the mouth. III-Specialized mucosa This is represented by the mucous membrane covering dorsal surface of tongue. It is a highly specialized structure, because of the presence of different types of papillae, taste buds & lingual tonsils.
- The cells of the stratum intermedium contain Odland bodies with their size; shape and location are different from those found in keratinized epithelium.
- Simple Squamous Epithelium Is composed of flattened, irregularly-shaped cells forming a continuous surface which is often referred to as pavemented epithelium. Like all epithelia, this delicate lining is supported by an underlying basement membrane.
- Simple Squamous Epithelium This micrograph of a small B.V. illustrates the typical appearance of simple squamous epithelium in section; the epithelial lining cells E (known as endothelium in the circulatory system) are so flattened that they can only be recognized by their nuclei which bulge into the vessel lumen.
- Stratified Squamous Epithelium Consists of a variable number of cell layers. Stratfied epithelia are defined as epithelia consisting of 2 or more layers of cells. In contrast to simple epithelia, stratified epithelia have a protective function & the degree & nature of the stratification is related to the kinds of physical stresses to which the surface is exposed.
- This specialized form of stratified squamous epithelium constitutes the epithelial surface of the skin & is adapted to withstand the constant abrasion & desiccation to which the body surface is exposed. During maturation, the epithelial cells undergo a process called keratinization resulting in the formation of a tough, non-cellular layer consisting of the protein, keratin K, & the remnants of degenerate epithelial cells.
- PAS stained section
- An important property of epithelium is its ability to function as a barrier that depends to a great extent on the close contact or cohesiveness of epithelial cells. Cohesion between cells is provided by viscous intercellular material consisting of protein-carbohydrate complexes produced by epithelial cells themselves. In addition, there are specialized modifications of the adjacent membranes of epithelial cells, the most common of which is Desmosome. Adhesion between epithelium & C.T. is provided by the hemidesmosomes present on the basal membranes of the cells of the basal layer. These also possess intracellular attachment plaques into which tonofilaments are inserted. Two other types of junction are seen between the cells of oral epithelium. The gap junction is a region where the membranes of adjacent cells run closely together, separated by only a small gap. The cells are closely attached to each other by one or more type of cellular junction (tight, gap & desmosomal junction) & also to the B.M. by hemi-desmosomes. The hemi-desmosome consists of a single attachment plaque, in which tonofilaments are attached, plasma membrane & an extracellular structure attached to the B.M. The desmosomes are specialized structure of the cell surface consisting of adjacent cell membranes, a pair of intracellular attachment plaque with tonofilaments & an intervening extracellular structure.
- KERATINIZED EPITHELIUM Found in areas of oral mucosa as gingiva & mucosa of hard palate, which are subjected directly to mechanical irritating effect of food during mastication. The epithelial cells that ultimately keratinize are called keratinocytes or keratocytes. Keratinocytes constitute the major part of epithelial cells population. The cells are arranged in different layers of several rows & during maturation they either change to keratin or share in keratin formation. These cells have the following criteria:- Always present in sheets & attached to each other by one or more type of cellular junctions. The cytoplasm of these cells is stained with ordinary stain as H & E. Their cytoplasm contains the characteristic tonofilaments. These cells are arranged in 4 layers, basal (stratum basal), spinous (stratum spinosum), granular (stratum granulosum) & cornified (stratum cornium). These layers bear their names from their morphological appearance. Each layer consists of several rows of cells except the basal layer, which is formed of one row of cuboidal or columnar cells. The basal cells & the following few rows of spinous layer cells undergo mitosis producing new cells that match those lost at the surface by desquamation. These cells may remain in their place & divide again or migrate upward & become spinous, granular cells & finally they change to keratin. During their migration, the cells become more specialized & undergo biochemical & morphological changes. These cells of basal & deeper 2-3 layers of spinous layers are named stratum germinativum. The basal cell layer represents the least differentiated cells of epithelium; the cells are either cuboidal or columnar & are arranged in one row on a well-defined B.M. The cell posses not only the usual cell organelles seen in other cell but also a characteristic tonofilaments. The later are fine intracellular protein strands, arranged in bundles that form the tonofibrils. The cells are closely attached to each other by one or more type of cellular junction (tight, gap & desmosomal junction) & also