8 Lower Respiratory Infections
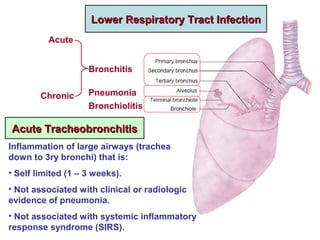
- 1. Bronchiolitis Bronchitis Pneumonia Acute Chronic Lower Respiratory Tract InfectionLower Respiratory Tract Infection Acute TracheobronchitisAcute Tracheobronchitis Inflammation of large airways (trachea down to 3ry bronchi) that is: • Self limited (1 – 3 weeks). • Not associated with clinical or radiologic evidence of pneumonia. • Not associated with systemic inflammatory response syndrome (SIRS).
- 2. • SIRS: > 2 criteria of: - Temp > 38 O C. - Pulse > 90 b/min. - RR > 20 b/min. - WBCs > 12,000 cells/mm3 . • Epidemiology: - Affects > 5% of adults annually. - More in cold season. - Viral in most cases, but usually empirically treated with antibiotics. • Treatment: - Rest, expectorants, mucolytics, antipyretics. - Antimicrobials if indicated: o Antibiotics: Azithromycin 500 mg tab once daily for 3 days. Or Doxycycline 100 mg/12 h for 5 days. o Antivirals: Oseltamivir (Tamiflu) tab 75 mg twice daily for 5 days (during seasonal outbreaks of influenza).
- 3. Pneumonitis Pneumonia Pneumonitis: broad term for inflammation of the lung. Pneumonia: used more specifically to indicate inflammation of lung parenchyma which is: • Caused by an infectious agent. • Leads to formation of an inflammatory exudate inside the alveoli. • Leads to loss of aeriation of lung tissue. This is referred to as hepatization (pathology) or consolidation (clinical). (Patchy) (Confluent)
- 4. Clinical Types of Pneumonia • Health Care Associated Pneumonia (HCAP): Diagnosed if the patient: - Was hospitalized for > 2 days within the last 3 months. - Lives in a nursing facility. - Was repeatedly exposed to a medical facility (hemodialysis, wound care, IV antibiotics or chemotherapy) • Hospital Acquired Pneumonia (HAP) (Nosocomial Pneumonia): develops: - > 48 hh after hospitalization (not incubating at time of admission). - Soon after discharge from hospital. - Ventilator Associated Pneumonia (VAP): a subtype of HAP: It develops > 48 hh after start of mechanical ventilation. • Community Acquired Pneumonia (CAP): acquired outside the above circumstances (unrelated to healthcare).
- 5. Epidemiology • Commonest potentially lethal acute infection. • A leading type of nosocomial (hospital- acquired) infection. • Commoner and more risky at extremes of age (< 2, > 65 y). • CAP is commonly preceded by a viral respiratory tract infection → o ↑ Adherence of bacteria to respiratory epithelial cells. o ↓ Mucociliary clearance. • HAP is responsible for 25% of ICU admissions. • VAP is the most frequent ICU acquired infection. • Aspiration pneumonia may be community or hospital acquired, though it more typically occurs in hospitals or extended care facilities.
- 6. Community Acquired Pneumonia (CAP)Community Acquired Pneumonia (CAP) Route of Infection• Microaspiration Unrecognized microaspiration is the usual route of infection for typical CAP caused by S. pneumoniae and H. influenzae. Some degree of microaspiration normally occurs during sleep. If upper airways are colonized or infected, small amounts of oral or pharyngeal secretions that are aspirated will carry the bacteria to the alveoli where they trigger the pneumonic process. • Inhalation as in transmission of: - Viral pneumonia. - Tuberculosis. • Haematogenous Spread as in Staph. aureus pneumonia. • Direct Extension from pleura or subdiaphragmatic space.
