aguzzi2010.pdf
- 1. Inappropriate aggregation of proteins is normally prevented by complex cellular quality control mecha- nisms.However, under certain circumstances, an unusual subset of proteins is able to aggregate within or around cells. Although the amino-acid sequences of this class of proteinsarediverse,theyallseemtoadoptasimilar,insol- uble, highly ordered structure when aggregated known as the cross-β spine1 (FIG. 1a). The histology of the resulting protein deposits was appreciated more than 150years ago and was termed amyloid2 (FIG. 1b). Although it is possible to predict the approximate tendency of proteins to form amyloid on the basis of their sequence3 , amyloid forma- tion is far from a simple function of protein sequences and secondary structures. It is becoming increasingly apparent that amyloid-forming proteins exist in a com- plex dynamic equilibrium between soluble monomeric or oligomeric states and various insoluble states of higher- order aggregation. The formation of these aggregates depends on the protein concentration, complex inter- actions with other proteins and the specific cellular envi- ronment. A more thorough understanding of the factors that influence this equilibrium is crucial for determining howproteinaggregationdisordersariseandfordeveloping effective therapies against them. From protein aggregation to pathology Aggregation and accumulation of amyloid-forming proteins can lead to a wide range of protein aggregation diseases known as amyloidoses. These diseases include systemic amyloidoses in which deposits may occur in any part of the body, such as AL amyloidosis due to the accumulation of immunoglobulin light chain amyloid fibrils; amyloid A (AA) or reactive systemic amyloid- osis resulting from deposits of catabolic products of the serum amyloid A protein (SAA); and ATTR duetotrans- thyretin (TTR) accumulation. There are also amyloidoses in which a single organ is affected — possibly including pancreatic accumulation of islet amyloid polypeptide in type 2 diabetes4 . Many protein aggregation diseases affect the nervous system. Interestingly, certain proteins specifically aggre- gate and are toxic in the central nervous system (CNS) despite the fact that they are ubiquitously expressed. These neurodegenerative diseases include disorders in which the pathological proteins may accumulate within the nucleus, as is the case with polyglutamine expansion diseases(suchasHuntington’sdiseaseandspinocerebellar ataxias), disorders characterized by cytoplasmic inclu- sions (such as α-synuclein in Parkinson’s disease), as well as disorders in which pathological proteins accumulate extracellularly (for example in prion diseases) or both intracellularly and extracellularly (for example, tau and amyloid-β (Aβ) in Alzheimer’s disease). It is becoming clear that amyloid formation is not always pathological, but rather might have a nor- mal physiological function5 . However, not all patho- logical protein aggregates necessarily form amyloids. Nevertheless, the definition of amyloid is broadening Institute of Neuropathology, University Hospital of Zürich, Schmelzbergstrasse 12, CH‑8091 Zürich, Switzerland. Correspondence to A.A. e‑mail: adriano.aguzzi@usz.ch doi:10.1038/nrd3050 Protein aggregation diseases: pathogenicity and therapeutic perspectives Adriano Aguzzi and Tracy O’Connor Abstract | A growing number of diseases seem to be associated with inappropriate deposition of protein aggregates. Some of these diseases — such as Alzheimer’s disease and systemic amyloidoses — have been recognized for a long time. However, it is now clear that ordered aggregation of pathogenic proteins does not only occur in the extracellular space, but in the cytoplasm and nucleus as well, indicating that many other diseases may also qualify as amyloidoses. The common structural and pathogenic features of these diverse protein aggregation diseases is only now being fully understood, and may provide novel opportunities for overarching therapeutic approaches such as depleting the monomeric precursor protein, inhibiting aggregation, enhancing aggregate clearance or blocking common aggregation-induced cellular toxicity pathways. REVIEWS NATuRe RevIewS | Drug Discovery voLuMe 9 | MARCH 2010 | 237 © 20 Macmillan Publishers Limited. All rights reserved 10
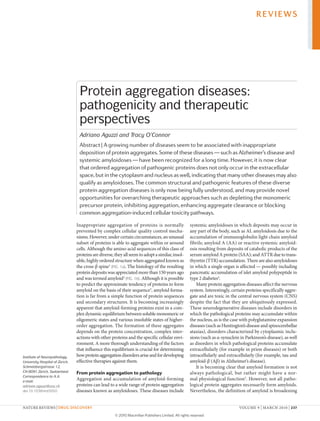
- 2. Nature Reviews | Drug Discovery a b 100 µm β1 β1 Odd end L17 V40 K28 D23 Odd end Fibril axis β2 β2 to encompass a wider range of diseases6 . originally, the term was used exclusively to describe extracellu- lar amyloid deposits that stain with histological dyes such as Congo red. Now, it is recognized that many cytoplasmic7 and even intranuclear inclusions8 , which do not necessarily stain with these dyes, are composed of ordered fibrillar structures similar to those of clas- sical amyloids. Furthermore, some of these dyes seem to bind to aggregated intermediates of amyloid-forming proteins in addition to mature amyloid fibrils (for exam- ple, thioflavin appears to bind to Aβ oligomers)9–11 . Interestingly, staining with Congo red and thioflavin S has been reported intracellularly in some cases12,13 . Thus, the current classification of amyloids is far from clearly defined. In this Review, we summarize various therapeutic approaches aimed at preventing or reversing patho- logical protein aggregation (TABLE 1). our discussion is focused around two neurodegenerative diseases: prion disease and Alzheimer’s disease. However, a number of extracerebral amyloidoses are also benefiting from therapeutic advances. Several systemic amyloidoses are becoming manageable chronic diseases rather than definite death sentences. Alzheimer’s disease Alzheimer’s disease, the most common neurodegenera- tive disorder, is currently the focus of some of the most exciting and rapidly progressing research on amyloid therapeutics. Alzheimer’s disease pathology is character- ized by the formation of two types of protein aggregates in the brain: amyloid plaques (FIG. 2a) — which form an extracellular lesion composed of the Aβ peptide; and intracellular neurofibrillary tangles (FIG. 2b) — which are composed of hyperphosphorylated filaments of the microtubule-associated protein tau. Genetic evidence implicates deregulated Aβ homeostasis as an early event in Alzheimer’s disease pathology14 . Indeed as all familial Alzheimer’s disease mutations lead to increased produc- tion of this peptide or preferential production of a more fibrillogenic Aβ isoform (Aβ42)15 . For this reason, most Alzheimer’s disease therapeutics have targeted the Aβ peptide, although tau-targeted therapies are also being pursued16,17 . Targeting Aβ production: the secretase inhibitors. one widely pursued method of combating protein aggrega- tion diseases is to inhibit the production of the mono- meric form of the protein with the aim of reducing the amount of protein available to aggregate. In the case of Alzheimer’s disease, the amyloidogenic Aβ frag- ment associated with amyloid plaques is derived from proteolytic processing of a longer, non-aggregating precursor protein — amyloid precursor protein (APP) (FIG. 3). Therefore, pharmacological inhibition of the enzymes responsible for Aβ formation (γ-secretase and β-secretase) is a prime strategy for blocking Aβ produc- tion. The γ-secretase complex consists of four proteins18 , the catalytic activity of which is thought to be mediated by the presenilin 1 (PS1) and PS2 proteins. The func- tional assembly of these proteins has the unusual ability to target a stretch of APP that is entirely buried within Figure 1 | common features of protein aggregation and amyloids. a | Ribbon diagrams of the three-dimensional structure of amyloid-β (Aβ42) (residues 17–40). Amyloid-forming proteins such as Aβ are all thought to form similar tertiary structures when aggregated, known as a cross-β spine or amyloid162 . The cross-β spine consists of an ordered arrangement of β-sheets (thick coloured arrows). b | Congo red-stained sections of human kidney affected by amyloidosis. The cross-β spine structure is able to intercalate with molecules of the azo-dye Congo red and cause them to emit a characteristic apple-green birefringence upon exposure to polarized light163 . This unique feature of amyloids has historically been used to identify them histologically. REVIEWS 238 | MARCH 2010 | voLuMe 9 www.nature.com/reviews/drugdisc © 20 Macmillan Publishers Limited. All rights reserved 10
