This document is a doctoral thesis submitted by Dein Vindigni to the University of Newcastle for the degree of Doctor of Philosophy in October 2004. The thesis examines the musculoskeletal health of Indigenous Australians living in rural communities. It acknowledges the supervision team and expresses gratitude to the Indigenous community, cultural elders, and others who supported the research. The thesis contains 7 chapters that review the burden of musculoskeletal conditions, associated risk factors, opportunities and barriers to management, and a pilot training program for Aboriginal Health Workers to address musculoskeletal health in the community.






































![- Prologue - 20
What are the guiding principles of Health Promotion?
The guiding principles of this thesis were drawn from health promotion theory,
which advocates that programs are more likely to be successful when the
modifiable determinants of the health problem are well understood, and the
needs and motivations of the target community are acknowledged and
addressed (Sanson-Fisher & Campbell, 1994; Nutbeam & Harris, 2002). Health
promotion has been defined as:
‘The process of enabling people to increase control over, and
to improve, their health. To reach a state of complete physical,
mental and social well being an individual must be able to
identify and realise aspirations, to satisfy needs and to change
or cope with the environment’
(World Health Organisation [WHO], 1986).
Defining the problem by identifying the magnitude of the health condition(s)
often involves drawing on epidemiological and demographic information as well
as an understanding of the Communities’ needs and priorities. According to
health promotion theory, the nature and quality of available evidence act as a
guide for the choice and design of health promotion activity. Where sufficient
evidence is not available, or the evidence is of poor quality, the researcher is
required to gain data to offset the identified deficiency in evidence (Tugwell et
al., 1985; Hawe, Degeling & Hall, 1990; Green & Kreuter, 1991; Wiggers &
Sanson-Fisher, 1998).
It is now well recognised that the ability of individuals to achieve positive health
outcomes can be significantly increased by enhancing the competence of the
community in which they live to address the broader health issues (Nutbeam &
Harris, 2002). Applying health promotion frameworks when planning an
intervention with community members can assist in comprehensive planning
through identifying options, predicting issues of potential importance, selecting
appropriate options, and explaining difficulties that frequently arise in practice
(Nutbeam & Harris, 2002). Figure 6 outlines the steps towards promoting the
musculoskeletal health of Indigenous people living in rural Communities using a](https://image.slidesharecdn.com/thesis-130609031900-phpapp02/85/Thesis-39-320.jpg)






![- Synopsis - 27
(AHWs) who participated in the MTP. This project was a collaborative initiative
between the Durri Aboriginal Medical Service (AMS), Booroongen Djugun
Aboriginal Health College and the School of Medical Practice and Population
Health, Faculty of Health, The University of Newcastle. The collaborative nature
of this initiative was in response to current thinking in Indigenous health, that the
drive and direction for changes to Aboriginal health must come from within
Aboriginal Communities (Houston & Legge, 1992).
The guidelines prepared by the National Health and Medical Research Council
(NH&MRC, 1999) on ethical matters in Aboriginal research were consulted
throughout the development of the survey, clinical assessment, data collection
and intervention phases of the project. In accordance with these guidelines,
AHWs were recruited from the participating Community (NH&MRC, 1999), and
were trained and employed under the auspices of the AMS. Ethics approval to
undertake all aspects of the studies reported in this thesis was obtained from
three sources: Community representatives (via the Durri AMS Board of
Management); the Human Research Ethics Committee (HREC) of The
University of Newcastle; and on an individual basis from participating
Community members.
Chapter one of this thesis provides a definition of the musculoskeletal
conditions under investigation. The focus is on musculoskeletal conditions of
mechanical causes (such as osteoarthritis [OA]) and non-specific origin, as
these have been described as the most significant causes of pain and disability
(Volinn, 1997). This chapter broadly explores the implications of
musculoskeletal conditions in terms of the physical, emotional and economic
burdens they impose. Indigenous people are the focus of this thesis because of
their poor health status in Australia. Although they experience poor health in
general, this includes health burdens associated with musculoskeletal
conditions. Indigenous people living in rural Communities are the particular
focus due to the evident health disadvantage in these Communities (McLennan
& Madden, 1999) and because a substantial proportion of Indigenous
Australians live in rural regions (ABS 1998a).](https://image.slidesharecdn.com/thesis-130609031900-phpapp02/85/Thesis-46-320.jpg)

































































































































