- 7. Microorganisms Common • Streptococcus pneumoniae (pneumococci): commonest and most typical. • Haemophylus influenzae. • Influenza virus, other respiratory viruses • Satphylococcus aureus • Mycobacterium tuberculosis Less Common • Moraxella catarrhalis. • Pseudomonas aeroginosa. • Klebsiella. • Mycoplasma. • Chlamydia (C. pneumoniae and C. psittaci) • Legionella. • Fungi Atypical organisms as Mycoplasma, Chlamydia, fungi are not revealed by ordinary Gram stain and culture.
- 8. Predisposing Conditions for Particular Organisms • Smoking, COPD predispose to CAP with typical organisms (S. pmeumoniae, H. influenzae, M. catarrhalis) as well as P. aeroginosa. • P. aeroginosa is predisposed to by structural lung damage as in bronchiectasis, cystic fibrosis. • S. aureus is predisposed to by: o Viral infection. o IV drug abuse. o Endovascular infection as endocarditis. o Chronic renal failure. • Cavitary lung lesions may denote S. aureus, Klebsiella or tuberculosis.
- 9. • Dental problems and poor oral hygiene predispose to infection with anaerobic organisms. • Exposure to birds predisposes to infection with C. psittaci (psittacosis). • HIV predisposes to: - Pneumocystis jirovecii pneumonia (PJP) (formerly Pneumocystis carinii pneumonia (PCP) - Tuberculosis - P. aeroginosa. - Fungal infection • Asplenia (anatomic or functional) predisposes to invasive infections with encapsulated organisms (pneumococci, meningococci, Klebsiella).
- 10. Clinical Picture Typical Pneumonia • Fever, malaise. • Cough with little (rusty) sputum. • Pleuritic chest pain. • Dyspnoea. Atypical Pneumonia • Elderly: Confusion and subtle changes of mental status dominate the picture. • Viral pneumonia: upper respiratory symptoms as rhinorrhoea, sore throat, dry cough. It occasionally occurs in epidemics or even pandemics (avian flu, swine flu) • Atypical organisms (Mycoplasma, chlamydia): more insidious onset, subtle symptoms (walking pneumonia).
- 11. InvestigationsChest X-Ray • Typical: unilateral lobar or segmental consolidation • Atypical: o Radiographic infiltrates that are not clearly segmental. o Small areas of alveolar consolidation may be missed, esp. in AP portable radiographs (but detected by the far more sensitive CT). o Rapidly progressive pneumonia of any cause may produce diffuse pulmonary infiltrates consistent with ARDS. Culture • Respiratory sample: o Sputum (spontaneous or induced by saline inhalation) o Endotracheal aspiration. o Bronchoalveolar lavage (BAL). Specimens obtained from lower respiratory tract are more predictive of true infection rather than colonization.
- 13. • Blood: Bacteraemia may be documented in: - 10% of patients hospitalized for CAP. - Most patients with haematogenous S. aureus pneumonia. C-Reactive Protein may be a useful indicator of the extent of parenchymal inflammation in pneumonia. It may also be utilized to assess the response to treatment. Lobar Pneumonia, Right Middle Lobe
- 14. C Confusion 1 U BUN > 20 mg/dL 1 R Respiratory Rate > 30 b/min 1 B BP < 90/60 mmHg or need for fluid resuscitation 1 65 Age > 65 y 1 CURB-65 score ranges 0 – 5 CRB-65 score ranges 0 – 4 (BUN excluded). Urea : Urea nitrogen = 60 : 28 (30 : 14) 0 10 20 30 40 50 60 0 1 2 3 4 5 CAP Mortality % In Relation to CURB-65 Score CURB- 65 Score CAP Severity Initial Treatment 0 – 1 Mild Out- patient 2 – 3 Moderate Out- or In- patient 4 - 5 Severe In- patient, possibly ICU CAP Severity Scores
- 15. This means persistence of pulmonary infiltrates > 30 days after initial presentation. • Causes: • Resistant organism. • Missed organism (TB / fungus). • Nosocomial superinfection: another pneumonia, empyema, endocarditis • Non- infectious complications: eg, Bronchiolitis Obliterans Organizing Pneumonia. Non-Resolving or Slowly Resolving Pneumonia Bronchiloitis Obliterans Organizing Pneumonia (BOOP) • Comorbidities: DM, RF, HF • Immunocompromised states Resolution of pneumonia requires resorption of the inflammatory exudate in the alveoli. In BOOP, the inflammatory exudate persists in the alveoli and bronchioles and becomes organized into fibrous tissue which further obliterates the air spaces. X-Ray shows bilateral wide spread patches of fibrosis. Diagnosis is confirmed by CT and bronchoscopic biopsy. Most patients recover with steroid therapy.
