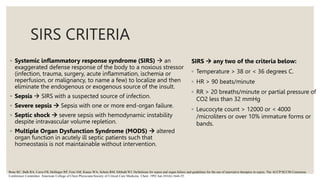
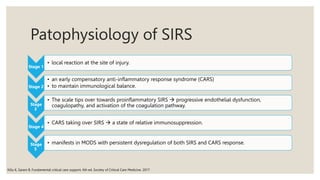
Sepsis is a life-threatening organ dysfunction caused by a dysregulated host response to infection. It can progress to septic shock, which is characterized by hypotension and elevated lactate levels. The document discusses definitions of sepsis, SIRS criteria, differences between recent sepsis guidelines, screening tools for sepsis, pathophysiology, management including initial resuscitation, hemodynamic support, antibiotics, ventilation, and additional treatments recommended by clinical practice guidelines.