- 3. Blood–brain barrier A protective wall of capillary epithelium separating the brain parenchyma from the bloodstream that is impenetrable to most circulating substances. the lipid bilayer of the plasma membrane. The γ-secretase complex is responsible for the carboxy-terminal cleavage of APP to produce Aβ40 or Aβ42. Potent small-molecule inhibitors of γ-secretase can dramatically reduce Aβ40 and Aβ42 production19–22 . The primary caveat to targeting γ-secretase for Alzheimer’s disease therapeutics is that APP is not the only substrate of γ-secretase. The most notable alternative cleavage substrate is the Notch receptor23,24 . Cleavage of Notch by γ-secretase is crucial for normal development, as shown by the fact that Ps1–/– mice suffer from embryonic lethality owing to deficient Notch cleavage25,26 . Although this does not necessarily disqualify γ-secretase as a drug target, Notch seems to mediate differentiation of sev- eral cell types throughout adulthood (for example, gut epithelium and T cells). The unfortunate consequence of this is that potent γ-secretase inhibitors have serious gastrointestinal and immunological side effects27 . As a result of this drawback, the field has shifted towards the development of γ-secretase modulators. These compounds either selectively inhibit γ-secretase cleavage of APP, leaving Notch cleavage unaffected, or alter γ-secretase cleavage of APP to favour Aβ40 pro- duction rather than Aβ42. The longer, less abundant 42 amino-acid isoform of Aβ, Aβ42, seems to be more closely associated with the development of amyloid pathology than its counterpart, Aβ40. Studies have shown that dominantly-inherited PS1 mutations, which cause Alzheimer’s disease with 100% penetrance, lead to a shift in γ-secretase cleavage of APP in favour of the Aβ42 isoform28–33 . Drugs that modulate γ-secretase activity in this manner include non-steroidal anti-inflammatory drugs (NSAIDs) such as ibuprofen34 and compounds that interact with the ATP-binding motif of PS1 near the γ-secretase active site35 . one such γ-secretase-modulating compound, the NSAID (R)-flurbiprofen (also known as tarenflurbil), effectively reduced amyloid plaque formation36 and res- cued memory deficits37 in APP-transgenic mice. It also yielded encouraging results in early human trials38,39 . However, (R)-flurbiprofen failed to significantly enhance cognitive performance of patients with Alzheimer’s disease in Phase III clinical trials and has recently been abandoned as a potential therapy40 . The compound- screening approach may identify additional promising small-molecule γ-secretase modulators, and other com- pounds may be more successful than (R)-flurbiprofen in human trials (for example, semagacestat from Lilly and elan is currently in Phase III trials41 ), researchers may also decide to capitalize on recent results demonstrating the existence of endogenous γ-secretase activity modi- fiers that are APP-specific42 and the observation that some components of the γ-secretase complex have tissue- specific isoforms, which may provide a novel means of achieving brain-specific γ-secretase inhibition43 . The amino-terminal cleavage of APP to form both Aβ40 and Aβ42 results from β-secretase activity. After the discovery that β-secretase cleavage of APP seemed to be due to the activity of a single aspartic protease, β-secretase 1 (BACe1; also known as memapsin 2 and ASP2), there was much interest in the possibility of targeting β-secretase for the treatment of Alzheimer’s disease44–48 . Deletion of this enzyme does not have an overt effect on phenotype in mice, suggesting that BACe1 inhibitors, unlike γ-secretase inhibitors, might lack serious target-related side effects49 . Inhibition of BACe1 activity can block the production of Aβ, prevent the development of amyloid pathology in the brain and rescue Alzheimer’s disease-related memory deficits in mice50–53 . However, nearly a decade has passed since the initial identification of BACe1 as the β-secretase, and researchers continue to struggle with the development of effective BACe1 inhibitors that are active in the CNS. The large BACe1 active site requires the identification of large compounds for potent BACe1 inhibition that also readily penetrate the blood–brain barrier (BBB)54 and are reasonably stable. unfortunately, the slow progress of the BACe1 inhibitor field is a testament to the fact that such molecules are relatively rare. Furthermore, it is becoming increasingly apparent that BACe1 has alternative cleavage substrates and may have Table 1 | Summary of therapeutic strategies for protein aggregation diseases Approach Therapy expected effect current status refs Inhibition of amyloidformation γ-Secretase inhibitors and modulators Reduced carboxy-terminal cleavage of APP to form Aβ40 or Aβ42 Phase II and III clinical trials 39 β-Secretase inhibitors Reduced amino-terminal cleavage of APP to form Aβ40 and Aβ42 Phase I clinical trials 63 Promotion of amyloid clearance Aβ immunotherapy Enhanced clearance of Aβ-containing aggregates Phase II and III clinical trials 17,82,83 Prion immunotherapy Enhanced clearance of PrPSc -containing aggregates; prevention of the invasion of prions into neurons Preclinical 117,118, 120–127 Inhibition of amyloid aggregation Scyllo-inositol Prevention of the formation of higher-order aggregates Phase II clinical trials 168 Tafamidis Stabilization of the native state of transthyretin Phase II and III clinical trials 145 Aβ, amyloid-β; APP, amyloid precursor protein; PrPSc , prion protein with abnormal conformation. REVIEWS NATuRe RevIewS | Drug Discovery voLuMe 9 | MARCH 2010 | 239 © 20 Macmillan Publishers Limited. All rights reserved 10
- 4. Nature Reviews | Drug Discovery a b 200 µm 200 µm Passive transfer A process by which a host acquires exogenous antibodies and hence immunity to an immunogen without generating an active immune response. subtle physiological roles in humans (for example, in peripheral nerve myelination and synaptic transmis- sion)55–64 . Nevertheless, some BACe1 inhibitors have progressed to early clinical trials65 . As with γ-secretase inhibition, problems with developing small-molecule BACe1 inhibitiors may ultimately be circumvented by indirect approaches to BACe1 inhibition — for example, by modulating regulatory mechanisms that control BACe1 expression66–72 or by taking advantage of the fact that BACe1 activity is optimal in acidic cellular compartments73 . Despite the various drawbacks to the approach of secretase inhibition, γ-secretase inhibi- tors, γ-secretase modulators and β-secretase inhibitors continue to be actively pursued as drug targets for Alzheimer’s disease therapy in the hope that the eventual benefits might outweigh the risks. Mobilizing the immune system: Aβ immunotherapy. An alternative approach to protein aggregation therapeutics is to enhance the degradation of the aggregating protein or the aggregates themselves. Manipulating the immune system for the purpose of enhancing Aβ clearance has been pursued as a therapeutic approach for Alzheimer’s disease since the turn of the millennium. This was when several studies reported dramatically reduced Aβ levels and plaque pathology and/or cognitive improvements upon active immunization of APP-transgenic mice with full-length Aβ peptide74–76 , Aβ peptide fragments77 and passive transfer of Aβ-specific antibodies78–81 . Based on these studies and encouraging results from Phase I trials, active Aβ immunotherapy in humans subsequently progressed to a widely publicized Phase II clinical trial in 2001. unfortunately, this trial was halted in January 2002 owing to the development of sterile meningoen- cephalitis in some patients82 . Nonetheless, a follow-up study on a small subset of patients from the Phase II immunotherapy trial sug- gested that individuals that had generated high Aβ anti- body titres exhibited a decreased rate of cognitive decline compared with placebo-treated individuals83 . However, theseresultsarecontroversialandfollow-upanalyseshave questioned the validity of this positive interpretation. As a complementary strategy, second-generation Aβ immunotherapies are attempting passive transfer approaches. A monoclonal Aβ antibody from Pfizer is currently in Phase II clinical trials. Additionally, bapineuzumab from elan–wyeth caused a significant delay in cognitive decline, at least in a subset of indi- viduals17 . Therefore, the outlook on Aβ immunotherapy remains hopeful. Interestingly, preliminary studies have shown that intravenous treatment with human immunoglobu- lins, an approved treatment for immune deficiencies and autoimmune disorders, also seems to be effective in reducing Aβ levels and cognitive decline in patients with Alzheimer’s disease84,85 . Although the mechanism of action remains unclear, these studies raise the interest- ing question of whether immunotherapy for Alzheimer’s disease needs to be directed against the Aβ peptide, or whether general immunomodulation (possibly through Fcγ-mediated engulfment of amyloid deposits by micro- glia, or through poorly understood modulation of cere- bral cytokine signalling)86 might be sufficient to enhance the clearance and degradation of pathological peptides in the brain. If so, this finding would have important implications for the treatment of other protein aggrega- tion diseases. Figure 2 | characteristics of Alzheimer’s disease. a | A human cortical section from a patient affected by Alzheimer’s disease, stained with an amyloid-β (Aβ)-specific antibody. One of the classical hallmarks of Alzheimer’s disease histopathology is the appearance of extracellular lesions known as senile or amyloid plaques, which are primarily composed of the Aβ peptide. b | A human cortical section from a patient affected by Alzheimer’s disease, stained with a phospho-tau-specific antibody. The second histopathological hallmark of Alzheimer’s disease is the presence of intraneuronal lesions known as neurofibrillary tangles (indicated by an arrow), which are composed of abnormal, hyperphosphorylated filaments of the microtubule- associated protein tau. REVIEWS 240 | MARCH 2010 | voLuMe 9 www.nature.com/reviews/drugdisc © 20 Macmillan Publishers Limited. All rights reserved 10
