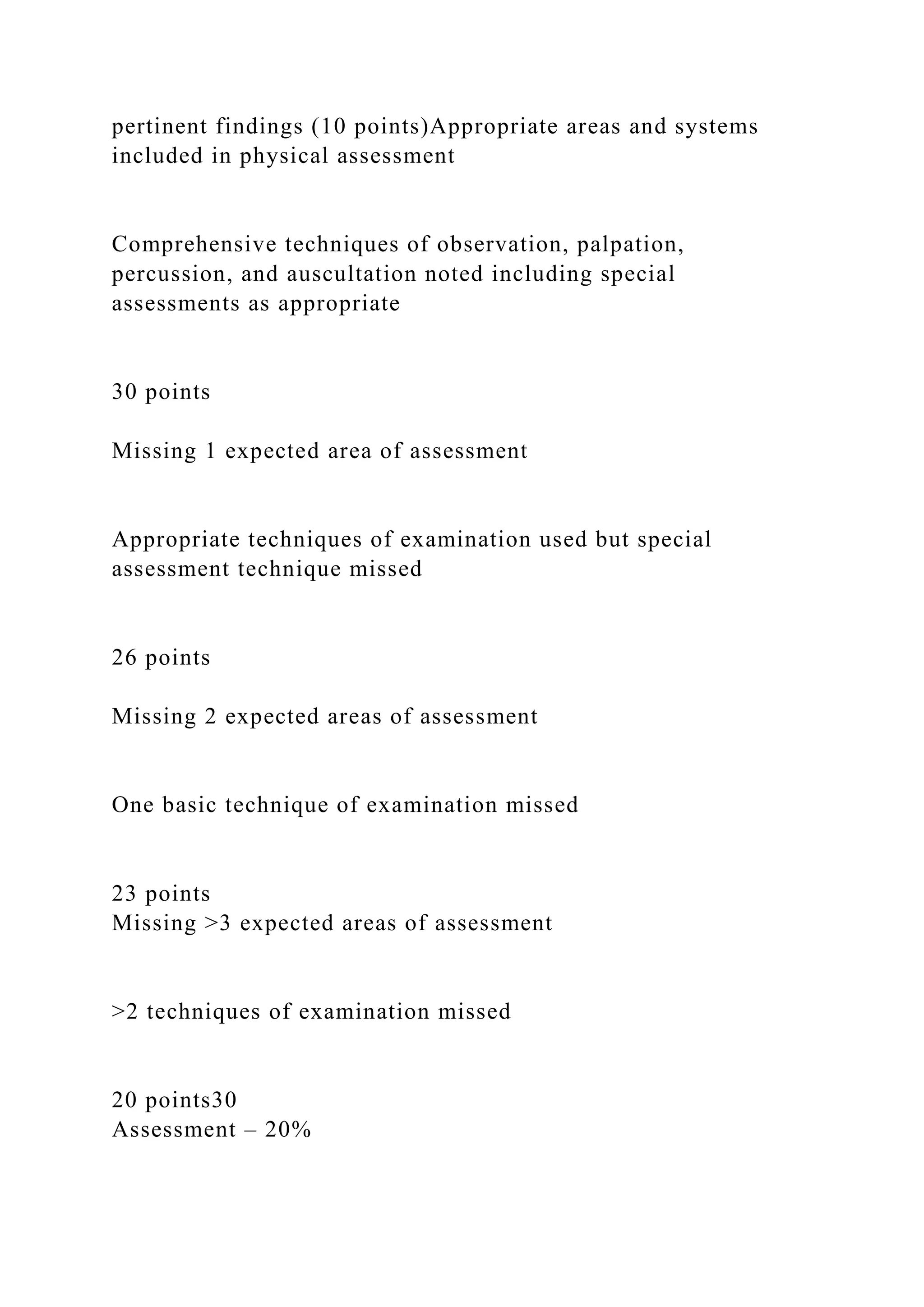
This document provides a rubric for evaluating a SOAP note assignment on gastritis. The SOAP note should include the following sections:
1) Subjective: Patient description, chief complaint, history of present illness, review of focus systems, medications, and health history.