- 16. Complications • Empyema: most common infectious complication It should be considered in patients with persistent fever and leucocytosis after 4 – 5 days of appropriate antibiotic treatment. • Extra- Pulmonary Infection eg, arthritis, osteomyelitis, endocarditis. • VTE (Venous Thromboembolism) Risk ↑ at both short and long term but is highest in the 4 weeks following diagnosis. Pneumococcal infection has been specifically associated with host thrombotic tendency stimulated by components of the bacterial cell wall. • BOOP Mortality < 1%: in outpatient treated CAP > 10%: in hospitalized patients 40%: in ICU patients Influenza vaccination ↓ risk of influenza and all cause pneumonia.
- 17. Treatment of CAP - Rest, expectorants, mucolytics, antipyretics. - Good hydration, may entail IV fluids. - Airway clearance techniques (respiratory therapy). - Prophylactic anticoagulation in hospitalized patients. Low molecular weight heparin should be considered in all patients who are not fully mobile. - Oxygen therapy as guided by oximetry. - Duration of treatment: • Outpatient, not complicated: 5 – 7 days. • Hospitalized: initial IV then oral treatment for a total of 7 – 10 days. • Non- Bacteraemic invasive organisms (as Staph. Aureus, Gm –ve bacilli): IV treatment for 10 to 14 days. • Bacteraemic Staph. aureus: 4 weeks of IV therapy because of organism resistance and the possibility of infective endocarditis as a cause or a consequence of pneumonia. • Atypical pneumonia: 2 weeks • PJP: 3 weeks • Fungal pneumonia: several months
- 18. Indications for Hospital Admission • CURB-65 score > 2. • Septic shock with need for vasopressors (ICU required). • Need for mechanical ventilation (ICU required). • Need for non- invasive ventilation. • PaO2 / FiO2 < 250 mmHg (acute lung injury). • Hypothermia < 36 O C. • Comorbidities, eg ESRD, ACS. • Inability to take oral medicines. • No responsible care giver. • Failure of out- patient treatment. Indications for Discharge (Clinical Stability) • Afebrile for > 48 hh. • Haemodynamically stable without vasopressors. • No tachypnoea. • No hypoxaemia (SaO2 > 90% on room air). • Normal mental status. • Normally functioning GIT. (so the patient can be given oral medications)
- 19. Empiric Antibiotic Treatment • Assessment (CURB – 65 score and other parameters) will dictate whether treatment is initiated orally as outpatient, or parenterally as inpatient. • Moderate cases may be started on IV antibiotics to be shortly converted to an oral regimen. Outpatient Treatment Mild Cases Amoxiclav remains the drug of choice: tab 1 gm / 12hh for 5 – 7 days. Alternatives if allergic to penicillin: • Macrolide as Azithromycin tab 500 mg daily for 3 – 5 days • Tetracycline as Doxycycline cap 100 mg / 12 hh for 7 days • Quinolone as Levofloxacin tab 500 mg or Moxifloxacin tab 400 mg once daily. Moderate Cases Amoxiclav + Macrolide Treatment may be initiated parenterally.