- 5. Nature Reviews | Drug Discovery b Non-amyloidogenic a Amyloidogenic γ γ α β Endosome Cytoplasm Nucleus Endosome APP APP APP APPsα C83 AICD p3 APPsβ C99 Aβ42 Aβ40 Curiously, despite the initial success of Aβ immuno- therapeutic methods, the mechanisms by which these antibodies function to clear amyloid and/or to elicit cog- nitive improvement remains an area of intensive debate. Three scenarios have been envisaged87 . First, immuno- therapy might enhance microglial phagocytic activity, which could be directed against the soluble monomeric and/or oligomeric forms of the amyloid-forming protein. This would reduce the amount of protein that is avail- able to aggregate. Alternatively, microglia might directly disassemble the insoluble deposits, as microscopic analy- sis suggests that Aβ antibody administration promotes microglial uptake of insoluble deposits78 . However, the stability of deposits in the brain argues against this hypothesis81,88 . Second, the ‘peripheral sink hypoth- esis’ postulates that antibodies mediate their effects by sequestering amyloid-forming proteins in the periphery (based on the theory that peripheral plasma proteins are in equilibrium with CNS amyloid-forming proteins )79,80 . In this scenario, antibodies may bind to amyloid-forming proteins and act as a physical barrier, preventing amyloid- formingproteinfromcrossingtheBBB,orantibodiesmay stimulate immune-mediated uptake of amyloid-forming proteins. In either case, the proposed net result is efflux of protein out of the CNS into the periphery, where the pro- tein is presumably degraded by circulating macrophages. Third, antibodies might inhibit the aggregation process by preventing the recruitment of monomeric species to aggregated moieties, either by binding to the monomers or the aggregates themselves. evidence that Aβ antibod- ies, which bind amyloid plaques, are the same antibodies that effectively ameliorate plaque pathology78 supports this hypothesis89 . Regardlessoftheexactimmunotherapeuticmechanism ofaction,thenetresultislikelytobeenhancedclearanceof amyloid-forming proteins, as non-aggregated and aggre- gated states are in equilibrium and soluble forms of the protein are more accessible to clearance and degrada- tion mechanisms than insoluble forms. Several of these mechanisms probably act simultaneously, with the rela- tive contribution of each to net reduction in aggregation depending upon the specific properties of the amyloid- forming protein being targeted, the stage of disease pro- gression and the antibody being used. All aggregates are not created equal: toxic oligomers and neurodegeneration. An important assumption underlying therapeutic strategies aimed at reducing protein aggregation is that protein aggregates are toxic to cells. But is this the case? It has long been known that the number of amyloid plaques in Alzheimer’s diseased brains correlates poorly with the degree of dementia90 . Figure 3 | Amyloid-β formation. Amyloid precursor protein (APP) undergoes a series of proteolytic cleavages in neurons to form the amyloid-β (Aβ) peptide that is associated with senile plaques in Alzheimer’s disease. In the amyloidogenic pathway (a), internalized APP is initially cleaved at its amino terminus by endocytic β-secretase (β) to form secreted APPsβ and C99. C99 then becomes a substrate for intramembraneous cleavage by the γ-secretase complex, leading to the release of Aβ40 (or Aβ42 at low frequency) and the APP intracellular domain (AICD), which may regulate gene expression. In a competing, non-amyloidogenic pathway (b), α-secretase cleaves cell surface APP to liberate secreted APPsα and C83. C83 is then cleaved by γ-secretase to form the soluble p3 peptide and the AICD. The majority of Aβ and N-terminal APP cleavage fragments are eliminated from the neuron by the secretory pathway. REVIEWS NATuRe RevIewS | Drug Discovery voLuMe 9 | MARCH 2010 | 241 © 20 Macmillan Publishers Limited. All rights reserved 10
- 6. Long-term depression An enduring weakening of synaptic strength that is thought to interact with long-term potentiation (LTP) in the cellular mechanisms of learning and memory. Unlike LTP, which is produced by brief high-frequency stimulation, LTD can be produced by long-term, low-frequency stimulation. More refined measurements that take into account levels of total Aβ aggregates (or amyloid load, of which plaques are only a subset) seem to be better predictors of cog- nitive performance. one theory that has emerged to explain this observation is that the large, insoluble lesions observed upon histological examination are benign ‘tombstones’ and that the pathological media- tors are highly toxic oligomeric intermediates, which exist in a kinetic state that is between the monomeric and the insoluble, aggregated state. oligomers derived from cultured cells consist primarily of Aβ dimers and trimers91,92 , whereas oligomers isolated from brain tissue consist of a mixture of dimers, trimers and higher-order aggregates93,94 . Interestingly, a reduction in higher-order Aβ aggregates (and not Aβ trimers) was co-incident with cognitive improvement in APP-transgenic mice receiv- ing scyllo-inositol (eLND005) treatment95 . A large body of evidence has accumulated over the past decade estab- lishing a role for Aβ oligomers in synaptic dysfunction and neurotoxicity (reviewed in REFS 96,97). In addition, more recent studies have further implicated this Aβ spe- cies in other aspects of Alzheimer’s disease pathogenesis, including tau phosphorylation98 , long-term depression 99 , retrograde trafficking of brain-derived neurotrophic fac- tor100 and insulin signalling101,102 . with regards to thera- peutics, it is hoped that traditional approaches will clear oligomeric species with as much (or more) efficacy as they clear mature amyloid fibrils. However, the theory of toxic oligomers has other interesting implications for therapeutics. For example, it implies that therapies do not have to clear protein aggre- gates to be beneficial. Indeed, studies in APP-transgenic mice indicate that certain Aβ immunotherapies lead to cognitive improvement without any detectable clearance of Aβ81 . In the future, conformation-specific antibodies that recognize and neutralize the action of these toxic species in addition to promoting Aβ clearance could be the most effective type of antibodies in eliciting cognitive improvement in Alzheimer’s disease. Interestingly, some of these antibodies recognize a common motif in diverse protein aggregates103 , and so could be broadly useful for the treatment of many aggregation disorders. Inside or out? The role of intracellular Aβ in amyloid pathology. As with any new discovery, the idea of toxic oligomershasultimatelyraisedasmanyquestionsasithas answered. For example, how and where do Aβ oligomers induce neurotoxicity? Amyloid plaques seem to be extra- cellular lesions; however, if soluble oligomers are the pri- mary toxic species, they could mediate their toxic effects inside the neuron. Although the majority of Aβ is elimi- nated from the cell through the secretory pathway (FIG. 3), supporting the idea that Aβ exerts its effects extracellu- larly,thereismountingevidencethatintracellularpoolsof Aβ could also have an important role in the disease proc- ess. The disease-associated isoform of Aβ, Aβ42, seems to be more prone to intracellular accumulation than Aβ40. Also, intracellular Aβ occurs most frequently in the hip- pocampus and entorhinal cortex (eRC), which are the brain regions to be affected first in Alzheimer’s disease104 . expression of the ε4 allele of apolipoprotein e (APoe4), a major genetic risk factor for Alzheimer’s disease, also increases intracellular Aβ105 . More recent studies have found that increased synaptic activity reduces intracellu- lar Aβ106 , and overexpression of neprilysin, which signifi- cantly ameliorates plaque pathology in APP-transgenic mice,alsodecreasesintracellularAβ107 .Therapiesaimedat reducing intracellular Aβ levels therefore warrant further investigation. The ability of current methods to influence intracellular Aβ levels might be indicative of their efficacy. Indeed, Aβ immunotherapy can reduce intracellular Aβ in addition to its other effects, even when the antibody is not internalized108 . Interestingly, Aβ immunotherapy has recently been used to reduce intracellular Aβ and attenuate motor impairment in a mouse model of inclu- sion body myositis — a disease in which intracellular Aβ accumulation is a prominent feature109 . The idea that soluble oligomeric intermediates and intraneuronal pools of Aβ have key roles in pathogenesis issteadilygainingsupport,indicatingthattraditionalideas about amyloid are rapidly evolving. Nevertheless, the idea that amyloid deposits are entirely non-pathological seems unlikely. In the case of Alzheimer’s disease, it is well established that neurons surrounding neuritic plaques have an abnormal appearance. It is likely that many forms of Aβ can contribute to neuronal dysfunction, as proposed by one recent study investigating neuronal Arc expression in the vicinity of extracellular and intracell- ular pools of Aβ110 . The extent to which each Aβ pool contributes to the disease process at different stages will undoubtedly be the subject of future studies. Infectious amyloid: the prion diseases Prion diseases, also known as transmissible spongiform encephalopathies, include Creutzfeldt–Jakob disease, kuru, fatal familial insomnia and Gerstmann–Sträussler– Scheinker syndrome in humans; scrapie in sheep; bovine spongiformencephalopathyincattle;andchronicwasting disease in cervids111 . The prion protein (PrP) is normally present in its native conformation (PrPC ). However, in all prion diseases, the protein is present in an abnormal conformation (PrPSc ) that accumulates and forms depos- its around neurons (FIG. 4a,b). A unique feature of prion diseases is that they are transmissible among humans and across species. Although a seeding mechanism with subsequent propagation of amyloid fibrils is thought to occur generally in amyloidoses, prion diseases seem to be theonlyamyloidosesthataregenuinelyinfectiousdiseases (with the possible exception of AA amyloidosis)112,164 . Remarkably, the infectious agent in all prion diseases appears to be composed exclusively of PrPSc aggregates, although the conversion process from PrPC to PrPSc may require other cellular cofactors. upon association with the PrPSc conformer, PrPC undergoes a dramatic shift in secondary structure from a protein composed of ~45% α-helices and relatively few β-sheets to a protein composed of ~30% α-helices and ~45% β-sheets. PrPSc aggregates are unusually resistant to degradation, and proteinase K digestion (which entirely degrades PrPC , but only partially degrades PrPSc ) is the most common biochemical method of distinguishing PrPC from PrPSc in tissues and cells (FIG. 4c,d). The unusual properties of REVIEWS 242 | MARCH 2010 | voLuMe 9 www.nature.com/reviews/drugdisc © 20 Macmillan Publishers Limited. All rights reserved 10