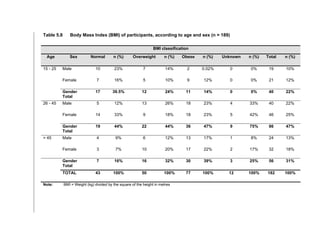
![- Chapter five - 190
5.3.8 Analyses
Analyses of demographic data (including Age, Gender, Occupation, Marital
status) and physical characteristics (Weight, Height, Body Mass Index [BMI])
were used to describe the sample, and explore if the sample obtained was
consistent with previous census findings (Huntington, 2000).
Frequencies were tabulated for Report of musculoskeletal conditions, Body site,
Duration of symptoms, Number of conditions, reported Pain, reported Limitation,
Risk factors and Management of conditions. Data pertaining to reported levels
of Pain, Limitation attributable to the reported Pain, Duration of symptoms,
Number of conditions, Risk factors and Management were grouped into
categories to facilitate comparative analyses.
Chi square analyses (Greenberg et al., 1993) were used to test associations
between musculoskeletal conditions (including Pain, Limitation, Duration of
symptoms, Number of conditions) and factors such as demographic and
physical characteristics, Occupational risk factors, Obesity, Physical inactivity
and Trauma.
While Marital status included ‘Never married’, ‘Married’, ‘De Facto’, ‘Separated’,
‘Divorced’ and ‘Widowed’, these categories were grouped as necessary into
‘Married/De facto’ and ‘No Partner’, to allow for more meaningful comparisons
given the small numbers in each sub-category.
Reported high Pain levels were further examined specifically within the sub-
categories of the most prevalent conditions in the Community including LBP,
neck and shoulder pain. High pain levels were classified as scores greater than
7/10 on a 10-point Likert scale and Low levels were classified as scores less
than 5/10 on the Likert scale.
Reported Limitation was examined within the sub-categories of the most
prevalent conditions. High limitation levels were classified as scores greater
than 6/10 and Low levels as scores less than 5/10 on a Likert 10-point scale.](https://image.slidesharecdn.com/thesis-130609031900-phpapp02/85/Thesis-209-320.jpg)






















































































































![- References - 2
Prologue
Australian Bureau of Statistics (2002). Deaths 2001. Catalogue No. 3302.0.
Canberra, ABS.
Australian Health Ministers’ Advisory Council Standing Committee for Aboriginal
and Torres Strait Islander Health. (2002). Aboriginal and Torres Strait Islander
health workforce national strategic framework. [Canberra], Australian Health
Ministers' Advisory Council: ii, 21.
Buchanan N (2001). Interview with Dein Vindigni on ‘the history of the Dunghutti
Nation since European settlement and beyond’. Interview in Kempsey, NSW,
July 2001.
Cook DJ, Greengold NL, Ellrodt AG, Weingarten SR (1997). The relation
between systematic reviews and practice guidelines. Ann Intern Med 127(3):
210-6.
Couzos S, Murray R, Kimberley Aboriginal Medical Services Council (WA)
(1999). Aboriginal primary health care: an evidence-based approach.
Melbourne, Vic., Oxford University Press.
Durie MH (2003). The health of indigenous peoples. BMJ 326(7388): 510-1.
Gordon P (1998). Interview with Dein Vindigni on ‘The history of Brewarrina’,
NSW, July, 1998.
Green L, Kreuter M (1991). Health Promotion Planning: An Educational and
Environmental Approach. Mountain View CA, Mayfield Publishing Company.
Hawe P, Degeling D, Hall J (1990). Evaluating health promotion: a health
worker's guide. Sydney, MacLennan & Petty.](https://image.slidesharecdn.com/thesis-130609031900-phpapp02/85/Thesis-331-320.jpg)



![- References - 6
Synopsis
Australian Bureau of Statistics (1998a). 1996 census population and housing:
community profiles for Australia. Cat. No. 2020.0. Canberra, ABS.
Australian Bureau of Statistics. (1998b). Experimental estimates of the
Aboriginal and Torres Strait Islander population, 30 June 1991 - 30 June 1996.
[Canberra], Australian Bureau of Statistics.
Donovan RJ, Spark R (1997). Towards guidelines for survey research in remote
Aboriginal Communities. Aust N Z J Public Health 21(1): 89-95.
Durie MH (2003). The health of indigenous peoples. BMJ 326(7388): 510-1.
Dwyer AP (1987). Backache and its prevention. Clin Orthop (222): 35-43.
Gordon P (1998). Interview with Dein Vindigni on ‘The history of Brewarrina’,
NSW, July, 1998.
Green L, Kreuter M. Health Promotion Planning. An Educational and
Environmental Approach. Second Edition. Mayfield Publishing Company,
Mountain View, Toronto, London, 1991.
Houston S, Legge D (1992). Aboriginal health research and the National
Aboriginal Health Strategy. Aust J Public Health 16(2): 114-5.
Li'Dthia Warrawee'a K (2000). An aboriginal perspective on holistic health.
Diversity, Natural & Complementary Health 2(2): 2-9.
McLennan W, Madden R (1999). The Health and Welfare of Australia’s
Aboriginal and Torres Straight Islander Peoples. Canberra, Australian Bureau of
Statistics & the Australian Institute of Health and Welfare, ABS Catalogue no.
4704.00 AIHW Catalogue no. IHW 3.](https://image.slidesharecdn.com/thesis-130609031900-phpapp02/85/Thesis-335-320.jpg)

