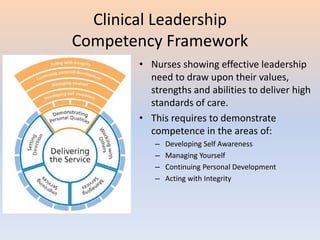
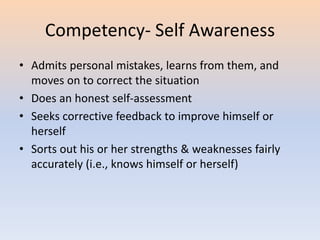
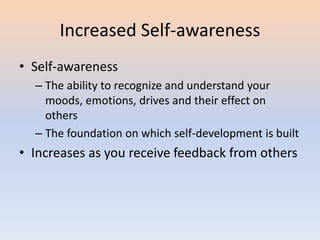
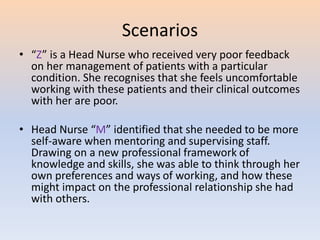
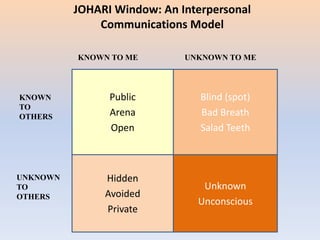
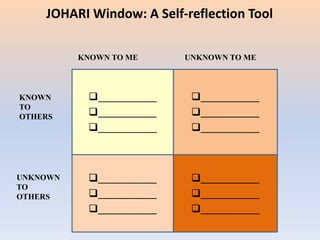
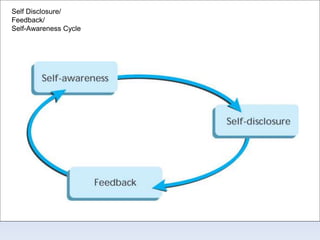
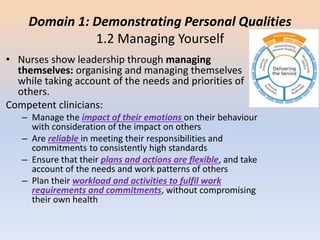
This document discusses leadership in nursing. It begins by explaining that front-line nurse leaders are essential to healthcare organizations but are often promoted due to technical skills rather than leadership abilities. As many as 40% of new supervisors fail due to a lack of training. Historically, nursing has focused on a task-oriented model rather than vision and relationships. The document then introduces the Clinical Leadership Competency Framework, which is built on shared leadership. It describes the five core domains of this framework: demonstrating personal qualities, working with others, managing services, improving services, and setting direction. Specifically, it discusses developing self-awareness, managing yourself, continuing personal development, and acting with integrity under the domain of demonstrating personal qualities.