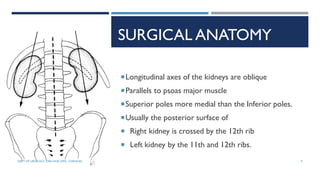
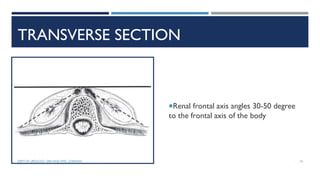
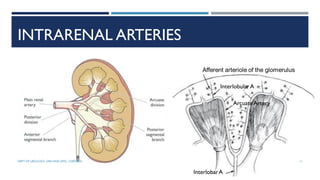
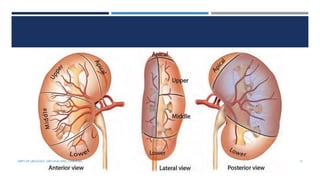
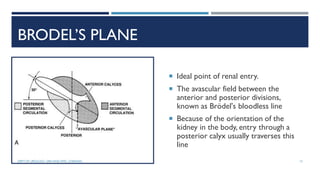
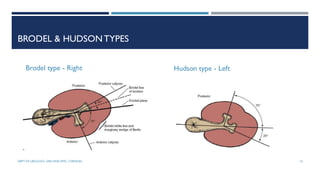
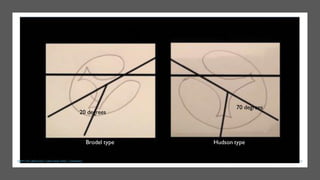
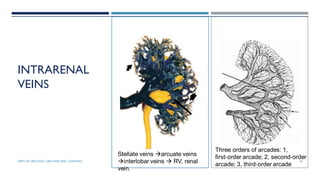
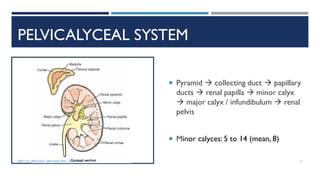
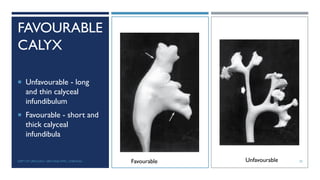
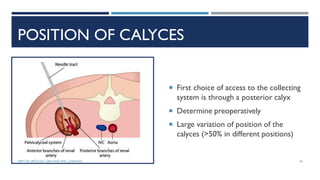
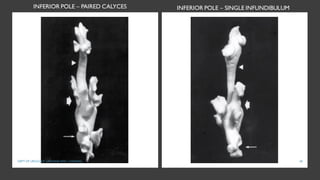
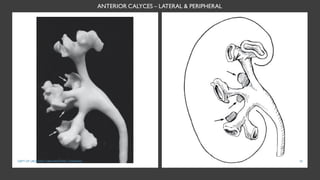
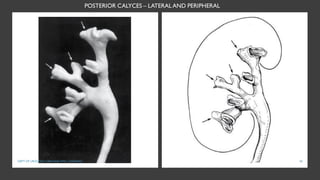
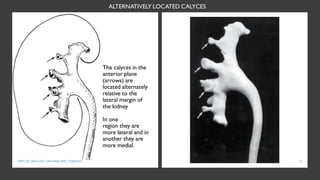
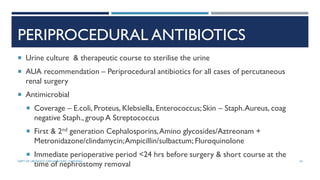
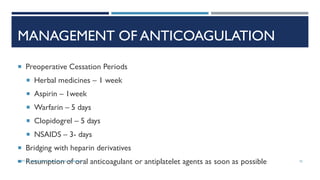
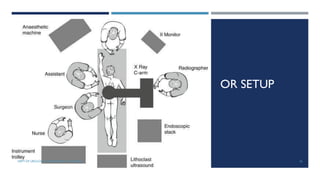
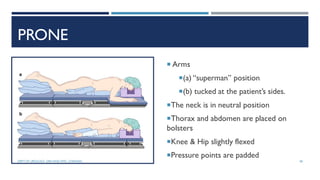
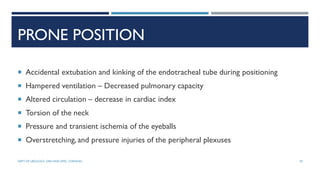
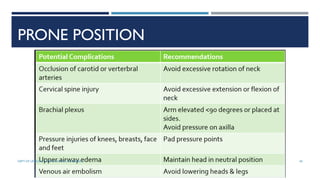
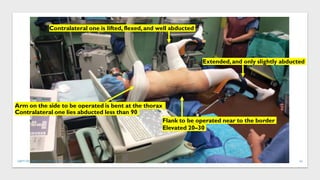
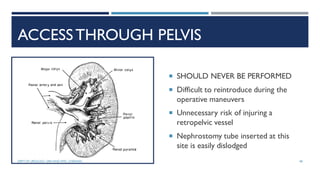
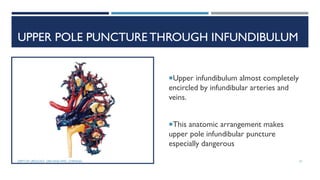
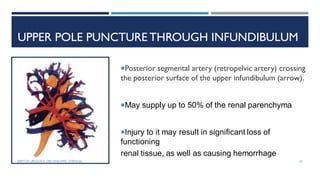
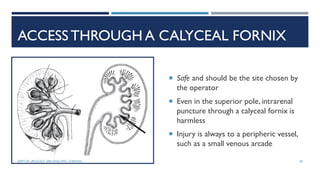
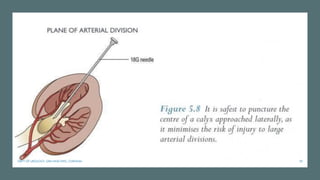
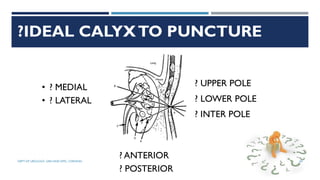