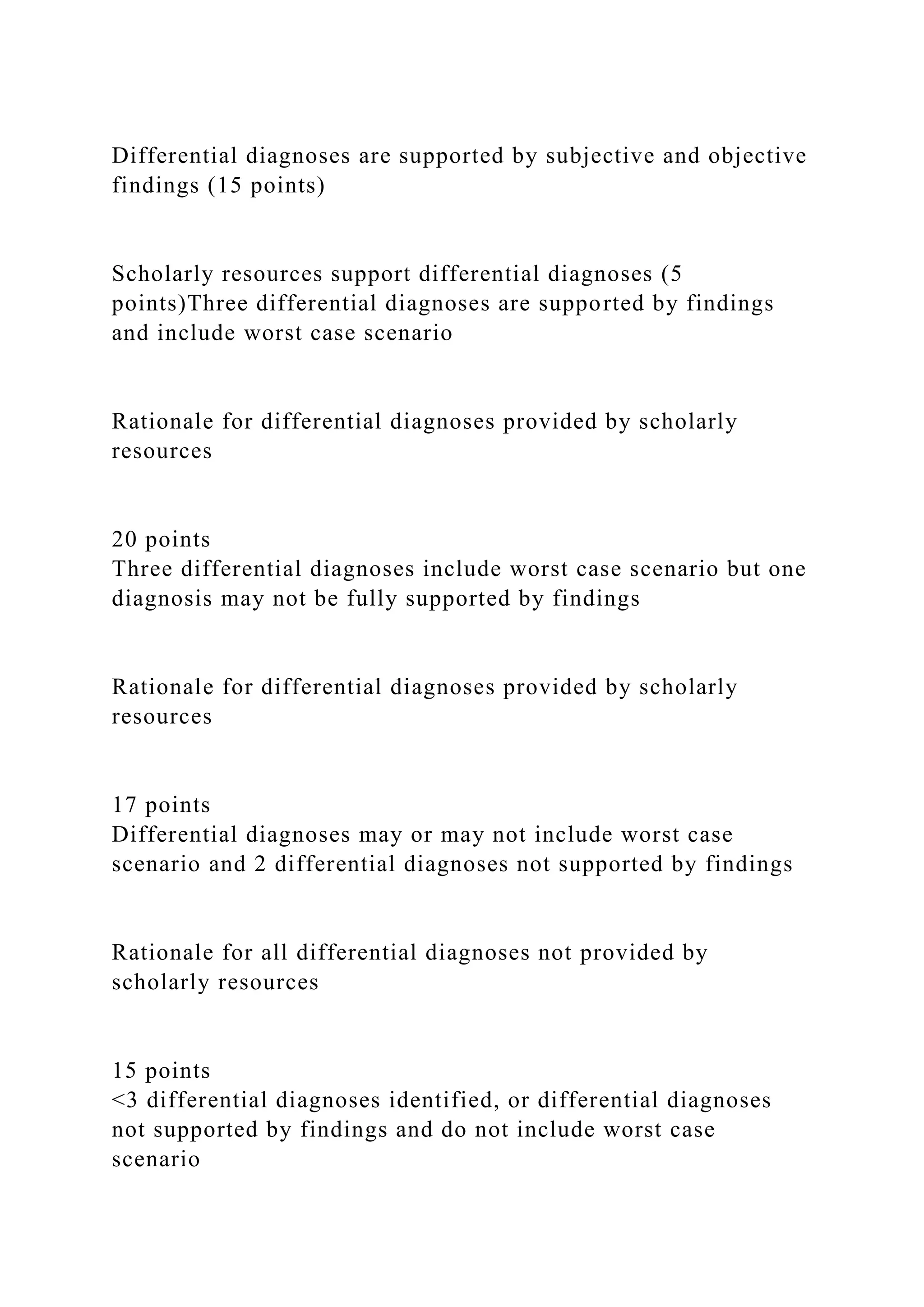
2) Objective: Physical exam findings relevant to the chief complaint and systems review. Appropriate examination techniques should be documented.
