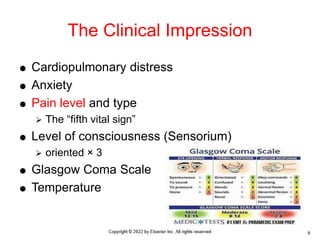
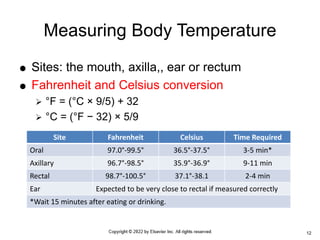
Vital signs (VS) are critical for assessing a patient's health, establishing baselines, and monitoring treatment responses, including temperature, pulse, respiration, and blood pressure. Trends in these vital signs can indicate changes in a patient's condition, guiding further diagnosis and interventions. Accurate measurement and recording are essential, considering individual patient factors such as age and chronic diseases.