- 7. Nature Reviews | Drug Discovery a b c d C57BL/6 Prnp–/– PK + + MW (kDa) 25 20 15 PrPSc PrPC Histoblot (PrP Sc ) prion amyloid propagation have presented considerable challenges for the development of effective therapeutics to treat prion diseases, as well as opportunities to explore unique therapeutic modalities. The immune system revisited: prion immunotherapy. The immune system has a complex role in the course of many amyloidoses, and prion diseases are no exception. The peripheral immune system is crucial for extraneu- ral prion replication and the spread of prions to the CNS. Mice that lack various components of the immune system — for example, B cells and follicular dendritic cells (FDCs) — are much less susceptible to prion dis- ease upon peripheral infection113–116 . Conversely, pro- inflammatory conditions increase susceptibility to prion infection117,118 , promote peripheral prion deposition119,120 and accelerate prion pathogenesis113–115,121 . However, the role of the immune system in prion replication in the CNS is less clear. Although extensive astrogliosis is a hallmark of prion diseases, transgenic mice in which various components of inflammatory pathways had been deleted were not more susceptible to prion infection when inoculated intracerebrally, indicat- ing that many key immune pathways do not contribute to prion replication in the CNS. However, depletion of microglia led to a nearly 15-fold increase in prion infec- tivity in a slice culture model of prion disease122 . This suggests that immune-mediated phagocytic activity in the CNS might be involved in degrading prion aggre- gates and prolonging neuronal survival. In either case, as with Alzheimer’s disease, targeting the immune system (both peripherally and in the CNS) has become a prime therapeutic strategy against prion disease pathogenesis. Targeting peripheral immune cells. unlike other neuro- degenerative diseases, prion diseases can spread from the periphery to the CNS (and possibly vice versa). The immune system has a pivotal role in this process. FDCs in secondary lymphoid organs accumulate PrPSc in both acquired and inherited forms of the disease. In the case of most acquired prion diseases, it is from these sites that PrPSc is subsequently transmitted to the CNS123 . Consequently, targeting FDCs has proved to be an effec- tive method of preventing the spread of PrPSc from the periphery to the CNS in animal models. For example, lymphotoxin-β receptor (LTβR) signalling is required for FDC maintenance and might even be directly involved in enabling prion replication at the cellular level116,124–126 . Blocking peripheral LTβR signalling in mice by adminis- teringsolubleLTβR–immunoglobulinfusionproteintran- siently depletes FDCs and prevents PrPSc accumulation in peripheral lymphoid organs (for example, the spleen) and subsequent transmission of PrPSc to the CNS124,165 . The drawback to this approach is that it requires the time of peripheral prion infection to be known, which is not pos- sible in many cases of acquired prion disease. However, this approach may prove useful to medical personnel for cases of accidental prion infection in the clinic. From Aβ to PrP: PrP immunization. The initial success of Aβ immunotherapy for the treatment of Aβ pathology in APP-transgenic mice inevitably led to the investigation of whether the immune system could also be mobilized to clear PrPSc aggregates. Both active and passive PrP immunotherapy have been tested for efficacy in the treat- ment of prion disease. These approaches have revealed additional challenges facing the immunotherapeutic approach to amyloid diseases. In the case of active PrP immunization, the immune systems of wild-type mice were largely tolerant to PrP as it is ubiquitously expressed. The result was the generation of low PrP-specific anti- body titres and minimal or non-significant increases in survival time when used to treat intraperitoneal prion inoculation127–131 . Transgenic expression in mice of a PrP epitope raised in Prnp–/– mice prevented disease following intraperitoneal prion inoculation and showed that PrP immunotherapy is theoretically an effective strategy for combating prion infection132 . Despite these encouraging results, subsequent attempts of passive PrP immuniza- tion have required unrealistically high levels of PrP anti- bodies to elicit any meaningful effect on the survival of Figure 4 | characteristics of prion disease. a | A human cortical section from a patient affected by prion disease, stained with prion protein (PrP)-specific antibodies. All prion diseases are marked by this widespread accumulation of insoluble deposits in the brain consisting of the human prion protein (PrPC ) folded in an abnormal conformation (PrPSc ). b | A haematoxylin- and eosin-stained human cortical section from a patient affected by prion disease. As seen here, another pathological hallmark of prion diseases is the formation of large vacuoles, or ‘spongiosis’, in the affected brain tissue. It is because of this lesion that prion diseases are also known as transmissible spongiform encephalopathies. c | Proteolytic degradation followed by PrPSc -specific immunostaining (PrPSc histoblot) of coronal mouse brain sections from C57BL/6 (prion-susceptible) and Prnp–/– (prion-resistant) mice infected with a mouse-adapted prion strain, Rocky Mountain Laboratory passage 5 (RML5). d | A PrP-specific immunoblot of brain homogenates digested by proteinase K (PK) and separated by SDS–PAGE, taken from RML5-infected C57BL/6 (PrPSc ) or uninfected (PrPC ) mice. PrPSc and PrPC have identical amino-acid sequences and are thought to differ only in secondary structure. Although the crystal structure of PrPSc has not been solved, its conformation can be distinguished from that of PrPC using biochemical techniques. For example, PrPSc is partially resistant to protease digestion, whereas PrPC is fully sensitive to proteolytic degradation. MW, molecular weight. Panel c is reproduced, with permission, from REF. 163 © (2007) Elsevier Science. REVIEWS NATuRe RevIewS | Drug Discovery voLuMe 9 | MARCH 2010 | 243 © 20 Macmillan Publishers Limited. All rights reserved 10
- 8. mice following intraperitoneal inoculation with prions. Furthermore, passive immunization has so far been ineffective in slowing the rate of disease progression in mice following intracerebral prion inoculation or in mice showing clinical signs of disease133 . Another potential problem with the PrP immuno- therapy approach was highlighted by the observation that certain PrP-specific antibodies are capable of trig- gering a pro-apoptotic signalling cascade in neurons that is reminiscent of PrPSc infection or deletion of the central domain of PrPC (REF. 134). Fortunately, not all PrP-specific antibodies seem to have this capability. Nevertheless, this study urges caution to those inves- tigating PrP immunotherapeutics. In its current state, PrP immunotherapy is still far from entering the clinic. However, new innovations, such as antibodies that are able to penetrate the BBB more readily or PrP–antibody fusion proteins designed to specifically target the immune system to PrPSc deposits, may dramatically increase the efficacy of PrP immunotherapy. Preventing amyloid formation: aggregation inhibitors. In recentyears,therehasbeentremendousprogressindevel- opingtherapeuticstrategiesaimedatreducingtheproduc- tion or enhancing the degradation of amyloid-forming proteins. However, in the case of prion diseases, in which the amyloid-forming protein is not produced from enzy- maticactivityandthepathologicalaggregatesareunusually resistant to degradation, it is likely that alternative strate- gies will have to be pursued. one viable approach might be to physically interfere with the aggregation process. As the process of aggregation itself is not entirely under- stood, this is a difficult approach at present. Nonetheless, numerous compounds, peptides and nucleic acids have been investigated for their ability to prevent PrPSc aggre- gation and slow the progression of prion disease. These types of compounds and their efficacy in different model systems have been extensively reviewed elsewhere135 . The exact mechanism of action of this type of therapy is not known; however, it is thought that the three-dimensional structure of this class of molecules might enable them to intercalate within growing amyloid structures, preventing further recruitment of monomers and promoting the dis- solutionofaggregates.Alternatively,thesecompoundsmay mimic the amyloid-binding properties of and/or compete with endogenous amyloid-stabilizing proteins. Certain endogenous proteins (and metal ions) associate with and