![- References - 8
Chapter one
Aaronson NK, Muller M, Cohen PD, et al. (1998). Translation, validation, and
forming of the Dutch language version of the SF-36 Health Survey in community
and chronic disease populations. J Clin Epidemiol 51(11): 1055-68.
Adams MA, Mannion AF, Dolan P (1999). Personal risk factors for first-time low
back pain. Spine 24(23): 2497-505.
Anderson RT (1984). An orthopaedic ethnography in rural Nepal. Medical
Anthropology 8(1): 46-59.
Andersson G (1997). The epidemiology of spinal disorders. In: Frymoyer JW
(ed). The adult spine: principles and practice. Philadelphia, PA, Lippincott-
Raven: 93-141.
Australian Acute Musculoskeletal Pain Guidelines Group (AAMPG) (2003).
Evidence-based management of acute musculoskeletal pain [Online. Available
at http://www.nhmrc.gov.au ]. Australian Academic Press: Brisbane.
Australian Bureau of Statistics. (1995). National Aboriginal and Torres Strait
Islander survey 1994: detailed findings. Canberra, Australian Bureau of
Statistics, Cat. No. 4190.0.
Australian Bureau of Statistics (1998). 1996 census population and housing:
community profiles for Australia. Cat. No. 2020.0. Canberra, ABS.
Australian Bureau of Statistics (ABS) (1999). National Health Survey: Aboriginal
and Torres Strait Islander Results, 1995, Cat. No. 4806.0, ABS, Canberra.
Australian Bureau of Statistics (2002). Deaths 2001. Catalogue No 3302.0.
Canberra, ABS.](https://image.slidesharecdn.com/thesis-130609031900-phpapp02/85/Thesis-337-320.jpg)
![- References - 9
Australian Health Infonet (2003). Summary of Indigenous health: hospitalisation.
Available at: www.healthinfonet.ecu.edu.au (Accessed 27 August, 2003).
Australian Health Ministers' Advisory Council Standing Committee for Aboriginal
and Torres Strait Islander Health. (2002). Aboriginal and Torres Strait Islander
health workforce national strategic framework. [Canberra], Australian Health
Ministers' Advisory Council:
ii, 21.
Australian Institute of Health and Welfare (1997). Australia’s Welfare. Cat. No.
AUS 8. Canberra, Australian Government Publishing Service.
Australian Institute of Health and Welfare (2000). Australia's Health 2000: the
seventh biennial health report of the Australian Institute of Health and Welfare.
Canberra: AIHW.
Australian Institute of Health and Welfare (2002a). Australia’s Health 2002: the
eighth biennial health report of the Australian Institute of Health and Welfare.
Canberra, Australian Institute of Health and Welfare.
Australian Institute of Health and Welfare (2002b). Health system costs of
injury, poisoning and musculoskeletal disorders in Australia 1993-94. Available
at: www.aihw.gov.au (Accessed July 29 2003). Canberra, Australian
Government Publishing Service.
Australian Institute of Health and Welfare, Britt H, Miller G, Charles J, et al.
(2000). General practice activity in Australia 1999-00. General Practice Series
No. 5. AIHW Cat. No. GEP 5. Canberra: AIHGW GPSCU.
Australian Institute of Health and Welfare, Mathers C & Penm R (1999). Health
system costs of injury, poisoning and musculoskeletal disorders in Australia
1993-94. Health and Welfare Expenditure Series No 6. AIHW Cat. No. HWE 12
Canberra: AIHW.](https://image.slidesharecdn.com/thesis-130609031900-phpapp02/85/Thesis-338-320.jpg)
![- References - 10
Barnsley L, Lord S, Bogduk N (1993). The pathophysiology of whiplash. Spine:
state of the art reviews 7: 329-53.
Becker N, Bondegaard Thomsen A, Olsen AK, et al. (1997). Pain epidemiology
and health related quality of life in chronic non-malignant pain patients referred
to a Danish multidisciplinary pain center. Pain 73(3): 393-400.
Berkow R (1992). Merck Manual of Diagnosis and Therapy, Chapter 11
Neurological Disorders. Sixteenth Edition, Merck & Co., New Jersey, USA,
1380-1526.
Biering-Sorensen F (1982). Low back trouble in a general population of 30-, 40-,
50-, and 60-year-old men and women. Study design, representativeness and
basic results. Danish Medical Bulletin 29(6): 289-99.
Black K, Eckerman S (1997). Disability support services provided under the
Commonwealth/State Disability Agreement: first national data 1995. Canberra
AIHW.
Boreham P, Whitehouse G, Harley B (1993). The labour force status of
Aboriginal people: a regional comparison. Labour and Industry 5(1): 16-32.
Boudreau LA, Reitav J (2001). Psychosocial and physical factors in work
transition leading to musculoskeletal pain. Journal of the Neuro
musculoskeletal System 9(4): 129-34.
Bowling A (1997). The Conceptualization of Functioning, Health and Quality of
Life. Pg 1-3. In: Bowling A. Measuring health. A review of quality of life
measurement scales. 2nd Ed. Buckingham, Philadelphia, Open University
Press.
Britt H (1994). Patient reasons for encounter in general practice in Australia.
[Thesis] University of Sydney.](https://image.slidesharecdn.com/thesis-130609031900-phpapp02/85/Thesis-339-320.jpg)