to the B.M & an extracellular structure attached to the B.M Desmosomes are specialized structure of the cell surface consisting of adjacent cell membranes, a pair of intracellular attachment plaque with tonofilaments & an intervening extracellular. These cells show the first stage of maturation. The spinous cell layer consists of several rows of polyhedral cells of different shape & size & larger than basal cells. The basal cells & the spinous cells constitute more than 1/2 the thickness of epithelium. The cells of spinous layer are joined together by intercellular bridges giving the cells a prickly appearance. The inter-cellular spaces are wide compared with that in the non-keratinized epithelium. The granular cell layer lies above prickle cell layer & is made up of several rows of flattened epithelial cells. The cells show a further increase in maturation compared with those of strata basal & spinosum. The cells contain large numbers of small granules called keratohyaline granules. This is associated with the development of a barrier in epithelium that limits the movement of substances between cells. The cornified layer in keratinized epithelium is the final stage in the maturation. Cells of stratum corneum may be termed epithelial squames; these are cells that shed, necessitating the constant turnover of epithelial cells. Desmosomes weaken & disappear to allow for this desquamation. Stratum corneum provides mechanical & chemical protective function to the mucosa.
- Non-keratinized oral epithelium In regions of oral mucosa that are covered by this type of epithelium, the latter shows absence of both keratin & granular cell layers. The epithelium is thicker & the superficial 1/2 of epithelium shows changes which distinguishes them from basal & prickle cells. These include increase in size, accumulation of glycogen & occasionally the presence of keratohyaline granules surrounded by ribosomes, which appear more regular & not associated with tonofilaments. Function of keratohyaline granules appear to be associated with thickening of cell membrane. This specialization permits classification of prickle cell layer into 2 regions, the superficial layers, stratum superficial & deeper layer, stratum intermedium. The cells of both strata are larger & tightly Packed together, the intercellular spaces are nearly absent & hence, absence of prickly appearance.
- Non-Keratinocytes in Oral Epithelium These cells are present in both keratinized & non-keratinized epithelium & constitute about 10% of the epithelial cell population. These cells have the following criteria: 1- Appear as clear cells by ordinary H&E stain, they need special stains. 2- Present as scattered cells & not in sheets. 3- A clear hallows around their nuclei. 4- Their cytoplasm is free from tonofilaments. 5- No cellular junctions. 6- They do not play any role in synthesis of keratohyaline granules or keratin.
- Non-keratinocytes are four types of cells A- Pigment cells B- Langerhan's cells C- Merkel cells D- Inflammatory cells A- Pigmentation & pigment cells There is a direct relationship between the degree of melanin pigmentation seen in skin & oral mucosa, where the most commonly pigmented regions are lips, gingiva & buccal mucosa. Pigmentation of gingiva occurs mostly in attached gingiva beneath interdental papilla. This pigmentation is produced by specialized cells called melanocytes or melanoblasts; they are derived from neural crest cells. They are chiefly found in basal or parabasal layers. The cytoplasm of these cells appears clear after staining with H&E., so these cells may also be termed dendritic or clear cells. The melanocytes synthesize melanin pigments in the presence of tyrosinase enzyme. The melanin pigment is found in the form of fine granules ranging in color from light brown to almost black. The melanin granules appear as groups of small granules called melanosomes. These granules pass into adjacent keratinocytes where they are stored, these cells are called melanophores. Also other cells containing melanin may be seen in the C.T. beneath normal pigmented epithelial cells. They represent macrophages containing melanin & called melanophages. B- The Langerhan's cells Is another dendritic clear cell present in upper layers of epidermis & oral epithelium & termed high level cell but they can also be found in the deeper layers of epithelium. Like the melanocyte, langerhan's cells lack tonofilaments & desmosomes but they do not synthesize melanin. They contain a characteristic rod-shaped body called the langerhan's granule. These cells may be demonstrated histologically by gold chloride. They have been variously described as neural elements, as degenerated melanocytes, as intra epithelial macrophages & as regulatory cells controlling epithelial cell division & differentiation. C- The Markel cells Markel cells appear histologically as clear cells situated basally in oral epithelium. They do not have the dendritic shape characteristic of melenocyte & langerhan's cells. They migrate from neural crest cells. D- Inflammatory cells Lymphocytes & P.N.L. are also found at various levels of the epithelium. These cells are & can pass through the epithelium to the surface lamina propria of gingiva.
