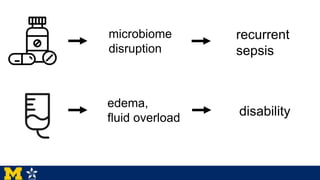
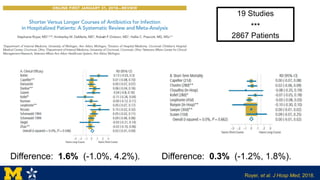
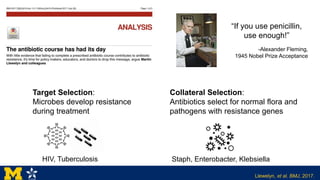
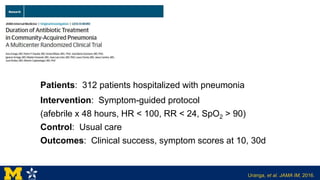
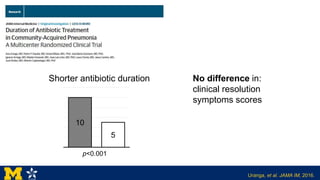
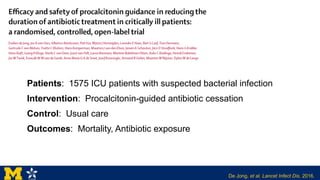
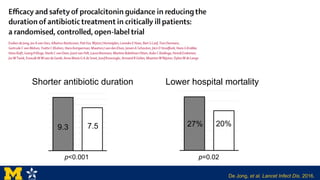
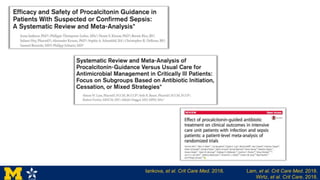
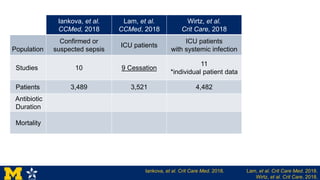
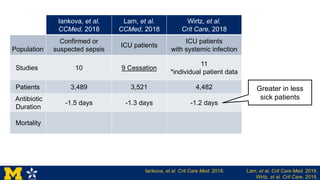
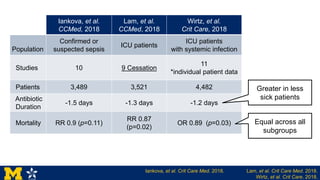
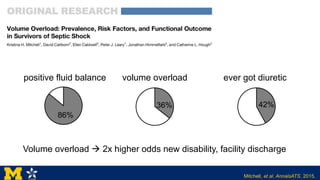
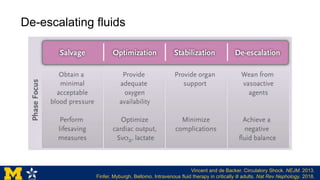
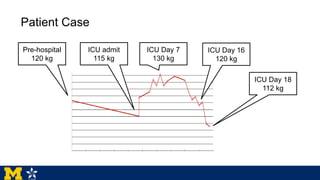
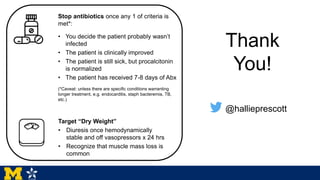
Dr. Hallie Prescott's presentation addresses the importance of de-escalating antibiotic treatment and managing fluid overload in patients with sepsis and critical illness. Evidence suggests that shorter courses of antibiotics are safe and can effectively limit the development of resistance, while careful management of fluid balance is vital to minimize complications like new disability. The proposed approach includes stopping antibiotics based on specific clinical criteria and emphasizing the restoration of euvolemia after stabilization.