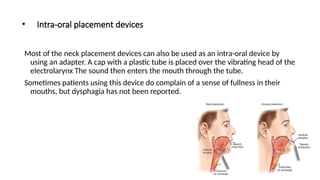
The document discusses speech options for patients post-laryngectomy, including esophageal speech, electrolarynx speech, and tracheoesophageal (TE) speech. It outlines the mechanics of each method, the benefits and drawbacks, particularly focusing on the use of voice prostheses and their management. Common complications and the rehabilitation process for voice restoration are also addressed.