- Racial pigmentation Linear increase in melanin pigmentation of basal keratinocytes
- Melanocytes Silver staining shows the pigmented basal keratinocytes & dentritic processes of melanocytes. Fontana stain
- KERATINIZED EPITHELIUM This type is found in the areas of oral mucosa as gingiva & mucosa of hard palate, which are subjected directly to mechanical irritating effect of food during mastication. The epithelial cells that ultimately keratinize are called keratinocytes or keratocytes. Keratinocytes constitute the major part of epithelial cells population. The cells are arranged in different layers of several rows & during maturation they either change to keratin or share in keratin formation. These cells have the following criteria:- Always present in sheets & attached to each other by one or more type of cellular junctions The cytoplasm of these cells is stained with ordinary stain as H & E Their cytoplasm contains the characteristic tonofilaments
- 1- Masticatory mucosa Gingiva: Topography & Macro-Anatomy Gingiva is that part of m.m. which surrounds teeth & covers part of alveolar bone from vestibular & lingual surfaces of both jaws. Gingiva is sharply limited from alveolar mucosa by scalloped line, the mucogingival junction; it is called also the healthy line. A similar line of demarcation is found on lingual aspect of mandible, while on the palate the gingiva merges with palatal mucosa & no distinct mucogingival junction is present. Gingiva is pale pink in color; in colored races the gingiva is pigmented. The degree of pigmentation is proportional to that of skin. Morphologically, gingiva is divided into free gingiva, attached gingiva & interdental papilla Free gingiva: is represented by that portion which extends along the cervical level of tooth at labial, buccal & lingual surfaces. It is freely movable & extends to bottom of gingival sulcus or slightly below its level, the free gingiva tapers to a knife-edge; the gingival margin. Free gingiva is marked off from attached gingiva by a shallow groove, called the free gingival groove. This groove is about 1.0 to 1.5 mm far from the actual gingival margin & follows its contour both labially & lingually. The free gingival groove is caused by functional impacts upon the free gingiva folding the movable free part back upon the attached & immovable zone. Gingival sulcus: Is a shallow groove lined by non-keratinized epithelium, the bottom of which is at the point of separation of attachment epithelium from tooth. The depth of gingival sulcus under normal conditions varies from 0-6mm, 45% of all measured sulci were below 0.5 mm the average being 1.8 mm. The shallower the sulcus the more favorable is the condition at gingival margin. Lymphocytes & plasma cells are seen in the C.T at bottom of gingival sulcus. Attached gingiva: is immovably anchored to underlying cementum or periosteum. It extends from free gingival groove to mucogingival junction, which separates it from underlying alveolar mucosa. The surface of attached gingiva shows the characteristic stippling resembling that of an orange peel. This stippling is a functional adaptation to mechanical impacts. The attached gingiva appears slightly depressed between adjacent teeth corresponding to the depression on alveolar process between eminences of sockets. Absence of stippling of attached gingiva is an indication of inflammation. Interdental papilla: portion of gingiva, which fills the interproximal space between two adjacent teeth & thus extends below the contact area. In cases where there is no contact point, the interdental papilla is reduced. The interdental papilla simulates a tent shape from the labial or buccal side, while lingually it is wedge in shape & the base corresponds to a line connecting the margin of the gingiva at center of one tooth to center of the next. The apex tapers to the contact area or point. Deep to interdental gingival tissue are transeptal fibers of P.L & then crest of interdental septum of bone. Beneath the contact areas the height of interdental papilla is less than that found lingually & labially, or buccally. Interdental gingival tissue found in the depression between the two peaks of interdental papilla is called col this col usually lacks keratinizations. Histology of Gingiva Gingiva is formed of surface epithelium & underlying L.P. 3 types of gingival epithelium exists according to behavior of keratin. 1- Orthokeratinized epithelium: stratum corneum consists of flat tightly packed scales & the nuclei are completely absent. 2- Pararkeratenized epithelium: the stratum corneum consists of flat horny scales, which retain pyknotic nuclei or remnants of nuclear material. This type constitutes 75%. 