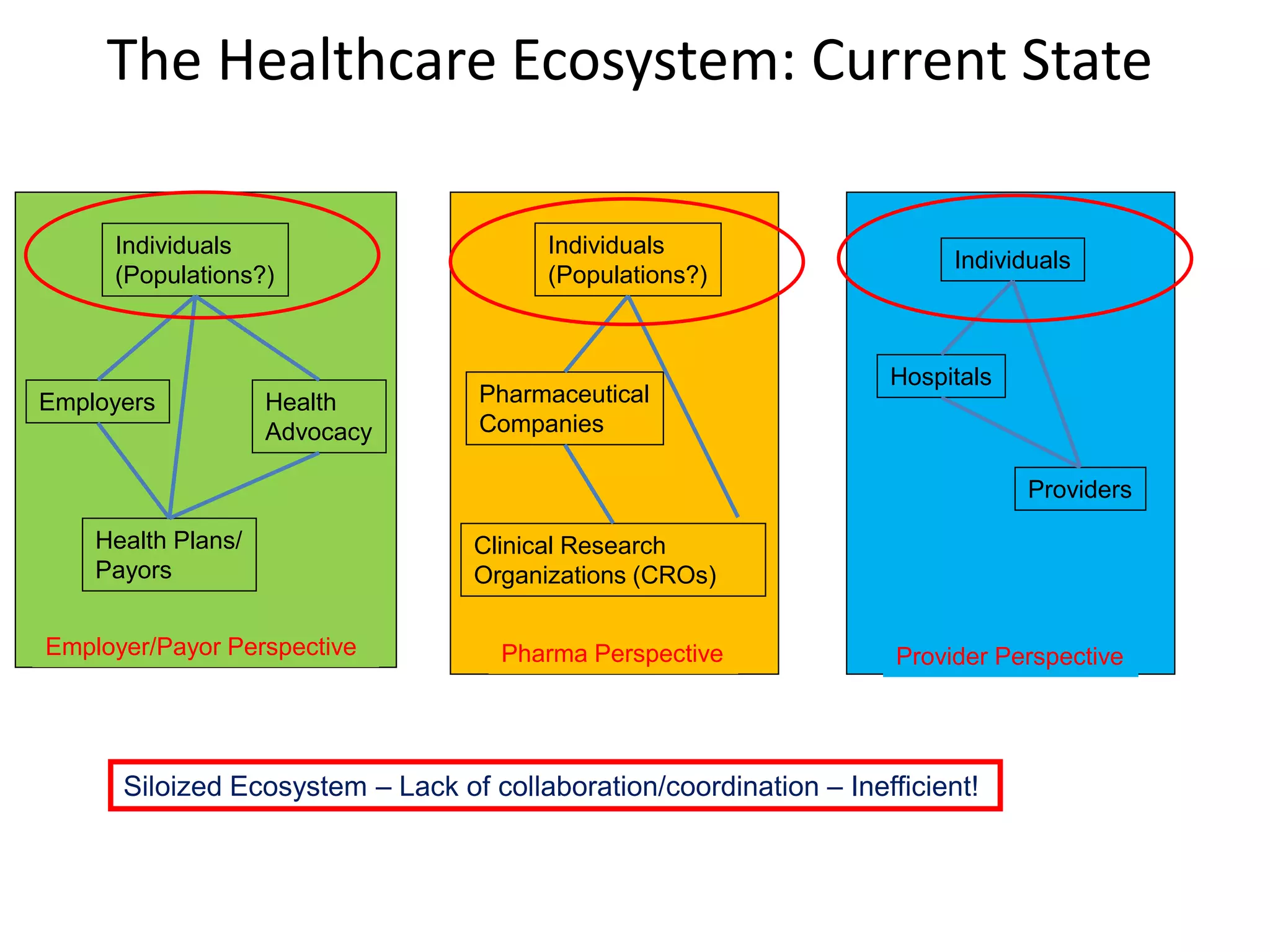
