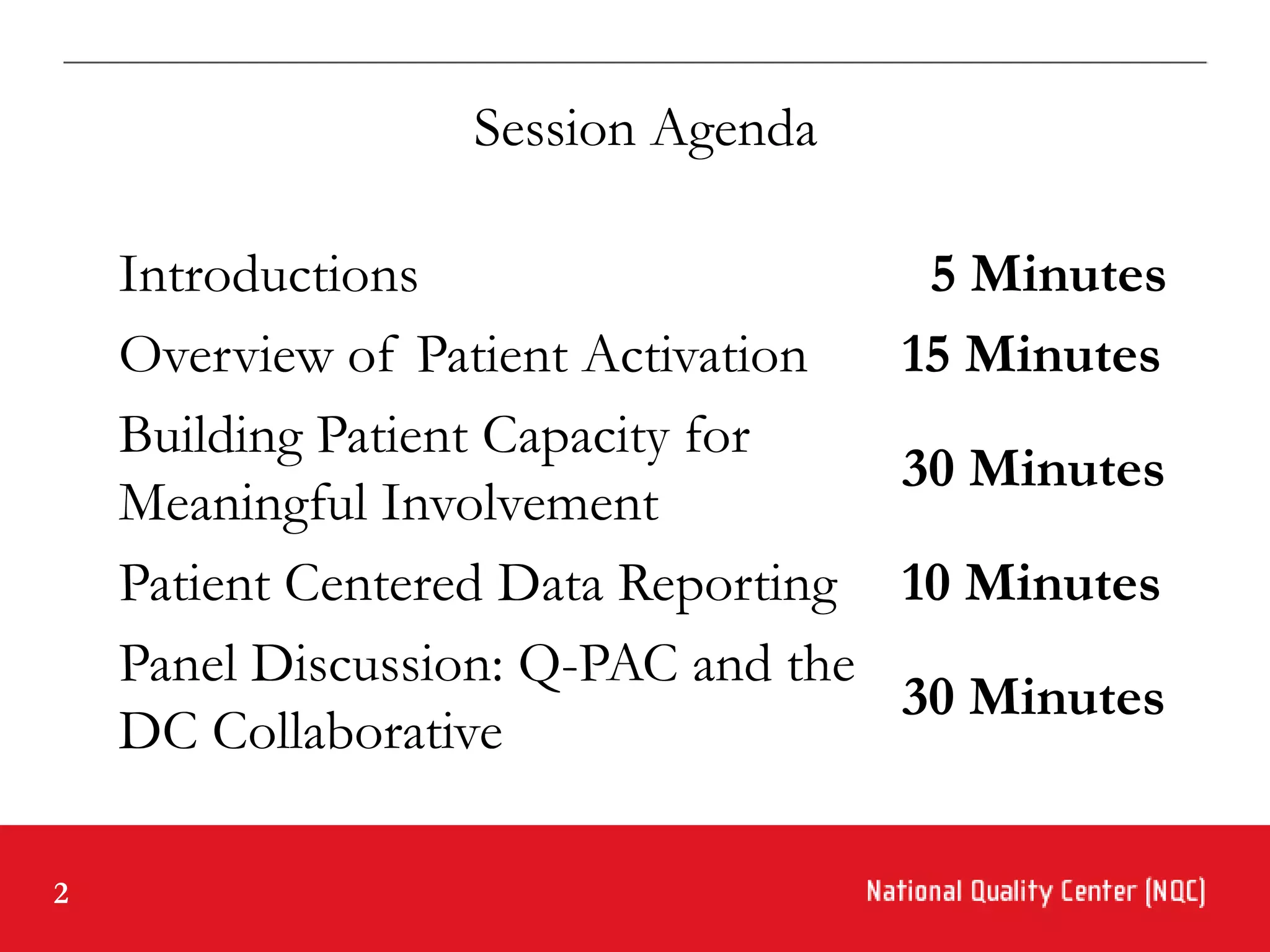
The document outlines an agenda for a session on introducing the Q-PAC model for patient activation and involvement in quality management. The agenda includes introductions, an overview of patient activation, building patient capacity, patient-centered data reporting, and a panel discussion. The objectives are to introduce patient activation as a method for improving consumer involvement, provide a model for consumer involvement, and discuss a framework for patient data in quality management.