promotethestabilityofamyloid in vivo,includingheparin sulphateproteoglycans,APoe,APoJ(alsoknownasclus- terin), α1-antichymotrypsin, complement factors, serum amyloid P (SAP), copper and zinc. A potential concern with this class of compounds is that mimicking the properties of amyloid-stabilizing proteins could also promote aggregation of amyloid- forming proteins. This may partially explain the conflict- ing results on the efficacy of these compounds on PrPSc aggregationacrossstudiesandindifferentmodelsystems. An interesting alternative approach may be to deplete endogenous levels of amyloid-stabilizing proteins. For example, successful depletion of SAP from serum and cerebrospinal fluid of patients with Alzheimer’s disease has been achieved using subcutaneous injections of the compound CPHPC (R-1-[6-[R-2-carboxy-pyrrolidin- 1-yl]-6-oxo-hexanoyl] pyrrolidine-2-carboxylic acid), which binds SAP and targets this peptide for hepatic degradation136 . Another class of drugs that may prevent the aggrega- tion of PrPSc are the antimalarial compounds quinacrine and chloroquine137–139 . These drugs localize to lysosomes, the cellular compartment in which PrPSc accumulates, and presumably interfere with the interaction of PrPC with PrPSc and the formation of PrPSc aggregates. However, antimalarial compounds also interfere with lysosomal function. As lysosomes might be involved in degrading endogenous PrPC , these drugs have the poten- tial to prolong PrPC half-life, thereby promoting PrPC – PrPSc interaction and the conversion of PrPC to PrPSc . This might explain why some studies have reported an accelerated disease course and enhanced PrPSc depo- sition following administration of antimalarial com- pounds140,141 . Despite these conflicting data about the efficacy of antimalarial drugs in preventing PrP aggre- gation, quinacrine was recently tested in a clinical trial of patients with Creutzfeldt–Jakob disease. The drug was reasonably well tolerated, but it did not have a significant effect on the course of prion disease142 . A viable alternative strategy could be to develop agents thatcompetewithendogenousamyloid-stabilizingproteins using a compound or peptide that cannot be incorporated into aggregates and has no known amyloid-stabilizing properties. The effectiveness of this approach has been demonstrated by transgenic overexpression of a soluble form of PrP (PrP-Fc), which significantly delayed incu- bation time following prion inoculation132 . A similar mechanismmightunderlietheactionofseveralotheranti- aggregationcompounds.Forexample,proteinXmimetics of PrP are compounds designed to interact with and block PrP amino acids that are thought to comprise the binding site of an unknown endogenous protein required for the conversion of PrPC to PrPSc (REFS 143,144). Compounds known as β-sheet breakers contain sequences from tar- get amyloid-forming proteins plus additional proline residues designed to interfere with amyloid formation145 . Similar compounds have been developed to interfere with the interaction of Aβ and APoe or Aβ and SAP146–148 . Additionally, the ability of Congo red to interfere with amyloid formation in some studies raises the intriguing possibilitythatcommonlyusedamyloiddiagnosticorbio- chemical tools may also have therapeutic applications. An example of one such tool is luminescent conjugated poly- mers (LCPs), which bind amyloids in a manner similar to Congo red or thioflavin but are sterically more flexible thanthesecompounds,perhapsmakingthemlesslikelyto stabilize amyloid conformations149,166 . Interestingly, com- pounds that block amyloid aggregation may ultimately reach the clinic for the treatment of systemic amyloidoses (which do not have the additional requirement for com- pounds to cross the BBB) long before neurodegenerative disorders. For example, two such compounds for the treatmentofATTRamyloidosis(tafamidisfromFoldRx150 andscyllo-inositolfromelan)arecurrentlyinPhaseIIand III clinical trials. REVIEWS 244 | MARCH 2010 | voLuMe 9 www.nature.com/reviews/drugdisc © 20 Macmillan Publishers Limited. All rights reserved 10
- 9. Nature Reviews | Drug Discovery a Physiological levels of oligomers b Pathological levels of oligomers Cytoplasm Lysosome Lysosomal enzymes Toxic oligomer PrPc Conformationally altered PrP Lipid raft Long-term potentiation A persistent increase in synaptic response following repeated stimulation of a neuron, which is thought to be associated with synaptic plasticity and the acquisition of memories. The prion protein as an aggregate receptor: the normal function of PrPC revealed? Another fascinating impli- cation of the toxic-oligomer theory is that specific cell surface receptors could trigger neuronal dysfunction and/or neuronal apoptotic pathways following binding of oligomeric species. This concept is not new to the prion field: it has long been known that PrPSc -mediated neuronal toxicity is completely abrogated in the absence of Prnp expression, even in experimental paradigms in which PrPSc can still accumulate151–153 . Intriguingly,arecentstudyhasclaimedthatendogenous PrPC may be one of the cell surface receptors mediating synaptic dysfunction associated with oligomeric Aβ154 . In this study, PrPC was identified in an expression clon- ing screen for proteins that could enhance oligomeric Aβ binding to the surface of CoS-7 cells. Furthermore, it was shown that the absence of PrP expression partially rescued Aβ oligomer-mediated deficits in long-term potentiation. Conformation-specific antibodies that rec- ognize oligomeric forms of Aβ also seem to be capable of recognizing the oligomeric forms of other amyloid- forming proteins, indicating that oligomers of diverse proteins have common structural motifs, similar to mature amyloid fibrils. This observation suggests the interesting possibility that PrPC might be capable of binding other oligomeric species and function physio- logically as a general ‘aggregation receptor’ for a wide range of amyloid-forming proteins. Several seemingly unrelated observations support this hypothesis. For example, PrPC is a glycosylphosphatidyl- inositol-anchored protein and therefore a permanent resident of lipid rafts155,156 . If PrPC is an aggregation detec- tor, this could explain why oligomerization increases the affinity of proteins for lipid rafts157 . Furthermore, it has been shown that endosomes containing lipid rafts are preferentially targeted to the lysosomal pathway rather than recycling to the cell surface158 , which implies that PrPC binding of protein aggregates could target these aggregates for degradation. So, at what point does pro- tein aggregation become toxic? one possibility is that, at sufficient concentrations, extracellular protein aggregates may cause clustering of PrPC , leading to a conformational change in PrP secondary structurethat activatesapoptotic pathways. This hypothesis is supported by several lines of evidence indicating that aggregation and/or conforma- tional change of PrPC triggers a pro-apoptotic signalling cascade134,159–161,167 . Alternatively, internalization and lyso- somal accumulation of insoluble aggregates might also be toxic (FIG. 5). Regardless of the precise mechanism, it is an intriguing idea that PrPC may serve as a general cell surface aggregation detector, and it could have important therapeutic consequences. First, this theory implies that oligomeric species from diverse aggregation disorders mayalltriggercellulartoxicitythroughcommonpathways. Second,itraisesthepossibilitythatPrPC -targetedtherapies might be broadly applicable to many amyloidoses. The future of amyloid therapeutics Although many challenges remain for amyloid therapeu- tics, the field is steadily moving forward thanks to vigor- ous and innovative research efforts. encouraging results from animal models and several promising immuno- therapies, secretase inhibitors and anti-aggregation compounds that are currently in clinical trials provide hope that the first disease-modifying treatments for amyloidoses may soon become available. Figure 5 | Possible roles of PrPc in oligomer-mediated toxicity. a | Normally folded prion protein (PrPC ) is a glyco- phosphatidylinositol -anchored cell surface protein and a permanent resident of lipid rafts. The physiological function of PrPC is unknown; however, an intriguing possibility is that cell surface PrPC may bind potentially toxic extracellular oligomeric species and target them to the lysosome for degradation. b | At high, pathological concentrations, toxic oligomers may induce clustering of and/or a conformational change in cell surface PrPC . This may lead to the direct induction of cell death pathways. Alternatively (or in combination), PrPC -mediated lysosomal accumulation of oligomers may induce cellular toxicity. REVIEWS NATuRe RevIewS | Drug Discovery voLuMe 9 | MARCH 2010 | 245 © 20 Macmillan Publishers Limited. All rights reserved 10