![- References - 15
Lawrence RC, Everett DF, Benevolenskaya LI, et al. (1996).
Spondyloarthropathies in circumpolar populations: I. Design and methods of
United States and Russian studies. Arctic Medical Research. 55(4): 187-94.
Leboeuf-Yde C & Lauritsen JM (1995). The prevlance of low back pain in the
literature. A structured review of 26 Nordic studies from 1954 to 1993. Spine.
20(19): 2112-8
Lee TG (1998). Indigenous Health. A Needs Assessment Study of the Outer
Eastern Metropolitan Region of Melbourne. Detailed Report. Victoria, Yarra
Ranges Health Service.
Lehoczky, et al. (2002). Hospital statistics. Aboriginal and Torres Strait Islander
Australians. 1999-2000. Canberra: Australian Bureau of Statistics.
Levy E, Ferme A, Perocheau D, Bono I (1993). [Socioeconomic costs of
osteoarthritis in France]. Revue du Rhumatisme. Edition Francaise 60(6 Pt 2):
63S-7S.
Loney PL, Stratford PW (1999). The prevalence of low back pain in adults: a
methodological review of the literature. Physical Therapy 79(4): 384-96.
March LM, Bachmeier CJ (1997). Economics of osteoarthritis: a global
perspective. Baillieres Clinical Rheumatology 11(4): 817-34.
Mathers C, Vos T, Stevenson C (1999). The burden of disease and injury in
Australia. Canberra, Australian Institute of Health and Welfare, AIHW Catalogue
No. PHE 17.
Matsui H, Maeda A, Tsuji H, Naruse Y (1997). Risk indicators of low back pain
among workers in Japan. Association of familial and physical factors with low
back pain. Spine 22(11): 1242-7; Discussion 8.](https://image.slidesharecdn.com/thesis-130609031900-phpapp02/85/Thesis-344-320.jpg)








![- References - 24
Chapter three
Royal Society, New South Wales, 1889, xxiii, p.491. Cited in: Basedow H. The
Journal of Tropical Medicine and Hygiene, p.230, August 1st, 1932.
Australian Wild Herb Bulletin, September 2000, Volume 2, Issue 3, p.1-7.
Aagaard-Hansen J, Saval P, Steino P, Storr-Paulsen A (1991). [Back health of
students]. Nord Med 106(3): 80-1.
Aagaard-Hansen J, Storr-Paulsen AA (1995). A comparative study of three
different kinds of school furniture. Ergonomics 38(5): 1025-35.
Adams MA, Mannion AF, Dolan P (1999). Personal risk factors for first-time low
back pain. Spine 24(23): 2497-505.
Alcouffe J, Manillier P, Brehier M, Fabin C, Faupin F (1999). Analysis by sex of
low back pain among workers from small companies in the Paris area: severity
and occupational consequences. Occup Environ Med 56(10): 696-701.
Australian Bureau of Statistics. (1995). National Aboriginal and Torres Strait
Islander survey 1994: detailed findings. Canberra, Australian Bureau of
Statistics.
Australian Institute of Health and Welfare. Health system costs of injury,
poisoning and musculoskeletal disorders in Australia 1993-94. Published,
1995. Available at: www.aihw.gov.au (Accessed July 29, 2003).
Australian Institute of Health and Welfare. (2002a). Australia's Health 2002: the
eighth biennial health report of the Australian Institute of Health and Welfare.
Canberra, Australian Institute of Health and Welfare.](https://image.slidesharecdn.com/thesis-130609031900-phpapp02/85/Thesis-353-320.jpg)