3- Nonkeratenized epithelium: The stratum corneum is absent. The sheltered areas of gingiva are always non-keratinized, & these are the epithelial lining of gingival sulcus & the epithelium of the col. Lamina Propria: made of dense C.T. composed of bundles of collagenous fibers, fibroblasts, B.Vs, lymphatics & nerves. The lamina propria consists of papillary layer & a reticular layer. The papillary layer is formed of tall, numerous & slender papillae. Few elastic fibers are confined to walls of B.Vs. The reticular layer is formed of same kind of tissue, the fibers being arranged in a delicate network. Lamina propria of gingiva contains dense bundles of collagen whose function include support of free gingiva, binding of attached gingiva to alveolar bone & tooth, & linkage of teeth one to another. These principal fiber groups have been given names based upon their orientation & attachments, & called gingival ligament. Their main function is to provide support for gingiva against tooth & alveolar bone surface, resisting masticatory loads, & the component of this ligament are:-
- DENTO-GINGIVAL JUNCTION The components of gingiva both epithelium & L.P. are attached to the tooth & both contribute to security of dentogingival junction. The epithelial portion of gingiva, which is in direct contact with surface of tooth, is called attachment epithelium or junctional epithelium. This epithelium is an epithelial collar that surrounds the tooth & normally extends from bottom of gingival sulcus towards the C.E.J & often surpasses the C.E.J. The length of attachment epithelium of tooth in adult varies from 1-3 mm, which is nearly equal to the distance between the apical end of attachment epithelium & crest of alveolar bone. HISTOLOGICAL STRUCTURE Coronally; the junctional epithelium may be 15-30 cells thick, whilst apically it narrows to only 1-3 cells thick. It consists of 2 zones; a single cell layer of cuboidal cells (the stratum germinativum) overlying several layers of flattened cells equivalent to a stratum spinosum. There is no stratum granulosum or corneum. The cells of the stratum germinativum rest on a typical lamina propria which shows many capillaries & appears to be more cellular than other parts of the gingiva. The C.T. interface is smooth. The cells of the junctional epithelium immediately adjacent to the tooth attach themselves to tooth (enamel or cementum) in the same way as cells of the stratum germinativun elsewhere attach themselves to lamina propria (i.e. by hemidesmosomes within the cell & a basal lamina produced by epithelial cells. This combination of hemidesmosomes & basal lamina is known as attached apparatus or epithelial attachment. The basal lamina in contact with the tooth is termed the internal basal lamina.
- 1- Dentogingival fibers; it is part of the P.L. & it arise from the root surface above alveolar crest & radiate to insert into the lamina propria of gingiva. The most superficial fibers lie beneath the sulcular epithelium. 2- Circular fibers encircle each tooth within the marginal & interdental gingiva, some attach to cementum, some to alveolar bone, some cross interdentally to join the fiber group of adjacent tooth. 3- Alveologingival fibers; run from crest of alveolar bone & interdental septum radiating coronally into overlying L.P. of gingiva 4- Dentoperiosteal fibers; occur only in labial, buccal & lingual gingiva. They arise from cementum & pass over the alveolar crest to insert into periostium. 5- Transeptal fibers pass horizontally from the root of one tooth, above alveolar crest to be inserted into the root of adjacent tooth. Such fibers provide an anatomical basis for linking all the teeth in the dentition 6-Semicircular fibers emanate from cementum near the cemento-enamel junction, cross the free marginal gingiva, & insert into a similar position on the opposite side of the tooth. 7- Transgingival fibers reinforce the circular & semicircular fibers. The fibers arise from the cervical cementum & extend into the marginal gingiva of the adjacent tooth, merging with the circular fibers. 8- Interdental fibers pass through coronal portion of interdental gingiva in buccolingual direction, connecting buccal & lingual papillae. 9- Vertical fibers arise in alveolar mucosa or attached gingival & pass coronally towards marginal gingiva & interdental papilla. 10- Longitudinal fibers extend for long distances within the free gingival, some for the whole length of the arch