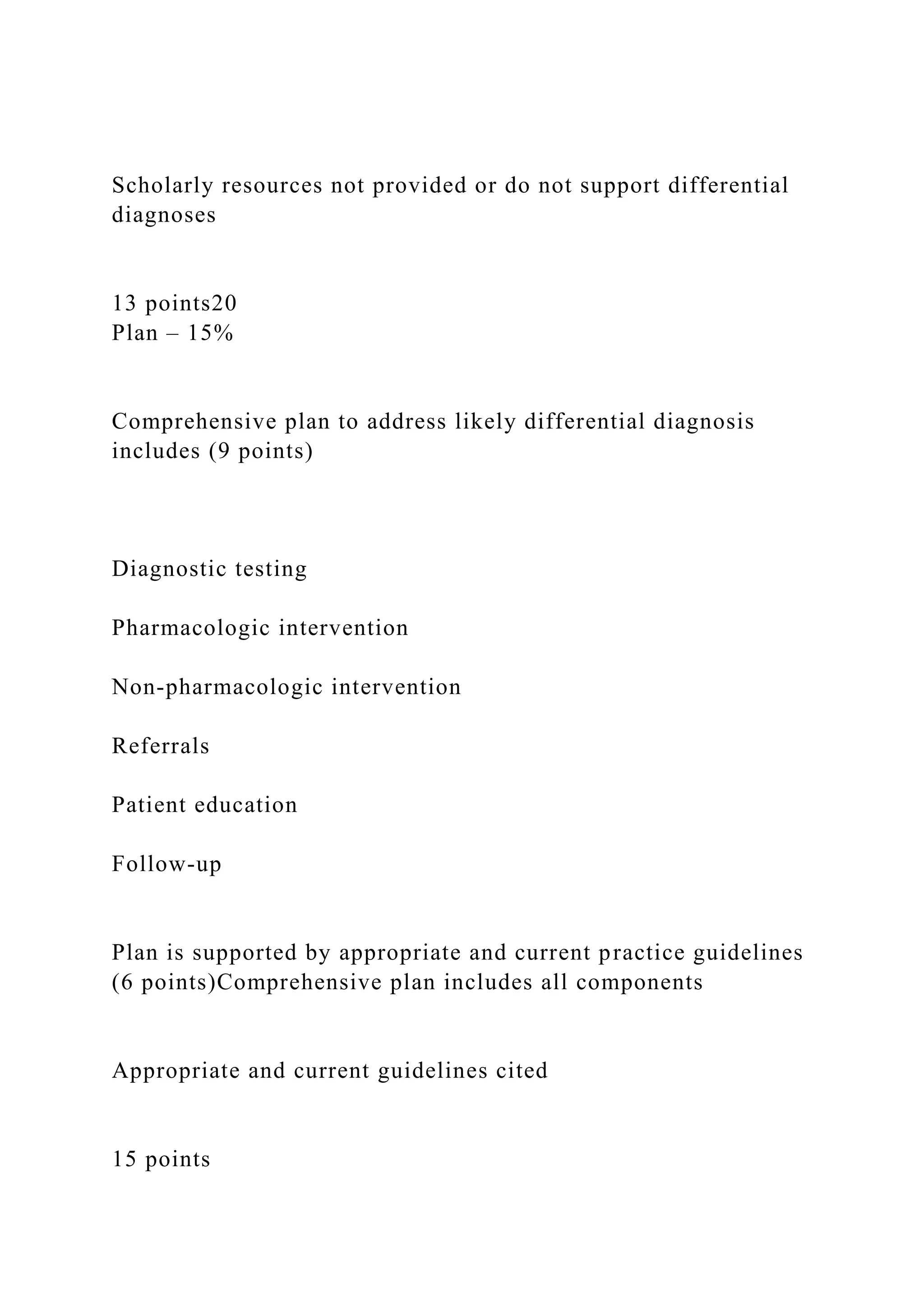
3) Assessment: Differential diagnoses supported by subjective and objective findings. Scholarly resources should support the differentials.