![- References - 37
Papageorgiou AC, Macfarlane GJ, Thomas E, et al. (1997). Psychosocial
factors in the workplace-do they predict new episodes of low back pain?
Evidence from the South Manchester Back Pain Study. Spine 22(10): 1137-42.
Pope MH, Wilder DG, Magnusson ML (1999). A review of studies on seated
whole body vibration and low back pain. Proc Inst Mech Eng [H] 213(6): 435-46.
Preyde M (2000). Effectiveness of massage therapy for subacute low-back
pain: a randomised controlled trial. CMAJ 162(13): 1815-20.
Riihimaki H, Viikari-Juntura E, Moneta G, et al. (1994). Incidence of sciatic pain
among men in machine operating, dynamic physical work, and sedentary work.
A three-year follow-up. Spine 19(2): 138-42.
Roquelaure Y, Mechali S, Dano C, et al. (1997). Occupational and personal risk
factors for carpal tunnel syndrome in industrial workers. Scand J Work Environ
Health 23(5): 364-9.
Ryden LA, Molgaard CA, Bobbitt S, Conway J (1989). Occupational low-back
injury in a hospital employee population: an epidemiologic analysis of multiple
risk factors of a high-risk occupational group. Spine 14(3): 315-20.
Saggers S, Gray D (1991). Aboriginal Health and Society: the traditional and
contemporary Aboriginal struggle for Better Health. Sydney, Allen and Unwin.
Salminen JJ (1984). The adolescent back. A field survey of 370 Finnish
schoolchildren. Acta Paediatr Scand Suppl 315: 1-122.
Salminen J, Pentti J, Terho P (1992). Low back pain and disability in 14-year-
old schoolchildren. Abstracts of the Third International Congress: Back pain-
current concepts and recent advances, Scandinavia.](https://image.slidesharecdn.com/thesis-130609031900-phpapp02/85/Thesis-366-320.jpg)
![- References - 38
Salminen JJ, Maki P, Oksanen A, Pentti J (1992). Spinal mobility and trunk
muscle strength in 15-year-old schoolchildren with and without low-back pain.
Spine 17(4): 405-11.
Schonstein E, Kenny DT, Keating J, Koes BW (2003). Work conditioning, work
hardening and functional restoration for workers with back and neck pain
(Cochrane Review). The Cochrane Library, Issue 3. Oxford: Updated Software.
Scutter S, Turker KS, Hall R (1997). Headaches and neck pain in farmers.
Australian Journal of Rural Health. 5(1): 2-5.
Snook SH (1988). Approaches to the control of back pain in industry: job
design, job placement and education/training. Occup Med 3(1): 45-59.
Storr-Paulsen AA (1995). A comparative study of three different kinds of school
furniture. Ergonomics 38(5): 1025-35.
Taplin Rev (1875). Report Sub-Protector Aborigines, South Australia,
December, p.6.
Thomson N, Paterson B. Aboriginal and Torres Strait Islander health
bibliography. National Aboriginal and Torres Strait Islander Health
Clearinghouse, Dept. of Health Studies, Edith Cowan University, Joondalup,
WA. Availabe at: http://www.healthinfonet.ecu.edu.au (Accessed November
12, 2003].
Towheed TE, Anastassiades TP, Shea B, et al. (2003). Glucosamine therapy
for treating osteoarthritis (Cochrane Review). The Cochrane Library, Issue 3.
Oxford: Updated Software.
Troussier B, Davoine P, de Gaudemaris R, Fauconnier J, Phelip X (1994). Back
pain in school children. A study among 1178 pupils. Scand J Rehabil Med
26(3): 143-6.](https://image.slidesharecdn.com/thesis-130609031900-phpapp02/85/Thesis-367-320.jpg)