- 10. 1. Sawaya, M. R. et al. Atomic structures of amyloid cross-β spines reveal varied steric zippers. Nature 447, 453–457 (2007). 2. Virchow, R. Über eine im Gehirn und Rückenmark des Menschen aufgefundene Substanz mit der chemischen Reaktion der Cellulose. Virchows Arch. 6, 135–138 (1853) (in German). 3. Monsellier, E., Ramazzotti, M., Taddei, N. & Chiti, F. Aggregation propensity of the human proteome. PLoS Comput. Biol. 4, e1000199 (2008). 4. Hull, R. L., Westermark, G. T., Westermark, P. & Kahn, S. E. Islet amyloid: a critical entity in the pathogenesis of type 2 diabetes. J. Clin. Endocrinol. Metab. 89, 3629–3643 (2004). 5. Berson, J. F. et al. Proprotein convertase cleavage liberates a fibrillogenic fragment of a resident glycoprotein to initiate melanosome biogenesis. J. Cell Biol. 161, 521–533 (2003). 6. Westermark, P. Aspects on human amyloid forms and their fibril polypeptides. FEBS J. 272, 5942–5949 (2005). 7. Vilar, M. et al. The fold of α-synuclein fibrils. Proc. Natl Acad. Sci. USA 105, 8637–8642 (2008). 8. Scherzinger, E. et al. Huntingtin-encoded polyglutamine expansions form amyloid-like protein aggregates in vitro and in vivo. Cell 90, 549–558 (1997). 9. Maezawa, I. et al. Congo red and thioflavin-T analogs detect Aβ oligomers. J. Neurochem. 104, 457–468 (2008). 10. Walsh, D. M. et al. Amyloid β-protein fibrillogenesis. Structure and biological activity of protofibrillar intermediates. J. Biol. Chem. 274, 25945–25952 (1999). 11. Ferreira, S. T., Vieira, M. N. & De Felice, F. G. Soluble protein oligomers as emerging toxins in Alzheimer’s and other amyloid diseases. IUBMB Life 59, 332–345 (2007). 12. Oakley, H. et al. Intraneuronal β-amyloid aggregates, neurodegeneration, and neuron loss in transgenic mice with five familial Alzheimer’s disease mutations: potential factors in amyloid plaque formation. J. Neurosci. 26, 10129–10140 (2006). 13. Casas, C. et al. Massive CA1/2 neuronal loss with intraneuronal and N-terminal truncated Aβ42 accumulation in a novel Alzheimer transgenic model. Am. J. Pathol. 165, 1289–1300 (2004). 14. Masters, C. L. et al. Amyloid plaque core protein in Alzheimer disease and Down syndrome. Proc. Natl Acad. Sci. USA 82, 4245–4249 (1985). 15. Tanzi, R. E. & Bertram, L. Twenty years of the Alzheimer’s disease amyloid hypothesis: a genetic perspective. Cell 120, 545–555 (2005). 16. Barten, D. M. & Albright, C. F. Therapeutic strategies for Alzheimer’s disease. Mol. Neurobiol. 37, 171–186 (2008). 17. Gura, T. Hope in Alzheimer’s fight emerges from unexpected places. Nature Med. 14, 894 (2008). 18. Aguzzi, A. & Haass, C. Games played by rogue proteins in prion disorders and Alzheimer’s disease. Science 302, 814–818 (2003). 19. Dovey, H. F. et al. Functional γ-secretase inhibitors reduce β-amyloid peptide levels in brain. J. Neurochem. 76, 173–181 (2001). 20. Barten, D. M. et al. Dynamics of β-amyloid reductions in brain, cerebrospinal fluid, and plasma of β -amyloid precursor protein transgenic mice treated with a γ-secretase inhibitor. J. Pharmacol. Exp. Ther. 312, 635–643 (2005). 21. Best, J. D. et al. Quantitative measurement of changes in amyloid- β(40) in the rat brain and cerebrospinal fluid following treatment with the γ-secretase inhibitor LY-411575 [N2 -[(2S)-2-(3,5-difluorophenyl)-2-hydroxye thanoyl]-N1 -[(7S)-5-methyl-6-ox o-6,7-dihydro-5H- dibenzo[b,d]azepin-7-yl]-l-alaninamide]. J. Pharmacol. Exp. Ther. 313, 902–908 (2005). 22. Siemers, E. R. et al. Effects of a γ-secretase inhibitor in a randomized study of patients with Alzheimer disease. Neurology 66, 602–604 (2006). 23. De Strooper, B. et al. Deficiency of presenilin-1 inhibits the normal cleavage of amyloid precursor protein. Nature 391, 387–390 (1998). This was the first indication that presenilin 1 was crucial for γ-secretase activity and might constitute a viable drug target for Alzheimer’s disease therapy. 24. De Strooper, B. et al. A presenilin-1-dependent γ-secretase-like protease mediates release of Notch intracellular domain. Nature 398, 518–522 (1999). 25. Wong, P. C. et al. Presenilin 1 is required for Notch1 and DII1 expression in the paraxial mesoderm. Nature 387, 288–292 (1997). 26. Shen, J. et al. Skeletal and CNS defects in Presenilin-1-deficient mice. Cell 89, 629–639 (1997). 27. Wong, G. T. et al. Chronic treatment with the γ-secretase inhibitor LY-411, 575 inhibits β-amyloid peptide production and alters lymphopoiesis and intestinal cell differentiation. J. Biol. Chem. 279, 12876–12882 (2004). 28. Sherrington, R. et al. Cloning of a gene bearing missense mutations in early-onset familial Alzheimer’s disease. Nature 375, 754–760 (1995). 29. Levy-Lahad, E. et al. Candidate gene for the chromosome 1 familial Alzheimer’s disease locus. Science 269, 973–977 (1995). 30. Rogaev, E. I. et al. Familial Alzheimer’s disease in kindreds with missense mutations in a gene on chromosome 1 related to the Alzheimer’s disease type 3 gene. Nature 376, 775–778 (1995). 31. Duff, K. et al. Increased amyloid-β42(43) in brains of mice expressing mutant presenilin 1. Nature 383, 710–713 (1996). 32. Lemere, C. A. et al. The E280A presenilin 1 Alzheimer mutation produces increased Aβ 42 deposition and severe cerebellar pathology. Nature Med. 2, 1146–1150 (1996). 33. Citron, M. et al. Mutant presenilins of Alzheimer’s disease increase production of 42-residue amyloid β-protein in both transfected cells and transgenic mice. Nature Med. 3, 67–72 (1997). 34. Weggen, S. et al. A subset of NSAIDs lower amyloidogenic Aβ42 independently of cyclooxygenase activity. Nature 414, 212–216 (2001). 35. Fraering, P. C. et al. γ-Secretase substrate selectivity can be modulated directly via interaction with a nucleotide-binding site. J. Biol. Chem. 280, 41987–41996 (2005). 36. Imbimbo, B. P. et al. 1-(3′,4′-Dichloro-2-fluoro[1,1′- biphenyl]-4-yl)-cyclopropanecarboxylic acid (CHF5074), a novel γ-secretase modulator, reduces brain β-amyloid pathology in a transgenic mouse model of Alzheimer’s disease without causing peripheral toxicity. J. Pharmacol. Exp. Ther. 323, 822–830 (2007). 37. Kukar, T. et al. Chronic administration of R-flurbiprofen attenuates learning impairments in transgenic amyloid precursor protein mice. BMC Neurosci. 8, 54 (2007). 38. Galasko, D. R. et al. Safety, tolerability, pharmacokinetics, and Aβ levels after short-term administration of R-flurbiprofen in healthy elderly individuals. Alzheimer Dis. Assoc. Disord. 21, 292–299 (2007). 39. Wilcock, G. K. et al. Efficacy and safety of tarenflurbil in mild to moderate Alzheimer’s disease: a randomised phase II trial. Lancet Neurol. 7, 483–493 (2008). 40. Myriad Genetics. Press release June 30: Myriad Genetics reports results of U.S. Phase 3 trial of Flurizan™ in Alzheimer’s disease. Myriad Genetics website [online], http://investor.myriad.com/ releasedetail.cfm?releaseid=325471 (2008). 41. Imbimbo, B. P. & Peretto, I. Semagacestat, a γ-secretase inhibitor for the potential treatment of Alzheimer’s disease. Curr. Opin. Investig. Drugs 10, 721–730 (2009). 42. Thathiah, A. et al. The orphan G protein-coupled receptor 3 modulates amyloid-β peptide generation in neurons. Science 323, 946–951 (2009). 43. Serneels, L. et al. γ-Secretase heterogeneity in the Aph1 subunit: relevance for Alzheimer’s disease. Science 324, 639–642 (2009). 44. Vassar, R. et al. β-Secretase cleavage of Alzheimer’s amyloid precursor protein by the transmembrane aspartic protease BACE. Science 286, 735–741 (1999). 45. Hussain, I. et al. Identification of a novel aspartic protease (Asp 2) as β-secretase. Mol. Cell Neurosci. 14, 419–427 (1999). 46. Lin, X. et al. Human aspartic protease memapsin 2 cleaves the β-secretase site of β-amyloid precursor protein. Proc. Natl Acad. Sci. USA 97, 1456–1460 (2000). 47. Sinha, S. et al. Purification and cloning of amyloid precursor protein β-secretase from human brain. Nature 402, 537–540 (1999). 48. Yan, R. et al. Membrane-anchored aspartyl protease with Alzheimer’s disease β-secretase activity. Nature 402, 533–537 (1999). 49. Luo, Y. et al. Mice deficient in BACE1, the Alzheimer’s β-secretase, have normal phenotype and abolished β-amyloid generation. Nature Neurosci. 4, 231–232 (2001). This was the first demonstration that deficiency in BACE1 abolished β-amyloid production in vivo, establishing the β-secretase as a valid drug target for Alzheimer’s disease. 50. Ohno, M. et al. BACE1 deficiency rescues memory deficits and cholinergic dysfunction in a mouse model of Alzheimer’s disease. Neuron 41, 27–33 (2004). 51. Ohno, M. et al. BACE1 gene deletion prevents neuron loss and memory deficits in 5XFAD APP/PS1 transgenic mice. Neurobiol. Dis. 26, 134–145 (2007). 52. Laird, F. M. et al. BACE1, a major determinant of selective vulnerability of the brain to amyloid-β amyloidogenesis, is essential for cognitive, emotional, and synaptic functions. J. Neurosci. 25, 11693–11709 (2005). 53. McConlogue, L. et al. Partial reduction of BACE1 has dramatic effects on Alzheimer plaque and synaptic pathology in APP transgenic mice. J. Biol. Chem. 282, 26326–26334 (2007). 54. Ghosh, A. K., Kumaragurubaran, N., Hong, L., Koelsh, G. & Tang, J. Memapsin 2 (β-secretase) inhibitors: drug development. Curr. Alzheimer Res. 5, 121–131 (2008). 55. Hu, X. et al. Bace1 modulates myelination in the central and peripheral nervous system. Nature Neurosci. 9, 1520–1525 (2006). 56. Kim, D. Y. et al. BACE1 regulates voltage-gated sodium channels and neuronal activity. Nature Cell Biol. 9, 755–764 (2007). 57. Kitazume, S. et al. In vivo cleavage of α2,6- sialyltransferase by Alzheimer β-secretase. J. Biol. Chem. 280, 8589–8595 (2005). 58. Kuhn, P. H. et al. Regulated intramembrane proteolysis of the interleukin-1 receptor II by α-, β-, and γ-secretase. J. Biol. Chem. 282, 11982–11995 (2007). 59. Li, Q. & Sudhof, T. C. Cleavage of amyloid-β precursor protein and amyloid-β precursor-like protein by BACE 1. J. Biol. Chem. 279, 10542–10550 (2004). 60. Lichtenthaler, S. F. et al. The cell adhesion protein P-selectin glycoprotein ligand-1 is a substrate for the aspartyl protease BACE1. J. Biol. Chem. 278, 48713–48719 (2003). 61. Pastorino, L. et al. BACE (β-secretase) modulates the processing of APLP2 in vivo. Mol. Cell Neurosci. 25, 642–649 (2004). 62. von Arnim, C. A. et al. The low density lipoprotein receptor-related protein (LRP) is a novel β-secretase (BACE1) substrate. J. Biol. Chem. 280, 17777–17785 (2005). 