- B) Hard palate It is keratinized masticatory mucosa. It is pink in color which is firmly attached to underlying structures Macro-Anatomy of hard palate The palate is characterized by the presence of 4 different regions:- 1- Palatine gingiva Adjacent directly to the teeth which is similar to the previously described gingiva but mucogingival junction is not present. 2- Median palatine raphe Extends from the palatine papilla posteriorly. Palatine papilla (incisive) is pear shaped & is formed of dense C.T. that contains the oral part of naso-palatine duct (this duct is lined by simple or pseudostratefied columnar epithelium rich in goblet cells). In median palatine raphe, it is difficult to differentiate between lamina propria & submucosa. Radiating from this raphe, transverse folds called palatine rugea which is formed of dense C.T. covered by epithelium. 3- The anterolateral area (fatty zone) This area present between the raphe & the gingiva anteriorly. Its lamina propria is fixed to periosteum by bands of fibrous C.T. dividing the submucosa into compartments containing fat cells. 4- The postero-lateral area (glandular zone) - Present posterior to the fatty zone. - The submucosa contains pure mucous glands. The fatty and glandular zones act as cushion. The C. T. of hard palate is thick anteriorly than posteriorly. Anterior palatine B.Vs. are present in sulcus between alveolar process & H.P, where they are surrounded by loose C.T.
- Nasopalatine Duct Cyst:- Typical presentation with a dome-shaped bluish enlargement overlying the incisive canal.
- Non-keratinized oral epithelium The oral mucosa that are covered by this type of epithelium shows absence of both keratin & granular cell layers. The epithelium is thicker & superficial 1/2 of epithelium shows changes which distinguishes them from basal & prickle cells. These include increase in size, accumulation of glycogen & occasionally the presence of keratohyaline granules. Function of keratohyaline granules appear to be associated with thickening of cell membrane. This specialization permits classification of prickle cell layer into 2 regions, the superficial layers & deeper layer. The cells of both strata are larger & tightly packed together, the intercellular spaces are nearly absent & hence, absence of prickly appearance. A) Lining mucosa (firmly attached) These are the mucous membrane covering muscles and they are firmly attached to the epimysium or fascia, in these regions the mucosa is elastic. These 2 characteristics permit the mucosa to maintain a relatively smooth surface during muscular movements & prevent its elevation into folds & lodging them between biting surfaces of teeth during mastication. 1- Inferior surface of tongue - Covered by thin non-keratinized epithelium with short & numerous C.T. papillae. - The submucosa can not be differentiated as a separate layer where it connects the mucous membrane to the C.T. surrounding tongue muscles. 2- Soft palate - Its epithelium is continuous with that of hard palate but non-keratinized So between them there is a healthy line. - Its epithelium forms the nasal side is pseudostratified columnar ciliated epithelium with goblet cells. - It is highly vascularized & red in color. - Lamina propria is thin with few & short papillae. - A continuous layer of elastic fibers separating lamina propria from submucosa. - The submucosa contains fat cells & mucous glands. 3- Cheek The epithelium is non-keratinized stratified squamous epithelium. C. T. papillae are short, irregular with few elastic fibers. In submucosa & between the buccinator muscle bundles small mixed salivary gland present. Sometimes isolated sebaceous glands may present in the C.T. lateral to the mouth corner (called Fordyce granules or spots). The firm attachment of cheek mucosa to the muscles prevents its biting especially during mastication. 4- Lip Formed of 3 surfaces. lining mucosab) transitional zone. c) skin side. a) Lining mucosa Similar to that of cheek except: 1-Submucosa contains fat cells & mixed S.Glands. on surface of orbecularis oris muscle. 2- No Fordyce spots. b) Transitional zone Lying between lining mucosa and skin side of lip. Present only in human race and represented as red zone called vermillion border. Covered by stratified squamous epithelium with thin layer of keratin. C.T. papillae are numerous, long and densely arranged, these deep papillae carry large capillary loops, so the thin layer of epithelium permits the red color of blood. One or two sebaceous glands may be present. c) The skin side Consists of: 1- Epidermis Formed of stratified squamous keratinized epithelium with hair, sweat and sebaceous glands. The epithelium is similar to that of keratinized mucosa except that; there is additional layer present between granular cell layer and the keratinized layer called stratum lucidum. The stratum lucidum is a pale translucent layer formed of 2-3 layers of flat cells, with very small nucleus and indistinct boundaries. Melanoblasts present in between the basal cell layer (in black races they may fill all epithelial layers & even C.T. papilla). The hair follicle Has a shaft projected above the surface & root embedded in an invagination of epidermis called hair follicle. The root terminates in an expansion called hair bulb. An upward invagination of C.T. to hair bulb called hair papilla. One or two sebaceous glands open in the neck of the hair follicle. Sweat glands also present and consist of coiled secretory part and duct which formed of single cuboidal or pyramidal cells with large nucleus. Myoepithelial cells present between basement membrane & secretory cells. 