![- References - 40
Westhof E, Ernst E (1992). [The history of massage] Dtsch Med Wochenschr;
117(4):150-153.
Wiggers J, Sanson-Fisher R (1998). Evidence-based health promotion. In:
Scott, D and Weston, R. Evaluating Health Promotion. London, Stanley Thornes
Ltd.
Wigley R, Manahan L, Muirden KD, et al. (1991). Rheumatic disease in a
Philippine village. II: a WHO-ILAR-APLAR COPCORD study, phases II and III.
Rheumatology International. 11(4-5): 157-61.
Wigley RD, Zhang NZ, Zeng QY, et al. (1994). Rheumatic diseases in China:
ILAR-China study comparing the prevalence of rheumatic symptoms in northern
and southern rural populations. Journal of Rheumatology. 21(8): 1484-90.
Wiley DC, James G, Jonas J, Crosman ED (1991). Comprehensive school
health programs in Texas public schools. J Sch Health 61(10): 421-5.
Williams K (1999). [Back pain]. Ugeskr Laeger 161(3): 273-4.
World Health Organisation (1996). Regional guidelines. Development of health
promoting schools - a framework for action. Geneva, World Health
Organisation.
World Health Organisation (2003). Scientific Group on the Burden of
Musculoskeletal Conditions at the Start of the New Millennium. 2003: Geneva,
Switzerland.
Yeung EW, Yeung SS (2003). Interventions for preventing lower limb soft-tissue
injuries in runners (Cochrane Review). The Cochrane Library, Issue 3. Oxford:
Updated Software.](https://image.slidesharecdn.com/thesis-130609031900-phpapp02/85/Thesis-369-320.jpg)
![- References - 41
Chapter four
Australian Health Ministers' Advisory Council, Australian Health Ministers'
Advisory Council. Standing Committee for Aboriginal and Torres Strait Islander
Health. (2002). Aboriginal and Torres Strait Islander health workforce National
Strategic Framework. [Canberra], Australian Health Ministers' Advisory Council:
ii, 21.
Guidelines for Chiropractic Quality Assurance and Practice Parameters (Mercy
Guidelines). Editors: Haldeman S, Chapman-Smith D, Petersen DM.
Consensus Conference Commissioned by the Congress of Chiropractic State
Associations. Mercy Conference Center, Burlingame, California, USA (1992).
Bolton JE (1999). Accuracy of recall of usual pain intensity in back pain
patients. Pain 83(3): 533-9.
Bolton JE, Breen AC (1999). The Bournemouth Questionnaire: a short-form
comprehensive outcome measure. I. Psychometric properties in back pain
patients. J Manipulative Physiol Ther 22(8): 503-10.
Canadian Chiropractic Association (1993). Clinical Guidelines for Chiropractic
Practice in Canada. Editors: Henderson D, Chapman-Smith D, Silvano M,
Vernon H. Proceedings of a Consensus Conference Commissioned by the
Canadian Chiropractic Association. Glenerin Inn, Mississauga, Ontario,
Canada.
Cardiel MH (1993). Rheumatic diseases in Mexico: Validation of the
ILAR/COPCORD core questionnaire against physical exam. XVIII ILAR
Congress of Rheumatology, Barcelona, Spain, Published in: Rev Esp.
Rheumatol, Vol 20, Supp 1.](https://image.slidesharecdn.com/thesis-130609031900-phpapp02/85/Thesis-370-320.jpg)




![- References - 46
Australian Bureau of Statistics. (1998b). Experimental estimates of the
Aboriginal and Torres Strait Islander population, 30 June 1991 - 30 June 1996.
[Canberra], Australian Bureau of Statistics.
Australian Health Ministers' Advisory Council., Australian Health Ministers'
Advisory Council, Standing Committee for Aboriginal and Torres Strait Islander
Health. (2002). Aboriginal and Torres Strait Islander health workforce National
Strategic Framework. [Canberra], Australian Health Ministers' Advisory Council.
Australian Institute of Health and Welfare (1992). Australia’s Health 1992. The
Third Biennial Report of the Australian Institute of Health and Welfare.
Canberra, Australian Government Publishing Service.
Australian Institute of Health and Welfare. (2002a). Australia's Health 2002 : the
eighth biennial health report of the Australian Institute of Health and Welfare.
Canberra, Australian Institute of Health and Welfare.
Australian Institute of Health and Welfare (2002b). Health system costs of
injury, poisoning and musculoskeletal disorders in Australia 1993-94. Available
at: www.aihw.gov.au (Accessed July 29, 2003). Canberra, Australian
Government Publishing Service.
Becker N, Bondegaard Thomsen A, Olsen AK, et al. (1997). Pain epidemiology
and health related quality of life in chronic non-malignant pain patients referred
to a Danish multidisciplinary pain center. Pain 73(3): 393-400.
Bolton JE (1999). Accuracy of recall of usual pain intensity in back pain
patients. Pain 83(3): 533-9.
Bolton JE, Breen AC (1999). The Bournemouth Questionnaire: a short-form
comprehensive outcome measure. I. Psychometric properties in back pain
patients. J Manipulative Physiol Ther 22(8): 503-10.](https://image.slidesharecdn.com/thesis-130609031900-phpapp02/85/Thesis-375-320.jpg)








