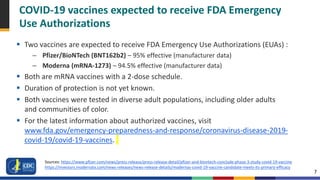
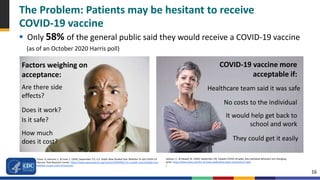
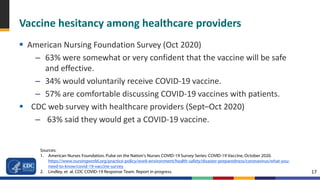
This document provides guidance for building confidence in COVID-19 vaccines among healthcare personnel and patients. It discusses the COVID-19 vaccines that are expected to receive emergency authorization, how they were tested and monitored for safety, and strategies for mitigating side effects like fever and soreness that may cause absenteeism. It also outlines elements of vaccine confidence like safety, effectiveness, and ease of access. Recommended strategies to increase confidence include engaging leaders to promote vaccines, addressing common concerns, and emphasizing the role of healthcare workers in ending the pandemic.