2- The dermis Formed of dense C. T. with few and short papillae. It is formed of:- Reticular layer contains Collagen fibers arranged in network with less no. of cells. The layer contains thin elastic fibers. Papillary layer contains Irregularly arranged collagen fibers with more cells. The layer contains thick elastic fibers B) Loosely attached 1- Alveolar mucosa Covers outer surface of alveolar bone & attached loosely to periostum. Covered by stratified squamous non-keratinized epithelium. C.T. papillae are short or even missing. The collagen fibers of lamina propria are regularly interwoven. Submucosa may contain small mixed salivary gland. Elastic fibers are thin in lamina propria & thick in submucosa 2- Vestibular fornix It allows the free mobility of lips & checks. It permits movement of lip & cheek, & covered by stratified squamous non-keratinized epithelium. C.T. papillae are short & few. Labial frenum (median & lateral) is folds of m.m. contain loose C.T. with no muscle fibers. 3- Floor of mouth Allows free mobility of tongue. Covered by thin stratified squamous non-keratinized epithelium. C.T. papillae are few & short. Submucosa contains fat cells. Sublingual & submandibular ducts are present near the covering mucosa in sublingual folds.
- Specialized mucosa Dorsal surface of tongue, which is divided by V- shaped sulcus terminalis into papillary part (ant 2/3) & lymphatic part (post 1/3) Anterior 2/3 of tongue Its dorsal surface contains papillae & taste buds.
- Dorsum of tongue is covered by very thick keratinized epithelium, & the presence of papillae can make the microscopical appearances particularly variable. Filiform papillae are the most numerous & cover the whole dorsal surface of anterior 2/3 of tongue. They are conical with central C.T core covered by keratinized stratified squamous epithelium. Fungiform papillae are much less numerous & form smooth red elevations covered by non-keratinized epithelium. Vallate or cirumvallate, which are about 10-12 in number, are found in front of sulcus terminalis, the V-shaped groove which separates posterior 1/3 of tongue from anterior 2/3. Each vallate papilla is surrounded by a deep circular groove & small serous glands open into the base of the groove. Taste buds are present in the lateral wall of each papilla.
- Types of tongue papillae 1- Filiform papillae - Found on dorsal surface of tongue, as high, narrow conical structures that arranged in parallel rows & near post. 1/3 the rows become parallel to sulcus terminalis. - The papilla is composed histologically from central core of C.T. covered by keratinized epithelium. - The primary papilla sends up 1-2 secondary papillae, where the epithelium over them becomes hornified. - This papilla dose not contains taste buds. 2- Fungiform papilla - Present on dorsal surface of tongue in between filiform papillae & they are numerous at the tip of tongue & its lateral border. - The papilla is mushroom like, narrow at the base with smooth rounded top. - Histologically it composed of central core of primary C.T. papilla & covered by stratified squamous non-keratinized epithelium. - The secondary C.T. papillae make the blood vessels near to the surface epithelium so this papilla appears red in color. - This papilla contains 1-2 taste buds at its lateral wall. The papillae on the tip of tongue responsible for sweet sensation. The papillae on lateral borders responsible for salt sensation. Chorda tympani responsible for theses sensation. 3- Circumvallate papillae Are (7-12 in no.) present on dorsal surface of tongue anterior to sulcus terminalis. - They do not protrude above the surface of tongue but embedded in tongue & surrounded by deep trough, the taste buds located at the lateral wall of papilla & also at the lateral wall of trough. - In the base of the trough the von Ebner salivary gland ducts open. - The papilla has narrow base & wide surface with central core of C.T which sends secondary C.T papillae to the stratified squamous non-keratinized epithelium. ● Circumvallate papillae responsible for the bitter sensation, by the glossopharyngeal nerve. 4- Foliate papillae - They are ill developed in human (rudimentary) but are large in some animals. - Present as sharp parallel clefts on lateral sides & anterior to sulcus terminalis. - These clefts are bordered by narrow folds of mucous membrane at which taste buds are found. The von Ebner salivary gland opens in the clefts of these papillae. - Foliate papillae responsible for Sour sensation by glossopharyngeal nerve.