63. Willem, M. et al. β-Site amyloid precursor protein cleaving enzyme 1 increases amyloid deposition in brain parenchyma but reduces cerebrovascular amyloid angiopathy in aging BACE x APP[V717I] double-transgenic mice. Am. J. Pathol. 165, 1621–1631 (2004). 64. Wong, H. K. et al. β Subunits of voltage-gated sodium channels are novel substrates of β-site amyloid precursor protein-cleaving enzyme (BACE1) and γ-secretase. J. Biol. Chem. 280, 23009–23017 (2005). 65. Neugroschl, J. & Sano, M. An update on treatment and prevention strategies for Alzheimer’s disease. Curr. Neurol. Neurosci. Rep. 9, 368–376 (2009). 66. O’Connor, T. et al. Phosphorylation of the translation initiation factor eIF2α increases BACE1 levels and promotes amyloidogenesis. Neuron 60, 988–1009 (2008). 67. Wen, Y. et al. Transcriptional regulation of β-secretase by p25/cdk5 leads to enhanced amyloidogenic processing. Neuron 57, 680–690 (2008). 68. Hebert, S. S. et al. Loss of microRNA cluster miR-29a/b-1 in sporadic Alzheimer’s disease correlates with increased BACE1/β-secretase expression. Proc. Natl Acad. Sci. USA 105, 6415–6420 (2008). 69. Wang, W. X. et al. The expression of microRNA miR-107 decreases early in Alzheimer’s disease and may accelerate disease progression through regulation of β-site amyloid precursor protein-cleaving enzyme 1. J. Neurosci. 28, 1213–1223 (2008). 70. Faghihi, M. A. et al. Expression of a noncoding RNA is elevated in Alzheimer’s disease and drives rapid feed- forward regulation of β-secretase. Nature Med. 14, 723–730 (2008). 71. Tesco, G. et al. Depletion of GGA3 stabilizes BACE and enhances β-secretase activity. Neuron 54, 721–737 (2007). 72. He, W. et al. Reticulon family members modulate BACE1 activity and amyloid-β peptide generation. Nature Med. 10, 959–965 (2004). REVIEWS 246 | MARCH 2010 | voLuMe 9 www.nature.com/reviews/drugdisc © 20 Macmillan Publishers Limited. All rights reserved 10
- 11. 73. Rajendran, L. et al. Efficient inhibition of the Alzheimer’s disease β-secretase by membrane targeting. Science 320, 520–523 (2008). 74. Schenk, D. et al. Immunization with amyloid-β attenuates Alzheimer-disease-like pathology in the PDAPP mouse Nature 400, 173–177 (1999). This was the first successful attempt to modify Alzheimer disease plaque pathology using Aβ immunotherapy in an animal model. 75. Janus, C. et al. Aβ peptide immunization reduces behavioural impairment and plaques in a model of Alzheimer’s disease. Nature 408, 979–982 (2000). 76. Morgan, D. et al. Aβ peptide vaccination prevents memory loss in an animal model of Alzheimer’s disease. Nature 408, 982–985 (2000). 77. Sigurdsson, E. M., Scholtzova, H., Mehta, P. D., Frangione, B. & Wisniewski, T. Immunization with a nontoxic/nonfibrillar amyloid-β homologous peptide reduces Alzheimer’s disease-associated pathology in transgenic mice. Am. J. Pathol. 159, 439–447 (2001). 78. Bard, F. et al. Peripherally administered antibodies against amyloid β-peptide enter the central nervous system and reduce pathology in a mouse model of alzheimer disease. Nature Med. 6, 916–919 (2000). 79. DeMattos, R. B. et al. Peripheral anti-Aβ antibody alters CNS and plasma Aβ clearance and decreases brain Aβ burden in a mouse model of Alzheimer’s disease. Proc. Natl Acad. Sci. USA 98, 8850–8855 (2001). 80. DeMattos, R. B., Bales, K. R., Cummins, D. J., Paul, S. M. & Holtzman, D. M. Brain to plasma amyloid-β efflux: a measure of brain amyloid burden in a mouse model of Alzheimer’s disease. Science 295, 2264–2267 (2002). 81. Dodart, J. C. et al. Immunization reverses memory deficits without reducing brain Aβ burden in Alzheimer’s disease model. Nature Neurosci. 5, 452–457 (2002). 82. Senior, K. Dosing in phase II trial of Alzheimer’s vaccine suspended. Lancet Neurol. 1, 3 (2002). This Phase II study was the first attempt to treat Alzheimer’s disease in humans with a disease-modifying therapy. 83. Gilman, S. et al. Clinical effects of Aβ immunization (AN1792) in patients with AD in an interrupted trial. Neurology 64, 1553–1562 (2005). 84. Dodel, R. C. et al. Intravenous immunoglobulins containing antibodies against β-amyloid for the treatment of Alzheimer’s disease. J. Neurol. Neurosurg. Psychiatry 75, 1472–1474 (2004). 85. Relkin, N. R. et al. 18-Month study of intravenous immunoglobulin for treatment of mild Alzheimer disease. Neurobiol. Aging 30, 1728–1736 (2008). 86. Samuelsson, A., Towers, T. L. & Ravetch, J. V. Anti-inflammatory activity of IVIG mediated through the inhibitory Fc receptor. Science 291, 484–486 (2001). 87. Schenk, D. Amyloid-β immunotherapy for Alzheimer’s disease: the end of the beginning. Nature Rev. Neurosci. 3, 824–828 (2002). 88. Jankowsky, J. L. et al. Persistent amyloidosis following suppression of Aβ production in a transgenic model of Alzheimer disease. PLoS Med. 2, e355 (2005). 89. Gabizon, R., McKinley, M. P., Groth, D. & Prusiner, S. B. Immunoaffinity purification and neutralization of scrapie prion infectivity. Proc. Natl Acad. Sci. USA 85, 6617–6621 (1988). 90. Wilcock, G. K. & Esiri, M. M. Plaques, tangles and dementia. A quantitative study. J. Neurol. Sci. 56, 343–356 (1982). 91. Podlisny, M. B. et al. Aggregation of secreted amyloid β-protein into sodium dodecyl sulfate-stable oligomers in cell culture. J. Biol. Chem. 270, 9564–9570 (1995). 92. Walsh, D. M., Tseng, B. P., Rydel, R. E., Podlisny, M. B. & Selkoe, D. J. The oligomerization of amyloid β-protein begins intracellularly in cells derived from human brain. Biochemistry 39, 10831–10839 (2000). 93. Gong, Y. et al. Alzheimer’s disease-affected brain: presence of oligomeric A β ligands (ADDLs) suggests a molecular basis for reversible memory loss. Proc. Natl Acad. Sci. USA 100, 10417–10422 (2003). 94. Lesne, S. et al. A specific amyloid-β protein assembly in the brain impairs memory. Nature 440, 352–357 (2006). 95. McLaurin, J. et al. Cyclohexanehexol inhibitors of Aβ aggregation prevent and reverse Alzheimer phenotype in a mouse model. Nature Med. 12, 801–808 (2006). 96. Shankar, G. M. et al. Amyloid-β protein dimers isolated directly from Alzheimer’s brains impair synaptic plasticity and memory. Nature Med. 14, 837–842 (2008). 97. Walsh, D. M. et al. The role of cell-derived oligomers of Aβ in Alzheimer’s disease and avenues for therapeutic intervention. Biochem. Soc. Trans. 33, 1087–1090 (2005). 98. Ma, Q. L. et al. β-Amyloid oligomers induce phosphorylation of tau and inactivation of insulin receptor substrate via c-Jun N-terminal kinase signaling: suppression by omega-3 fatty acids and curcumin. J. Neurosci. 29, 9078–9089 (2009). 99. Li, S. et al. Soluble oligomers of amyloid β protein facilitate hippocampal long-term depression by disrupting neuronal glutamate uptake. Neuron 62, 788–801 (2009). 100. Poon, W. W. et al. β-Amyloid impairs axonal BDNF retrograde trafficking. Neurobiol. Aging 18 Jun 2009 (doi:10.1016/j.neurobiolaging.2009.05.012). 101. Zhao, W. Q. et al. Insulin receptor dysfunction impairs cellular clearance of neurotoxic oligomeric Aβ. J. Biol. Chem. 284, 18742–18753 (2009). 102. De Felice, F. G. et al. Protection of synapses against Alzheimer’s-linked toxins: insulin signaling prevents the pathogenic binding of Aβ oligomers. Proc. Natl Acad. Sci. USA 106, 1971–1976 (2009). 103. Kayed, R. & Glabe, C. G. Conformation-dependent anti-amyloid oligomer antibodies. Methods Enzymol. 413, 326–344 (2006). 104. Gouras, G. K. et al. Intraneuronal Aβ42 accumulation in human brain. Am. J. Pathol. 156, 15–20 (2000). 105. Zerbinatti, C. V. et al. Apolipoprotein E and low density lipoprotein receptor-related protein facilitate intraneuronal Aβ42 accumulation in amyloid model mice. J. Biol. Chem. 281, 36180–36186 (2006). 106. Tampellini, D. et al. Synaptic activity reduces intraneuronal Aβ, promotes APP transport to synapses, and protects against Aβ-related synaptic alterations. J. Neurosci. 29, 9704–9713 (2009). 107. Spencer, B. et al. Long-term neprilysin gene transfer is associated with reduced levels of intracellular Aβ and behavioral improvement in APP transgenic mice. BMC Neurosci. 9, 109 (2008). 108. Arbel, M. & Solomon, B. Immunotherapy for Alzheimer’s disease: attacking amyloid-β from the inside. Trends Immunol. 28, 511–513 (2007). 109. Kitazawa, M., Vasilevko, V., Cribbs, D. H. & LaFerla, F. M. Immunization with amyloid-β attenuates inclusion body myositis-like myopathology and motor impairment in a transgenic mouse model. J. Neurosci. 29, 6132–6141 (2009). 110. Wegenast-Braun, B. M. et al. Independent effects of intra- and extracellular Aβ on learning-related gene expression. Am. J. Pathol. 175, 271–282 (2009). 111. Aguzzi, A., Sigurdson, C. & Heikenwaelder, M. Molecular mechanisms of prion pathogenesis. Annu. Rev. Pathol. 3, 11–40 (2008). 112. Aguzzi, A. Cell biology: Beyond the prion principle. Nature 459, 924–925 (2009). 113. Klein, M. A. et al. A crucial role for B cells in neuroinvasive scrapie. Nature 390, 687–690 (1997). 114. Klein, M. A. et al. Complement facilitates early prion pathogenesis. Nature Med. 7, 488–492 (2001). 115. Prinz, M. et al. Positioning of follicular dendritic cells within the spleen controls prion neuroinvasion. Nature 425, 957–962 (2003). 116. Prinz, M. et al. Lymph nodal prion replication and neuroinvasion in mice devoid of follicular dendritic cells. Proc. Natl Acad. Sci. USA 99, 919–924 (2002). 117. Bremer, J. et al. Repetitive immunization enhances the susceptibility of mice to peripherally administered prions. PLoS One 4, e7160 (2009). 118. Sigurdson, C. J. et al. Bacterial colitis increases susceptibility to oral prion disease. J. Infect. Dis. 199, 243–252 (2009). 