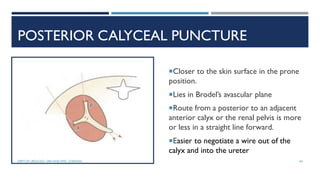
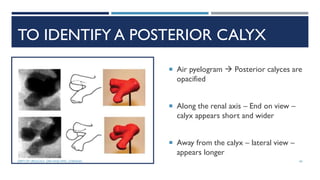
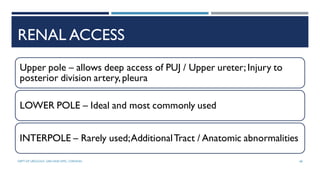
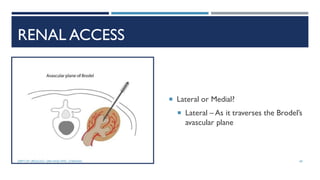
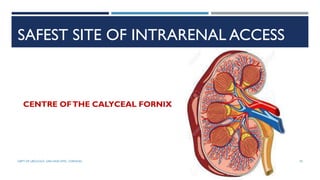
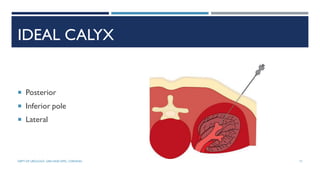
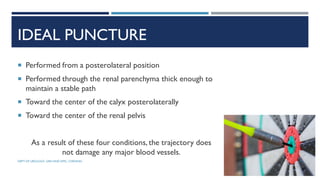
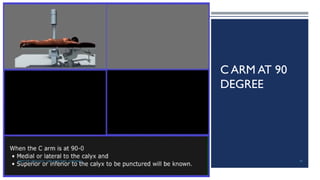
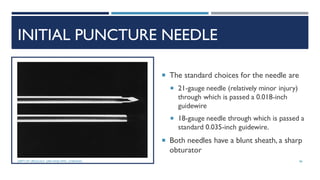
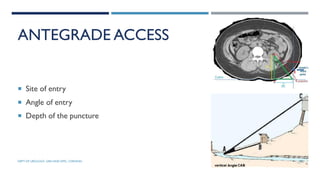
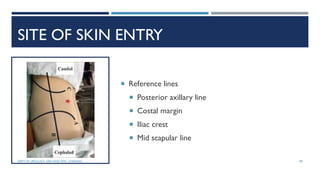
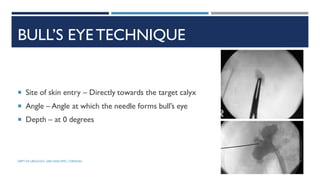
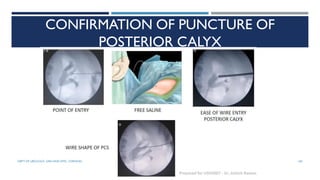
This document provides information about percutaneous nephrolithotomy (PNL) from the Department of Urology at Govt Royapettah Hospital and Kilpauk Medical College in Chennai. It discusses the moderators of the department, indications and contraindications for PNL, preoperative investigations and consent, renal anatomy considerations, PNL technique, intrarenal access points, and patient positioning for the procedure. The document emphasizes accessing the renal collecting system through a posterior calyx rather than the pelvis or infundibulum. It also highlights important anatomical structures like Brodel's plane to aid safe access during PNL.