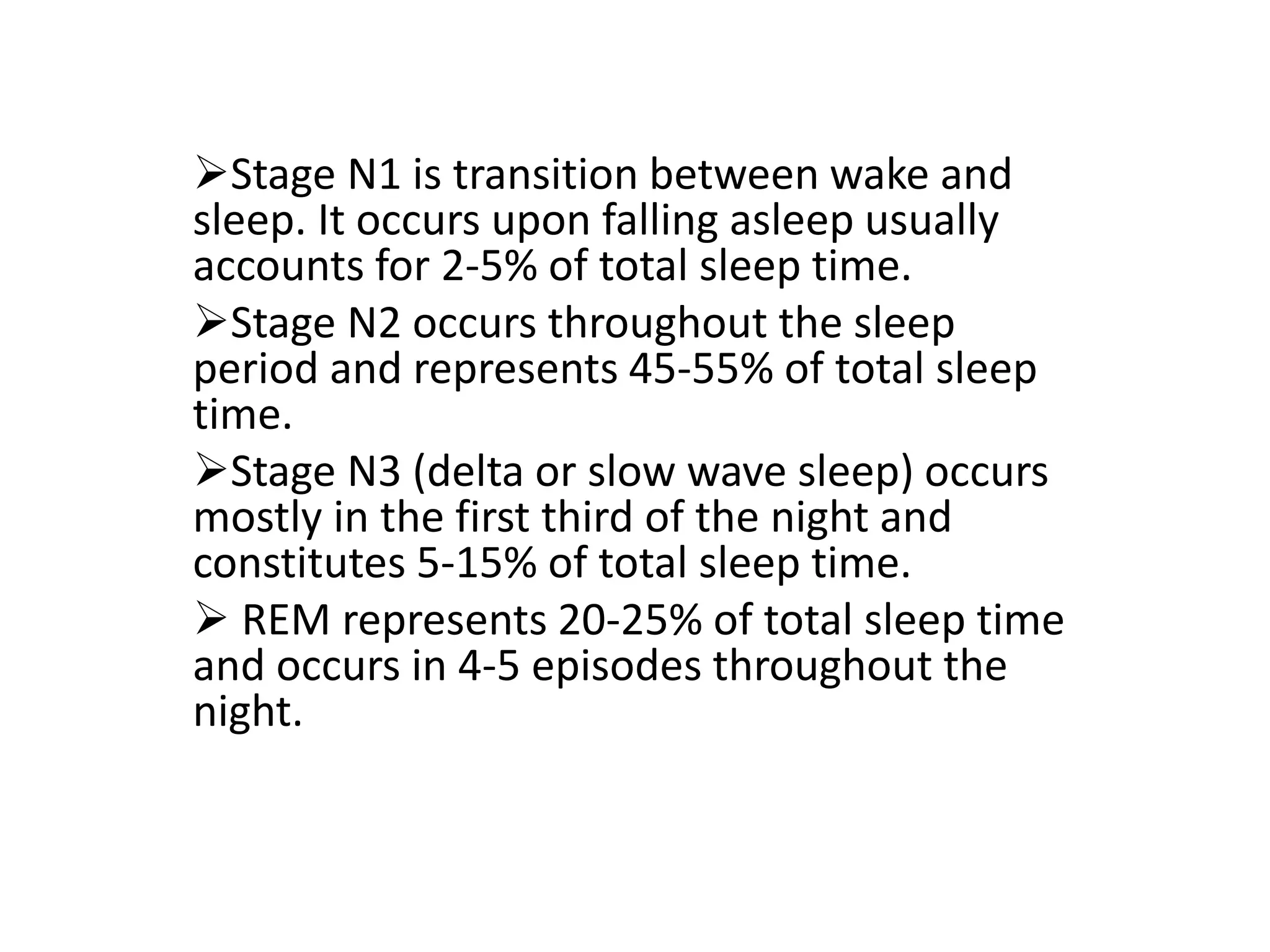
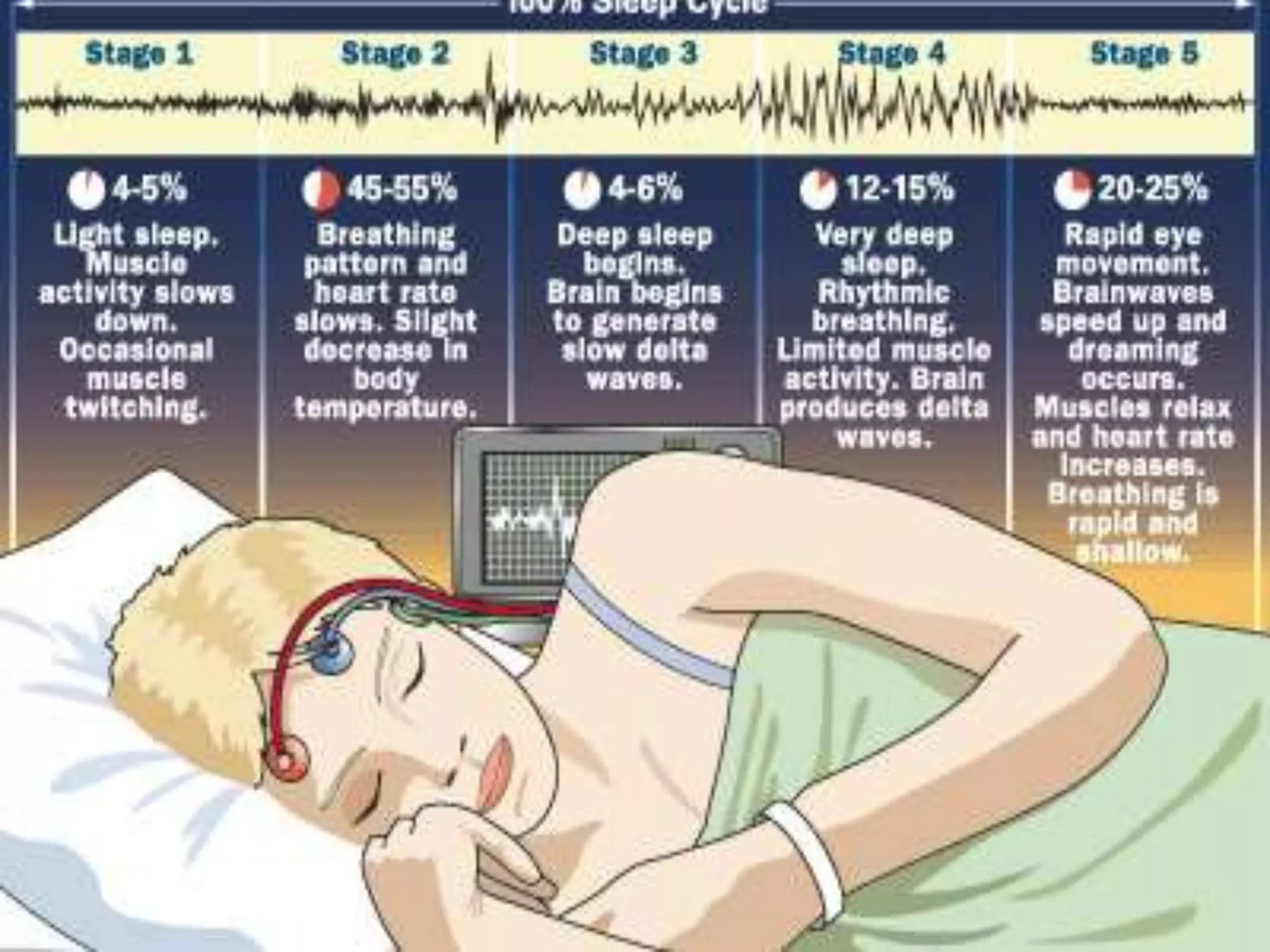
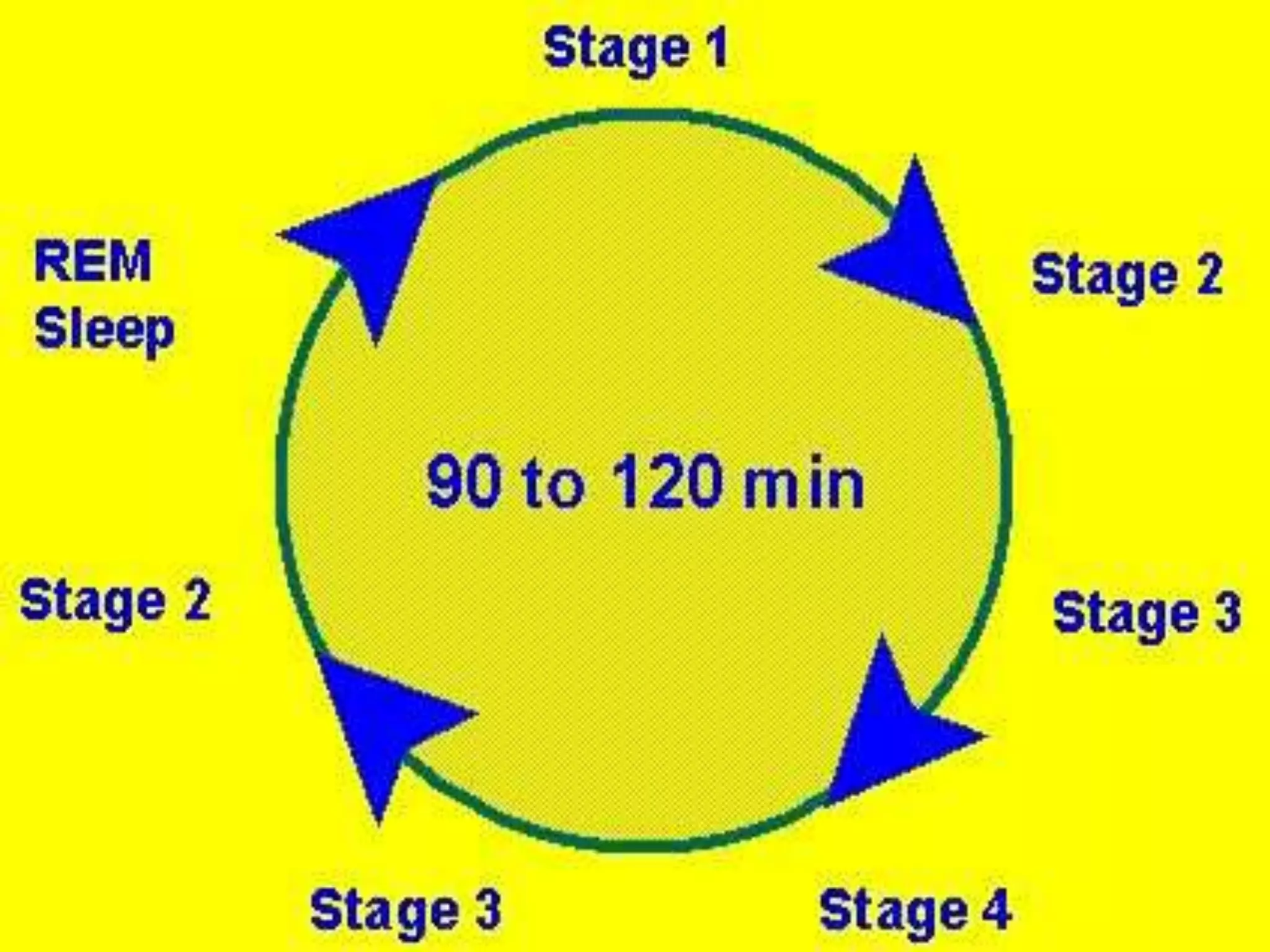
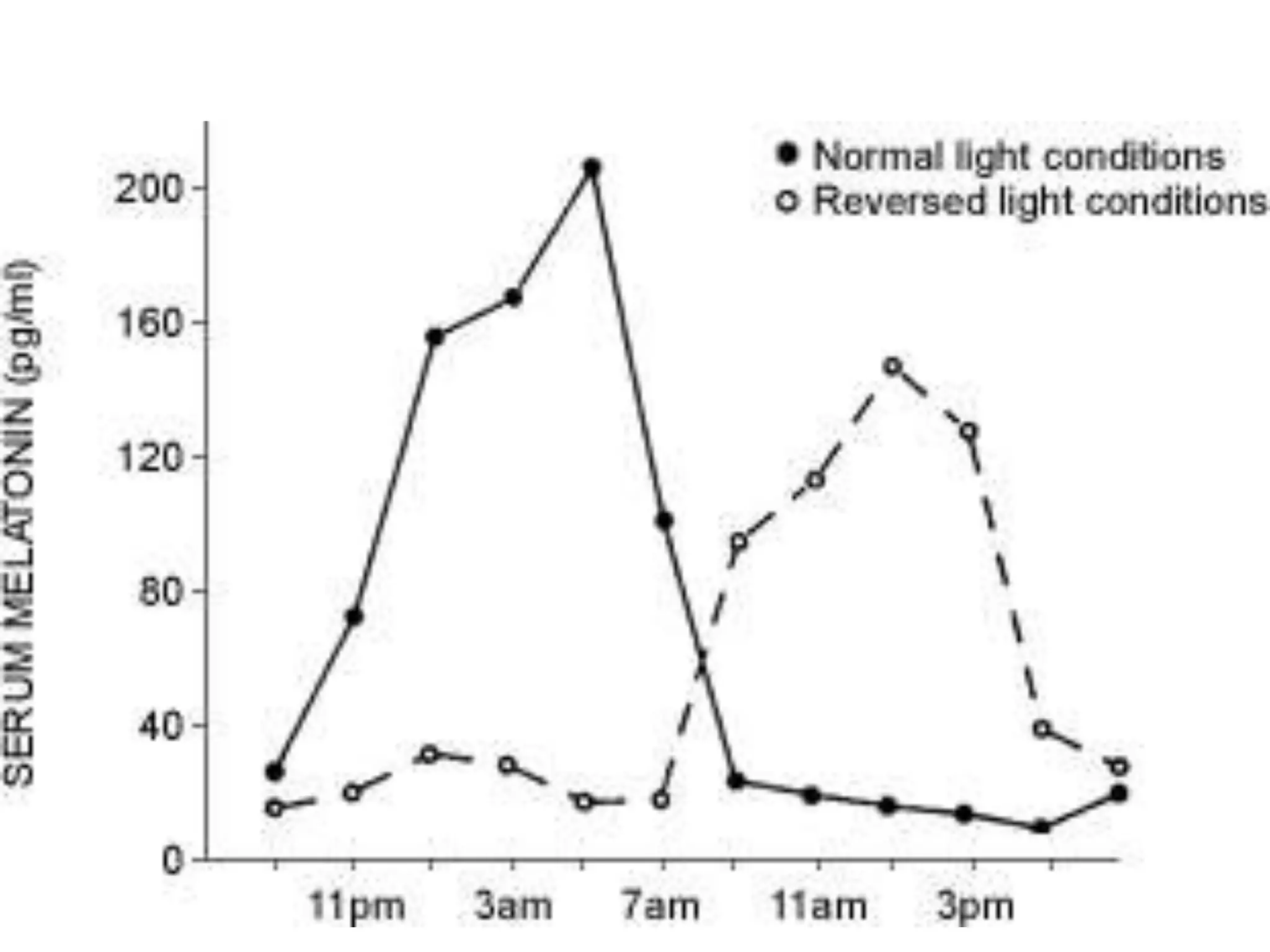
The document discusses the neurology of sleep. It describes the two main types of sleep - NREM and REM sleep. NREM sleep involves synchronous cortical EEG, low muscle tone, and minimal dreaming. REM sleep is characterized by rapid eye movements, muscle atonia, and vivid dreaming. The document also discusses circadian rhythms and how the suprachiasmatic nucleus regulates sleep-wake cycles. Disruptions to circadian rhythms can lead to sleep disorders like jet lag.