![- References - 55
Chapter six
Aboriginal Healthinfonet. Available at: www.healthinfonet.ecu.edu.au
(Accessed: July 30, 2003).
Australian Health Ministers' Advisory Council, Australian Health Ministers'
Advisory Council. Standing Committee for Aboriginal and Torres Strait Islander
Health. (2002). Aboriginal and Torres Strait Islander health workforce National
Strategic Framework. [Canberra], Australian Health Ministers' Advisory Council:
ii, 21.
Australian National Training Authority (ANTA) Available at:
http://www.anta.gov.au/dapStrategies.asp (Accessed: February 10, 2002).
National Training Information Service (NTIS), Community Services and Health
Industry Council, Australian National Training Authority, 2002.
Available at: http://www.ntis.gov.au (Accessed: August 19, 2004).
Royal Commission into Aboriginal Deaths in Custody. Canberra: Australian
Government Publishing Service. (1992).
Training Revisions. National Review of Aboriginal and Torres Strait Islander
Health Worker Training. A report submitted to the Office for Aboriginal and
Torres Strait Islander Health. (2002). Curtin Indigenous Research Centre with
Centre for Education Research and Evaluation Consortium and Jojara &
Associates.
Browell T (2003). Founder and Principal, Murray School of Health Education,
Established 1979. Echuca, Mildura, Victoria.
Buchanan N (2002). Listening and learning from each other. Interview with
Indigenous elder Uncle Neville Buchanan and Dein Vindigni, Booroongen
Djugun College, Kempsey, NSW. July 2002.](https://image.slidesharecdn.com/thesis-130609031900-phpapp02/85/Thesis-384-320.jpg)



![- References - 59
Chapter seven
Australian Health Ministers' Advisory Council, Australian Health Ministers'
Advisory Council. Standing Committee for Aboriginal and Torres Strait Islander
Health. (2002). Aboriginal and Torres Strait Islander health workforce National
Strategic Framework. [Canberra], Australian Health Ministers' Advisory Council.
Australian Institute of Health and Welfare. (2002). Australia's Health 2002 : the
eighth biennial health report of the Australian Institute of Health and Welfare.
Canberra, Australian Institute of Health and Welfare.
Bolton JE, Breen AC (1999). The Bournemouth Questionnaire: a short-form
comprehensive outcome measure. I. Psychometric properties in back pain
patients. J Manipulative Physiol Ther 22(8): 503-10.
Bolton JE (1999). Accuracy of recall of usual pain intensity in back pain
patients. Pain 83(3): 533-9.
Bourke C, Bourke E, Edwards B, (Eds) (2003). Aboriginal Australia. An
Introductory reader in Aboriginal Studies. Queensland. University of
Queensland Press.
Darmawan J, Valkenburg HA, Muirden KD, Wigley RD (1992). Epidemiology of
rheumatic diseases in rural and urban populations in Indonesia: a World Health
Organisation International League Against Rheumatism COPCORD study,
stage I, phase 2. Annals of the Rheumatic Diseases. 51(4): 525-8.
Davis G, Wanna J, Warhurst J, Weller P (1988). Public policy in Australia. Allen
and Unwin, Sydney.](https://image.slidesharecdn.com/thesis-130609031900-phpapp02/85/Thesis-388-320.jpg)













