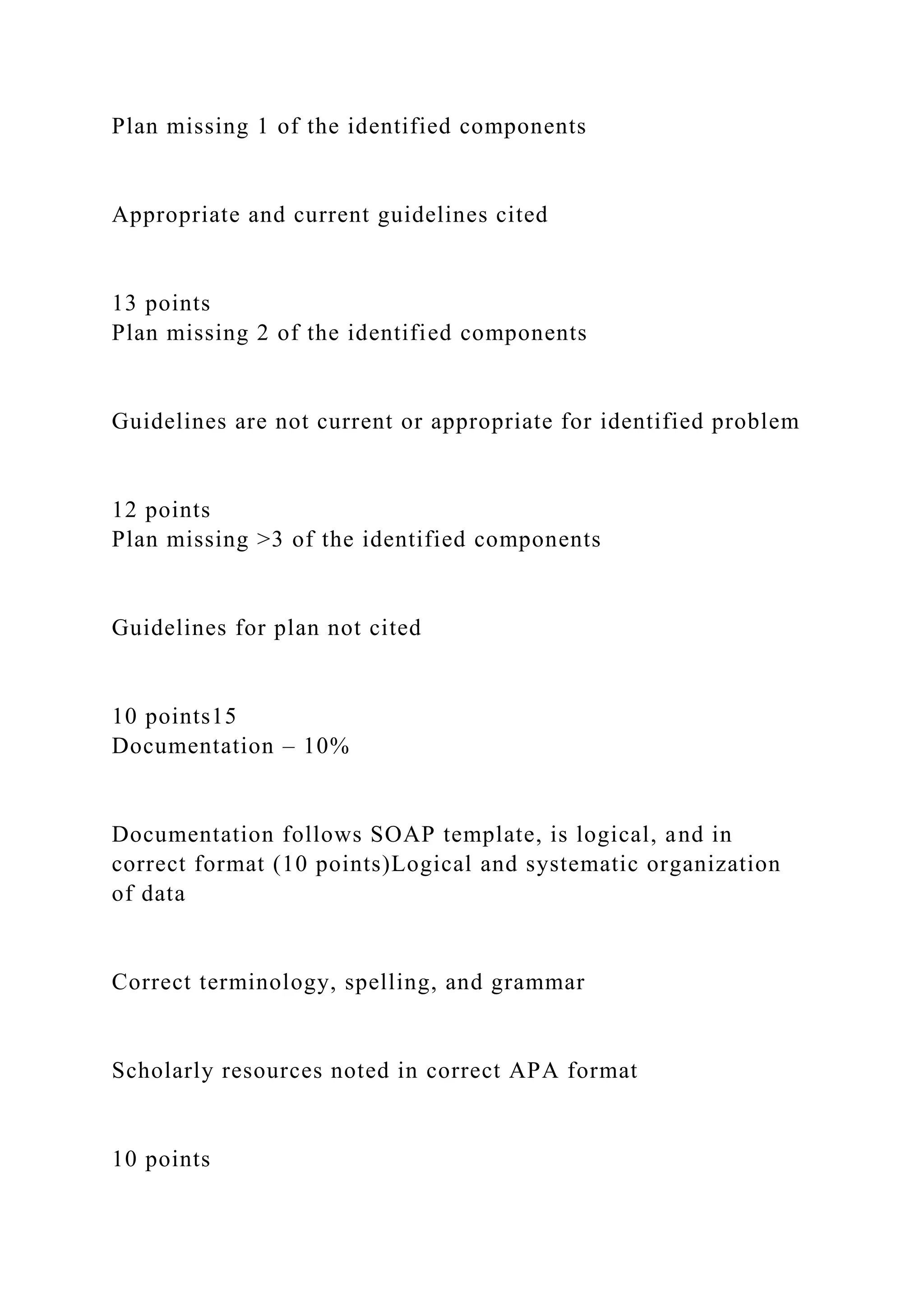
4) Plan: Comprehensive treatment plan including testing, medications, referrals, education and follow up. The plan should be supported by current guidelines.
![SOAP NOTE- GASTRITIS
The goal of this assignment is to practice writing a SOAP Note
for a sick or episodic visit related to the focus system(s)
reviewed in the previous week’s learning materials.--
GASTRITIS . Review the SOAP Note Rubric. Use a case from
the previous week’s discussion or patient from your video
submission or clinical practicum experience (adding content as
needed to represent abnormal findings). Submit your own note.
Do not submit documentation from the patient’s record.
RUBRIC
SOAP Note Rubric
[SOAP Note Rubric] – 100 PointsCriteriaExemplary
Exceeds ExpectationsAdvanced
Meets ExpectationsIntermediate
Needs ImprovementNovice
InadequateTotal Points
Subjective – 25%
Information about the patient (3 points)](https://image.slidesharecdn.com/soapnote-gastritisthegoalofthisassignmentistopracti-230117174910-2ec40f03/75/SOAP-NOTE-GASTRITISThe-goal-of-this-assignment-is-to-practi-docx-1-2048.jpg)