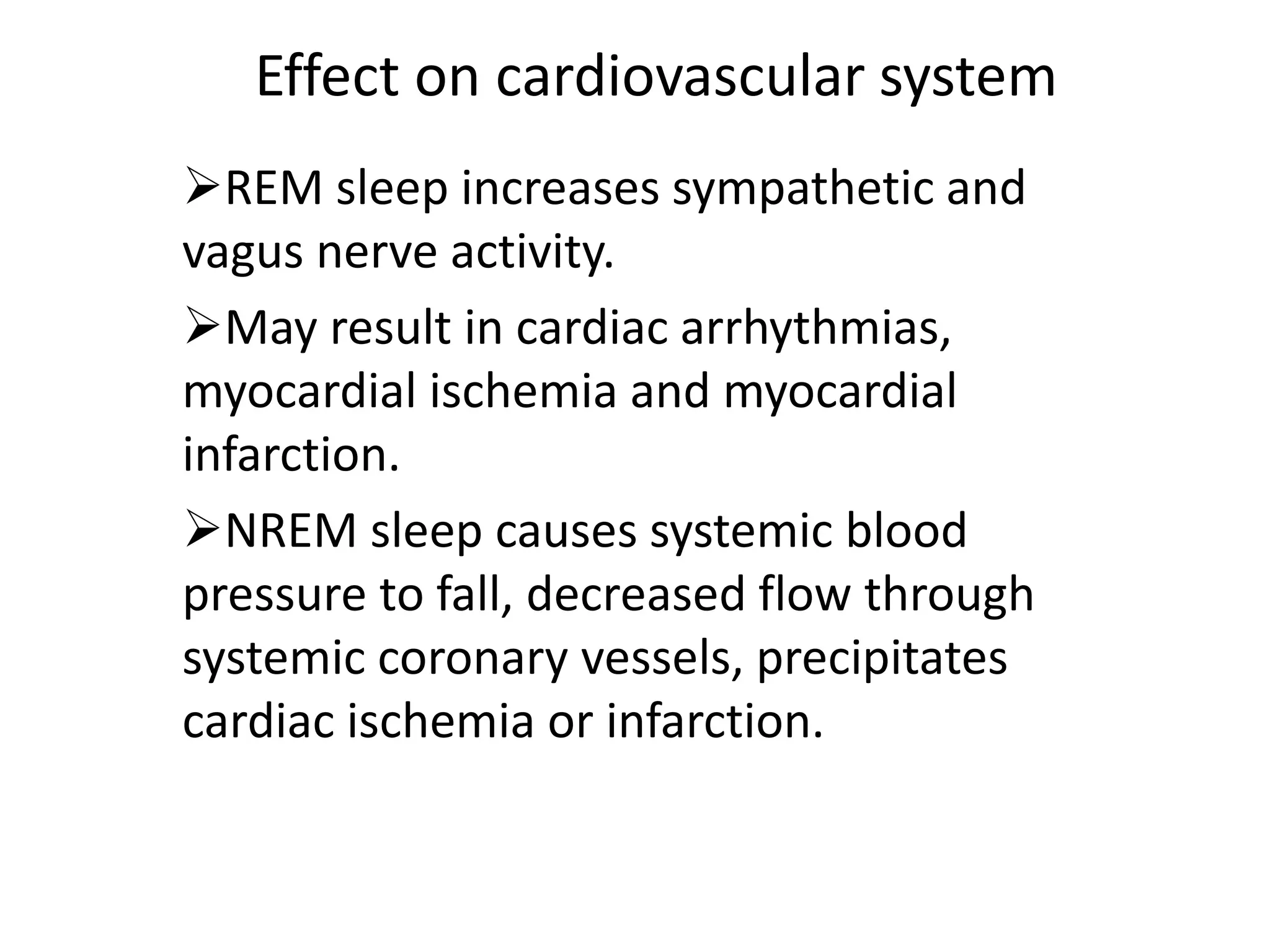











![Treatment options
Behavioural and light therapy are the mainstays of
treatment of circadian rhythm disturbances.
Timed bright light therapy: bright room light over
time may be sufficient; however, a higher intensity of
light (>6000 lux over 30-60 min) is often necessary to
accomplish acute phase shifts.
Light therapy applied in the early evening and night
time delays the cycle in patients with advanced sleep-
phase syndrome [ASPS]), early morning stimulates
morning alertness and an earlier bedtime in patients
with delayed sleep-phase syndrome [DSPS].
Chronotherapy: This behavioural treatment consists
of a gradual shift in sleep time in accordance with the
patient's tendency.](https://image.slidesharecdn.com/sleep1-230222184731-a6013da0/75/SLEEP1-ppt-42-2048.jpg)