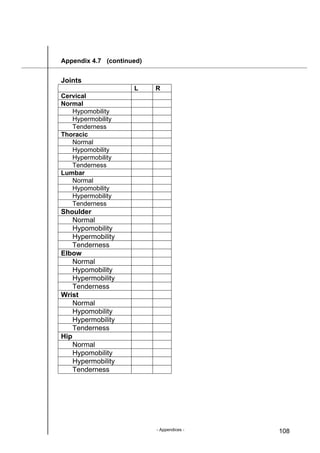
![- Appendices - 105
Appendix 4.7 Participant Assessment Form (revised)
Participant Assessment Form (revised)
Kempsey Pilot Program
Survey date: ____/____/____ Investigator/s: ______________________
Name/code number: _______________
Date of Birth: ____/____/____
Gender: _______
Height: _______ [cm]
Weight: _______ [Kg
Occupation:
Yes No
Aged pensioner
Disability pensioner
Management
CDEP students
TAFE & High School
Health worker
Home duties
Labourers
Clerical
Professional
Other
Marital status:
Yes No
Married
De-facto
Separated
Divorced
Widowed
Never married
Number of children: _______](https://image.slidesharecdn.com/thesis-130609031900-phpapp02/85/Thesis-434-320.jpg)
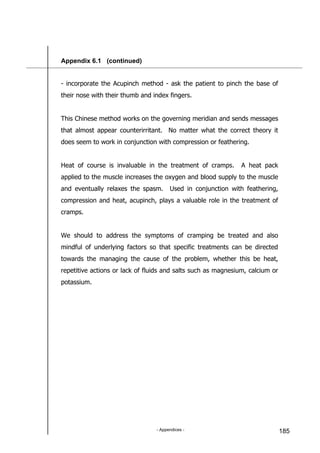
![- Appendices - 106
Appendix 4.7 (continued)
Vital signs
Blood pressure: _______ [mmHg]
Pulse rate: ___________ [bpm]
Respiration rate: _______ [rpm]
Temperature: _________ [°C]
Musculoskeletal Assessment
Inspection
Posture
Yes No
Forward head carriage
Normal thoracic kyphosis
Increased thoracic kyphosis
Decreased thoracic kyphosis
Normal lumbar lordosis
Increased lumbar lordosis
Decreased lumbar lordosis
Scoliosis
Yes No
Cervical
Thoracic
Lumbar
Joint abnormalities
Yes No
Swelling
Reddening
Thickening
Location (of joint abnormalities)](https://image.slidesharecdn.com/thesis-130609031900-phpapp02/85/Thesis-435-320.jpg)


















































































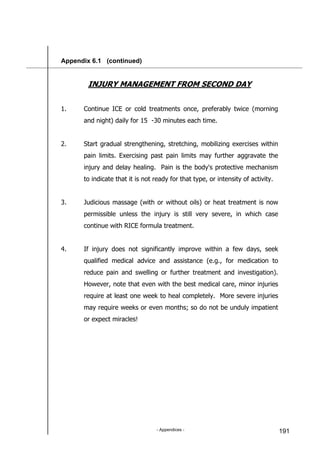

























![- Appendices - 217
Appendix 6.1 (continued)
Hopbush, sticky hopbush (common name)
(botanical name: Sapindaceae)
Hopbush is one if the more well-documented indigenous medical herbs.
Details of numerous traditional uses have been accumulated from four
continents including Australia.
Family: Sapindaceae
Description: Erect evergreen shrubs 5m high, may be
monoecious or dioecious. Leaves linear-lanceolate,
narrowly tapered at apex base, entire margins,
glabrous, petiolate, 6-13cm long, 5-10mm wide.
Flowers appear in Spring on pedicels 3-9mm long
arranged in terminal panicles. Sepals 3-4 petals
absent. Capsules, winged with a glabours surface,
cover the plant during summer [Harden, 1991].
Distribution: Dodonea viscose is widespread in Eastern
Australia, and also found in parts of Asia, Africa
and Central America. The subspecies angustifolia
occurs in the Americas, the Asia-Pacific region and
from tropical to southern Africa [Ghisalberti 1998]
as well as eastern Australia where it grows chiefly
on slopes and tablelands in dry sclerophyll forest
or woodland.
Part used: Leaves, aerial parts, roots
Traditional Uses: Hopbush was used by Aborigines in the form of a
root decoction for cuts and open wounds. Leaves
were chewed as a painkiller and used for
toothache. Boiled root juice was applied for
headache [Isaacs, 1987]. In India a tincture](https://image.slidesharecdn.com/thesis-130609031900-phpapp02/85/Thesis-546-320.jpg)
![- Appendices - 218
Appendix 6.1 (continued)
was taken internally for gout, rheumatism and
fevers. A poultice of leaves was applied to
painful swellings and rheumatic joints. In Mexico
various preparations were used to treat
inflammation, swellings and pain.
Actions: Spasmolytic anti-inflammatory, andoyne.
Pharmacy research: The spasmolytic effects displayed by D.viscose
were equal to that Datura lanosa, and standard
anticholinergic, a calcium channel blocking
mechanism. Anti-inflammatory and anti-oxidant
activity.
Reasearch: Dr. Sean Cox from the Centre for Biomolecular
University of Western Sydney is currently
investigating the antiinflammatory and
antioxidant activity using samples of my 1.4
dried tincture of Dodonaea ssp. Angustifolia leaf.
This data is unpublished.
Indications: Gout rheumatism, inflammatory disorder,
toothache and applied to painful stings [Isaacs,
1987]](https://image.slidesharecdn.com/thesis-130609031900-phpapp02/85/Thesis-547-320.jpg)
