- 20. Inpatient Treatment for Severe cases; treatment is started IV: [β-Lactam + Macrolide] Or Quinolone β-Lactam as Amoxiclav 1.2 gm/12h Ampicillin/Sulbactam 1 gm/8h Cefotaxime 1 gm/6h Cetriaxone 1 gm/12h Macrolide as Azithromycin 500 mg/day Quinolone as Levofloxacin 750 mg/day Moxifloxacin 400 mg/day In case of parenteral cephalosporins, oral switch is preferably made to oral amoxiclav rather than oral cephalosporins Respiratory fluoroquinolones are generally effective for empirical therapy of CAP. They are ideal for IV to oral shift (same dose).
- 21. Pseudomonas aeroginosa Anti-Pseudomonal β-Lactam • Piperacillin / Tazobactam 4.5 gm IV /6h • Ceftazidime 1 gm IM/IV /8h • Cefepime 2 gm IV /12h • Imipenem / Cilastatin 1 gm IV /8h • Meropenem 1 gm IV /8h Antibiotics for Specific Pathogens Extended infusion of carbapenems may be preferable Klebsiella & Acinetobacter Carbapenem (Imipenem or Meropenem) If resistant: Colistin (Polymixin E) 2.5 – 5 mg/kg/day IV in 3 divided doses 1 mg Colistin Base = 3000 IU There are various forms of colistin used for inhalation therapy (eg. dry powder for inhalation, solution for nebulization). This minimizes nephrotoxicity from systemic absorption.
- 22. MSSA (Methicillin Sensitive Staph. Aureus) Add anti-Staphylococcal β-Lactam: • Oxacillin 1 gm IV /6h • Fluxacillin 500 mg PO /8h • Cefazolin 0.5 – 1 gm IV /6-8h MRSA (Methicillin Resistant Staph. Aureus) Add vancomycin or linezolid • Vancomycin 15 - 20 mg/Kg IV /8 - 12h, monitored to maintain trough level 15 – 20 mcg/mL • Linezolid 600 mg PO/IV /12h
- 23. Mycoplasma & Chlamydia Doxycyclin cap 100 mg PO/12h Or Macrolide (Azithromycin or Clarithromycin) Treatment for 14 days Legionella Fluoroquinolones for 14 days, starting IV then shifting to oral. PJP (Pneumcystis Jirovecii Pneumonia) Trimethoprim / Sulphamethoxazole 15 mg TMP/Kg/day IV Div /8h or 2 DS tablets (800 mg sulfamethoxazole and 160 mg trimethoprim) PO / 8h for 21 days Fungal Pneumonia (Aspergillosos, Histoplasmosis) Itraconazole 200 mg PO or IV q24h Or Amphotericin B 3 mg/kg q24h if severe Duration of therapy: 1-12 months
- 24. Aspiration Pneumonitis / PneumoniaAspiration Pneumonitis / Pneumonia Aspiration is defined as inhalation of oropharyngeal or gastric contents into the larynx and lower respiratory tract. Aspiration Pneumonitis is a chemical injury caused by aspiration of sterile gastric contents. Aspiration Pneumonia is an infectious process caused by aspiration of oropharyngeal secretions colonized or infected by pathogenic bacteria. However, it is difficult in practice to distinguish between infectious and non- infectious aspiration pneumonia. Aspiration should be initially considered as infectious and treated as such. Pulmonary aspiration is an important cause of serious illness and death among residents of nursing homes and hospitalized patients. However, many aspiration events probably pass unrecognized and are not adequately treated. Aspiration pneumonia is a common cause of death in patients with neurologic dysphagia.
- 25. Predisposing Factors For Occurrence of Aspiration • Diminished gag and cough reflexes due to: anaesthesia, CNS depressants, stroke, dementia, old age, asthenia. Post- extubation is a very vulnerable period. • Poor glottal function. • Seizures. • Choking while vomiting. • Severe GERD. • Mechanical ventilation: One of the most common risk factors for HAP. Ventilation and related interventions (intubation, sedation) ↑ risk of oropharyngeal and gastric aspiration. For the Aspirate to Contain Bacteria Oropharyngeal Aspirate • Upper respiratory infection. • Poor dental hygiene Gastric Aspirate • Hypo/Achlorhydria: as in patients given PPIs or H2 blockers for stress bleeding prophylaxis. Sucralfate (Gastrofait) does not ↑ risk of pneumonia. • Gastroparesis. • Intestinal obstruction.