- Taste bud ♦ Present in 1) All tongue papillae except filiform. 2) Soft palate. 3) Posterior surface of epiglottis. ♦ They are intraepithelial structure, barrel or ovoid with rounded base resting on B.M & end with narrow opening toward the epithelial surface & called taste pore. Flattened small epithelial cells surround the taste pore. Histology of the taste bud Each taste bud is composed of about 3 modified epithelial cell type. Outer supporting (sustentacullar) cells arranged like layers of onion & are in contact with neighboring epithelial cells. Inner supporting (sustentacular) cells, they are shorter & rode shape cells. Taste cells (Neuroepithelial cells) they are 11-12 in number & present between the inner supporting cells. These cells are slender with dark stained nucleus & apically stiff bristle-like process extends to the space beneath taste pore. Nerve plexus present in C.T. below the taste bud, some fibers enter it & end in contact with the taste cells. Posterior 1/3 of the tongue Other names: Root, lymphatic or pharyngeal part. Lingual tonsil Present as small rounded or oval elevations due to aggregation of lymphatic nodules in underlying C.T known as lingual follicles.
- Lingual tonsil Present as small rounded or oval elevations due to aggregation of lymphatic nodules in underlying C.T known as lingual follicles. Histologically - Lingual follicles covered by St Sq Epith (non-keratinized) which extended down in many sites to form lingual crypt. The lymphatic tissue surrounds the crypt & composed of germinal centers & lymphatic tissue fills the spaces between these centers. - Ducts from underlying Weber mucous salivary gland open into the bottom of lingual crypt. - Lingual tonsil forms a part of the lymphatic ring between mouth & nose from one side & pharynx on the other side.
- Shift of Dento-Gingival junction (stages of passive eruption) When the tooth first erupts; enamel is almost covered by epithelium. By further eruption & gingival recession, more of the tooth will be exposed in oral cavity. Active eruption: The actual movement of teeth towards occlusal plane. Passive eruption: It is the gradual exposure of the crown by separation of attached epithelium from tooth surface. Passive eruption has 4 stages where the 1st & 2nd stages considered normal & 3rd & 4th stages may be normal or pathologic. First stage Occur in primary teeth till one year before shedding; in the permanent teeth till 20-30 years. Coronal end of primary attachment epithelium present on the enamel & the apical end on the C.E.J. Clinical crown is < than anatomical crown. Second stage Occur till the age of 40 years or even later. The coronal end is still on the enamel & the apical end on cementum. The clinical crown is less than the anatomical crown. Third stage It is a transient stage. The coronal end present at the C.E.J & apical end on cementum. The clinical crown equal to the anatomical crown. Fourth stage From 60 years or even later. The coronal and the apical ends present on the cementum. The clinical crown is longer than the anatomical crown. Epithelial attachment (mode of attachment) The attachment of epithelium to tooth surface is so strong that an attempt to detach the gingiva from tooth surface the junctional epithelium will tear rather than peel off from the tooth surface. This firm union is achieved by what is called epithelial attachment.
- Second stage Occur till the age of 40 years or even later. The coronal end is still on enamel & apical end on cementum. Clinical crown is < than anatomical crown.
- Third stage It is a transient stage. Coronal end present at C.E.J & apical end on cementum. Clinical crown = anatomical crown.
- Fourth stage From 60 years or even later. The coronal & apical ends present on cementum. Clinical crown is > than anatomical crown