BDSRA 2015 CLN10 Burrow, Spaeth, Sisk, Hallinan
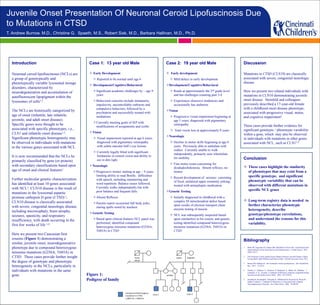
- 1. Introduction Neuronal ceroid lipofuscinoses (NCLs) are a group of genotypically and phenotypically variable lysosomal storage disorders, characterized by neurodegeneration and accumulation of autofluorescent lipopigment within the lysosomes of cells1,2. The NCLs are historically categorized by age of onset (infantile, late infantile, juvenile, and adult onset disease). Specific genes were thought to be associated with specific phenotypes, i.e., CLN1 and infantile onset disease1,2. Significant phenotypic heterogeneity may be observed in individuals with mutations in the various genes associated with NCL. It is now recommended that the NCLs be primarily classified by gene (or protein) with secondary classifications based upon age of onset and clinical features1. Further molecular genetic characterization has identified at least 10 genes associated with NCL3. CLN10 disease is the result of mutations in the lysosomal aspartic protease cathepsin D gene (CTSD) 1. CLN10 disease is classically associated with severe, congenital neurologic disease, including microcephaly, brain atrophy, seizures, spasticity, and respiratory insufficiency, with death occurring in the first few weeks of life 1,4. Here we present two Caucasian first cousins (Figure 1) demonstrating a similar, juvenile onset, neurodegenerative phenotype due to compound heterozygous missense mutations (G256A; T685A) in CTSD. These cases provide further insight the degree of genotypic and phenotypic heterogeneity in the NCLs, particularly in individuals with mutations in the same gene. Case 1: 13 year old Male Early Development Reported to be normal until age 6 Development/Cognitive/Behavioral Significant academic challenges by ~ age 9 years Behavioral concerns include immaturity, impulsivity, uncontrollable outbursts and compulsive behaviors; followed by a psychiatrist and successfully treated with mediations Currently meeting goals of IEP with modifications of assignments and scribe Vision Visual impairment reported at age 6 years; diagnosed with pigmentary retinopathy with subtle macular bull’s eye lesions Currently legally blind with significant limitations in central vision and ability to see in dim light Neurologic Progressive tremor starting at age ~ 9 years, limiting ability to read Braille; difficulties with speech, including stammering and word repetition. Balance issues followed. Currently walks independently but with poor balance and frequent falls. Absent Reflexes Parents report occasional full body jerks; staring spells noted by teachers Genetic Testing Based upon clinical features NCL panel was performed; identified compound heterozygous missense mutations (G256A; T685A) in CTSD Case 2: 19 year old Male Early development Mild delays in early development Development/Cognitive/Behavioral Reads at approximately the 2nd grade level and has challenges counting past 3-4 Experiences obsessive tendencies and occasionally has outbursts Vision Progressive visual impairment beginning at age 5 years; diagnosed with pigmentary retinopathy Total vision loss at approximately 8 years Neurologic Decline in motor skills beginning at age 6 years. Previously able to ambulate with walker. Currently unable to walk independently, primarily uses wheelchair for mobility Fine motor exam concerning for dysdiadochokinesia. Absent reflexes; no tremor Recent development of seizures consisting of focal, unilateral upper extremity jerking; treated with antiepileptic medication Genetic Testing Initially diagnosed in childhood with a complex III mitochondrial defect based upon results of electron transport chain enzyme testing of muscle NCL was subsequently suspected based upon similarities to his cousin, and genetic testing identified compound heterozygous missense mutations (G256A; T685A) in CTSD Bibliography 1 Mink JW, Augustine EF, Adams HR, Marshall FJ, Kwon JM. Classification and Natural History of the Neuronal Ceroid Lipofuscinoses. J Child Neurol. 2013. 28(9):1101-5. 2 The Neuronal Ceroid Lipofuscinoses (Batten Disease), Second Edition, Edited by Sara Mole, Ruth Williams and Hans Goebel . Oxford University Press, 2011. 3 Bennet MJ, Rakheja D. The Neuronal Ceroid-Lipofuscinoses. Dev Disabil Res Rev. 2013. 17:254-9. 4 Siintola, E., Partanen, S., Stromme, P., Haapanen, A., Haltia, M., Maehlen, J., Lehesjoki, A.-E., Tyynela, J. Cathepsin D deficiency underlies congenital human neuronal ceroid-lipofuscinosis. Brain. 2006. 129:1438-45. 5 Steinfeld R, Reinhardt K, Schreiber K, Hillebrand M, Kraetzner R, Bruck W, Saftig P, Gartner J. Cathepsin D Deficiency is Associated with a Human Neurodegenerative Disorder. Am J Hum Genet. 2006. 78:988-98 Conclusion These cases highlight the similarity of phenotypes that may exist from a specific genotype, and significant phenotypic variability that can be observed with different mutations in specific NCL genes Long-term registry data is needed to further characterize phenotypic heterogeneity, describe genotype/phenotype correlations, and understand the reasons for this variability. Juvenile Onset Presentation Of Neuronal Ceroid Lipofuscinosis Due to Mutations in CTSD T. Andrew Burrow, M.D., Christine G. Spaeth, M.S., Robert Sisk, M.D., Barbara Hallinan, M.D., Ph.D. Discussion Mutations in CTSD (CLN10) are classically associated with severe, congenital neurologic disease. Here we present two related individuals with mutations in CLN10 demonstrating juvenile onset disease. Steinfeld and colleagues previously described a 17-year-old female with a childhood onset disease phenotype, associated with progressive visual, motor, and cognitive impairment5. These cases provide further evidence for significant genotypic / phenotypic variability within a gene, which may also be observed in individuals with mutations in other genes associated with NCL, such as CLN11,2. Figure 1: Pedigree of family