- 26. Organisms Usually polymicrobial because oropharyngeal secretions contain massive numbers of different organisms (aerobic, anaerobic). Prevention • Dietary Education • Eat only while sitting and fully awake. • Eat slowly, soft food, small bite size. • Swallow slowly and repeatedly. • Good Oral Hygiene • Tube Feeding (NGT or Gastrostomy): may be used in patients with poor cough and gag reflexes. Gastrostomy tube is better than NGT regarding delivery of prescribed nutrition, but it does not prevent gastric aspiration. Aspiration pneumonia is the commonest cause of death in patients fed with gastrostomy tube. Both tubes offer no protection against oropharyngeal aspiration. • Endotracheal Intubation: to protect the airways in patients with low level of consciousness.
- 27. Treatment of Aspiration Pneumonia IV antibiotics are given for 7 – 10 days. If cavitation is present, they may be continued for several weeks. Options include: • Piperacillin / Tazobactam 4.5 gm / 8h. • Ceftazidime 2 gm / 8h. • Ceftriaxone 1 gm / 12h. • Levofloxacin 500 mg / day. Add coverage for anaerobes in case of severe periodontal disease, putrid sputum, evidence for necrotizing pneumonia or lung abscess: • Clindamycin 600 mg / 8h. Or • Metronidazole 500 mg / 8h. NB: Corticosteroids were used for decades, but there is no evidence of benefit.
- 28. Hospital Acquired Pneumonia (HAP)Hospital Acquired Pneumonia (HAP) • If occurs within 4 days of hospital admission, organisms are relatively antibiotic susceptible. Later onset HAP is frequently caused by multi- drug resistant organisms (MDROs) and may be polymicrobial. • Most commonly identified organisms: S. aureus, P. aeroginosa. • High mortality, approaching 30 – 50% due to: o Severity of pneumonia. o Difficulty in providing antibiotic coverage. o Underlying diseases and comorbidities.
- 29. Ventilator Associated Pneumonia (VAP)Ventilator Associated Pneumonia (VAP) • Diagnosis is difficult because of the subjective nature of the variables considered (nature of respiratory secretions and CXR infiltrates) and the presence of many alternative explanations (ARDS, atelectasis, pulmonary embolism, heart failure,…) • Even if organisms are cultured from respiratory secretions, it remains difficult to determine whether they represent true infection or mere colonization. • Mortality rates and health care costs are among the highest among all HAIs and among all HAPs.
- 30. Prevention of VAP • Avoiding mechanical ventilation is the most effective preventive measure. Non- invasive ventilation may be used instead. • Proper sterilization of the ventilator. • Daily assessment of readiness for weaning from ventilator. • Daily “sedation vacation”, if possible. • Elevation of head of bed. • Regular mouth care. • Regular aspiration of subglottic secretions. • Prohibition of unnecessary PPIs and H2 blockers use. • Selective oropharyngeal and/or digestive tract decontamination has been associated with significant reduction in VAP, but may lead to selection of MDROs.
Editor's Notes
- Colonization refers to presence of bacteria at some body site without causing inflammation or tissue destruction, on the contrary to infection which indicates that bacteria are causing some local or systemic harm.
- Identification of influenza virus in a patient with pneumonia should lead to appropriate antiviral treatment, even if &gt; 48 hours passed since the onset of symptoms.
- DM: diabetes mellitus RF: renal failure HF: heart failure
- ESRD: end- stage renal disease ACS: acute coronary syndrome
- Immediately after extubation, there may be still residual effect of anaesthesia and residual laryngeal muscular dysfunction.