119. Ligios, C. et al. PrPSc in mammary glands of sheep affected by scrapie and mastitis. Nature Med. 11, 1137–1138 (2005). 120. Heikenwalder, M. et al. Chronic lymphocytic inflammation specifies the organ tropism of prions. Science 307, 1107–1110 (2005). 121. Prinz, M. et al. Prion pathogenesis in the absence of Toll-like receptor signalling. EMBO Rep. 4, 195–199 (2003). 122. Heppner, F. L. et al. Experimental autoimmune encephalomyelitis repressed by microglial paralysis. Nature Med. 11, 146–152 (2005). 123. Aguzzi, A. & Sigurdson, C. J. Antiprion immunotherapy: to suppress or to stimulate? Nature Rev. Immunol. 4, 725–736 (2004). 124. Montrasio, F. et al. Impaired prion replication in spleens of mice lacking functional follicular dendritic cells. Science 288, 1257–1259 (2000). This was the first successful attempt to block peripheral prion replication pharmacologically in an animal model. 125. Heikenwalder, M. et al. Lymphotoxin-dependent prion replication in inflammatory stromal cells of granulomas. Immunity 29, 998–1008 (2008). 126. Nuvolone, M., Aguzzi, A. & Heikenwalder, M. Cells and prions: a license to replicate. FEBS Lett. 583, 2674–2684 (2009). 127. Sigurdsson, E. M. et al. Immunization delays the onset of prion disease in mice. Am. J. Pathol. 161, 13–17 (2002). 128. Magri, G. et al. Decrease in pathology and progression of scrapie after immunisation with synthetic prion protein peptides in hamsters. Vaccine 23, 2862–2868 (2005). 129. Polymenidou, M. et al. Humoral immune response to native eukaryotic prion protein correlates with anti- prion protection. Proc. Natl Acad. Sci. USA 101, 14670–14676 (2004). 130. Sigurdsson, E. M. et al. Anti-prion antibodies for prophylaxis following prion exposure in mice. Neurosci. Lett. 336, 185–187 (2003). 131. Souan, L. et al. Modulation of proteinase-K resistant prion protein by prion peptide immunization. Eur. J. Immunol. 31, 2338–2346 (2001). 132. Heppner, F. L. et al. Prevention of scrapie pathogenesis by transgenic expression of anti-prion protein antibodies. Science 294, 178–182 (2001). This was the first demonstration that the course of prion disease could be significantly altered by PrP antibodies. 133. White, A. R. et al. Monoclonal antibodies inhibit prion replication and delay the development of prion disease. Nature 422, 80–83 (2003). 134. Solforosi, L. et al. Cross-linking cellular prion protein triggers neuronal apoptosis in vivo. Science 303, 1514–1516 (2004). 135. Trevitt, C. R. & Collinge, J. A systematic review of prion therapeutics in experimental models. Brain 129, 2241–2265 (2006). 136. Kolstoe, S. E. et al. Molecular dissection of Alzheimer’s disease neuropathology by depletion of serum amyloid P component. Proc. Natl Acad. Sci. USA 106, 7619–7623 (2009). 137. Doh-Ura, K., Iwaki, T. & Caughey, B. Lysosomotropic agents and cysteine protease inhibitors inhibit scrapie-associated prion protein accumulation. J. Virol. 74, 4894–4897 (2000). 138. Korth, C., May, B. C., Cohen, F. E. & Prusiner, S. B. Acridine and phenothiazine derivatives as pharmacotherapeutics for prion disease. Proc. Natl Acad. Sci. USA 98, 9836–9841 (2001). 139. Ryou, C. et al. Differential inhibition of prion propagation by enantiomers of quinacrine. Lab. Invest. 83, 837–843 (2003). 140. Doh-Ura, K. et al. Treatment of transmissible spongiform encephalopathy by intraventricular drug infusion in animal models. J. Virol. 78, 4999–5006 (2004). 141. Barret, A. et al. Evaluation of quinacrine treatment for prion diseases. J. Virol. 77, 8462–8469 (2003). 142. Collinge, J. et al. Safety and efficacy of quinacrine in human prion disease (PRION-1 study): a patient- preference trial. Lancet Neurol. 8, 334–344 (2009). This was the first anti-aggregation compound to be tested for efficacy in the treatment of prion disease in humans. 143. Perrier, V. et al. Mimicking dominant negative inhibition of prion replication through structure- based drug design. Proc. Natl Acad. Sci. USA 97, 6073–6078 (2000). 144. Reddy, T. R. et al. Library design, synthesis, and screening: pyridine dicarbonitriles as potential prion disease therapeutics. J. Med. Chem. 49, 607–615 (2006). 145. Soto, C. et al. Reversion of prion protein conformational changes by synthetic β-sheet breaker peptides. Lancet 355, 192–197 (2000). REVIEWS NATuRe RevIewS | Drug Discovery voLuMe 9 | MARCH 2010 | 247 © 20 Macmillan Publishers Limited. All rights reserved 10
- 12. 146. Soto, C. et al. β-Sheet breaker peptides inhibit fibrillogenesis in a rat brain model of amyloidosis: implications for Alzheimer’s therapy. Nature Med. 4, 822–826 (1998). 147. Ma, J., Brewer, H. B., Jr. & Potter, H. Alzheimer Aβ neurotoxicity: promotion by antichymotrypsin, ApoE4; inhibition by A β-related peptides. Neurobiol. Aging 17, 773–780 (1996). 148. Pepys, M. B. et al. Targeted pharmacological depletion of serum amyloid P component for treatment of human amyloidosis. Nature 417, 254–259 (2002). 149. Sigurdson, C. J. et al. Prion strain discrimination using luminescent conjugated polymers. Nature Methods 4, 1023–1030 (2007). 150. Sekijima, Y., Kelly, J. W. & Ikeda, S. Pathogenesis of and therapeutic strategies to ameliorate the transthyretin amyloidoses. Curr. Pharm. Des. 14, 3219–3230 (2008). 151. Brandner, S. et al. Normal host prion protein necessary for scrapie-induced neurotoxicity. Nature 379, 339–343 (1996). 152. Mallucci, G. et al. Depleting neuronal PrP in prion infection prevents disease and reverses spongiosis. Science 302, 871–874 (2003). 153. Chesebro, B. et al. Anchorless prion protein results in infectious amyloid disease without clinical scrapie. Science 308, 1435–1439 (2005). 154. Lauren, J., Gimbel, D. A., Nygaard, H. B., Gilbert, J. W. & Strittmatter, S. M. Cellular prion protein mediates impairment of synaptic plasticity by amyloid-β oligomers. Nature 457, 1128–1132 (2009). 155. Rodgers, W., Crise, B. & Rose, J. K. Signals determining protein tyrosine kinase and glycosyl-phosphatidylinositol-anchored protein targeting to a glycolipid-enriched membrane fraction. Mol. Cell Biol. 14, 5384–5391 (1994). 156. Arreaza, G. & Brown, D. A. Sorting and intracellular trafficking of a glycosylphosphatidylinositol-anchored protein and two hybrid transmembrane proteins with the same ectodomain in Madin-Darby canine kidney epithelial cells. J. Biol. Chem. 270, 23641–23647 (1995). 157. Harder, T., Scheiffele, P., Verkade, P. & Simons, K. Lipid domain structure of the plasma membrane revealed by patching of membrane components. J. Cell Biol. 141, 929–942 (1998). 158. Fivaz, M. et al. Differential sorting and fate of endocytosed GPI-anchored proteins. EMBO J. 21, 3989–4000 (2002). 159. Shmerling, D. et al. Expression of amino-terminally truncated PrP in the mouse leading to ataxia and specific cerebellar lesions. Cell 93, 203–214 (1998). 160. Baumann, F. et al. Lethal recessive myelin toxicity of prion protein lacking its central domain. EMBO J. 26, 538–547 (2007). 161. Li, A. et al. Neonatal lethality in transgenic mice expressing prion protein with a deletion of residues 105–125 EMBO J. 26, 548–558 (2007). 162. Luhrs, T. et al. 3D structure of Alzheimer’s amyloid-β(1–42) fibrils. Proc. Natl Acad. Sci. USA 102, 17342–17347 (2005). 163. Heikenwalder, M.et al. Germinal center B cells are dispensable in prion transport and neuroinvasion. J. Neuroimmunol. 192, 113–123 (2007). 164. Sponarova, J., Nystrom, S. N. & Westermark G. T. AA-amyloidosis can be transferred by peripheral blood monocytes. PLoS ONE 3, e3308 (2008). 165. Mabbott, N. A., Young, J., McConnell, I & Bruce, M. E. Follicular dendritic cell dedifferentiation by treatment with an inhibitor of the lymphotoxin pathway dramatically reduces scrapie susceptibility. J. Virol. 77, 6854–6854 (2003). 166. Nilsson, K. P. et al. Structural typing of systemic amyloidoses by luminescent-conjugated polymer spectroscopy. Am. J. Pathol. 176, 563–574 (2010). 167. Hetz, C. et al. Caspase-12 and endoplasmic reticulum stress mediate neurotoxicity of pathological prion protein. EMBO J. 22, 5435–5445 (2003). 168. Elan. Press Release 8 July 2009: Elan to Showcase Its Leadership in Alzheimer’s Disease at Upcoming International Meeting. Elan website [online], http://newsroom.elan.com/phoenix.zhtml?c= 88326&p=irol-pressroomarticle&ID= 1305585&highlight= (2009). Acknowledgements Stained sections from human Alzheimer’s diseased brains, prion-diseased brains, kidney amyloidosis, and the PrPSc histo- blot were provided courtesy of J. Haybaeck, H. Fischer, V. Kana and M. Heikenwälder of the Institute for Neuropathology at the University Hospital of Zürich, Switzerland. The Aguzzi labo- ratory is supported by grants of the Ernst-Jung-Foundation, the Stammbach foundation, the EU (LUPAS, PRIORITY), the Swiss National Science Foundation, a Sinergia grant, and the National Competence Center on Neural Plasticity and Repair. A.A. is a recipient of an Advanced Grant of the European Research Council. Competing interests statement The authors declare no competing financial interests. DATABASES OMIM: http://www.ncbi.nlm.nih.gov/omim Alzheimer’s disease | Creutzfeldt–Jakob disease | fatal familial insomnia | Gerstmann–Sträussler–Scheinker syndrome | Huntington’s disease | Parkinson’s disease UniProtKB: http://www.uniprot.org APP | BACE1 | PrP | PS1 | SAP | tau FURTHER INFORMATION Adriano Aguzzi’s homepage: http://www.en.usz.ch/ MedicalServices/DeptPathology/Pages/Neuropathology.aspx All links Are AcTive in The online PDf REVIEWS 248 | MARCH 2010 | voLuMe 9 www.nature.com/reviews/drugdisc © 20 Macmillan Publishers Limited. All rights reserved 10