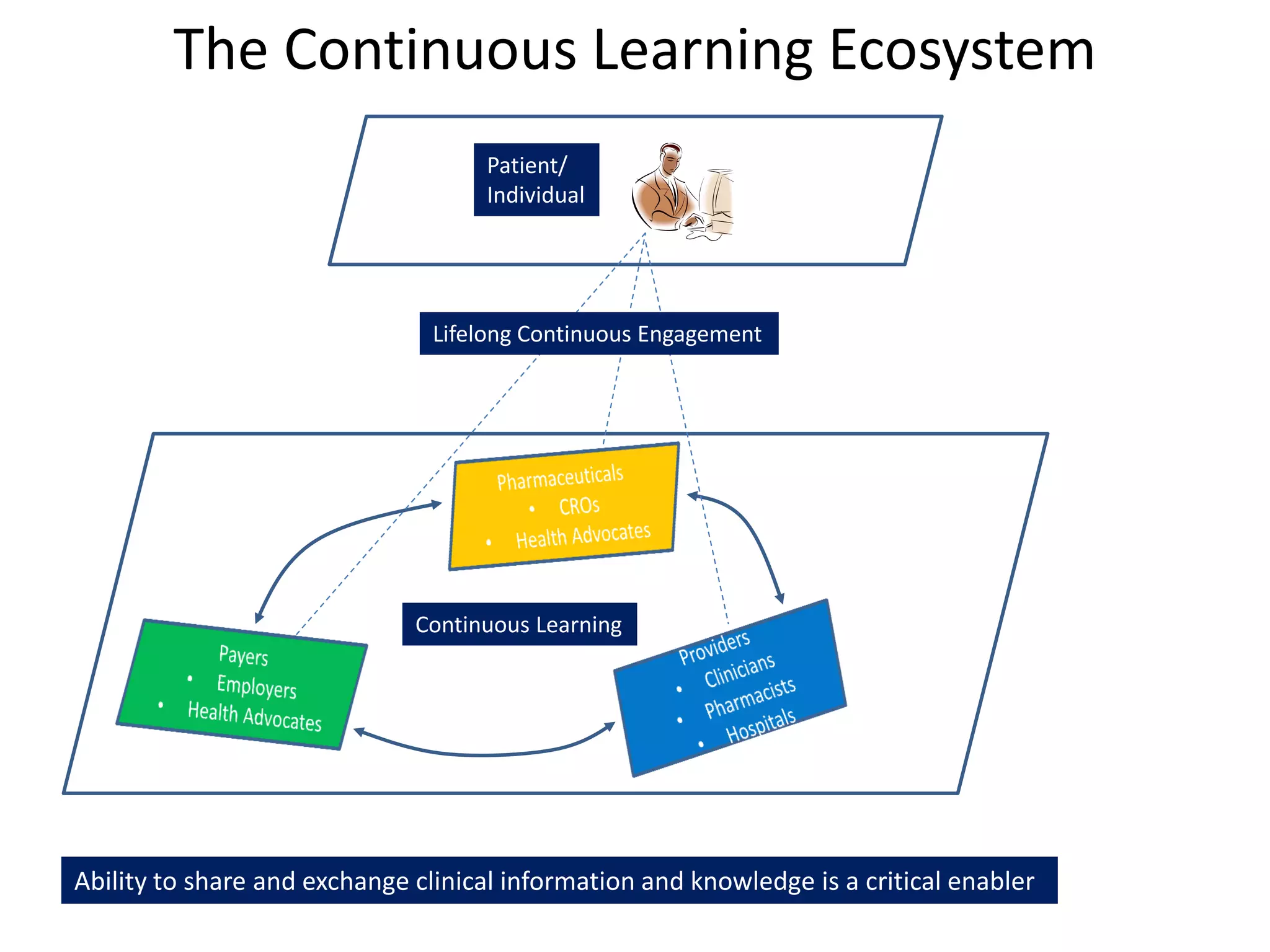
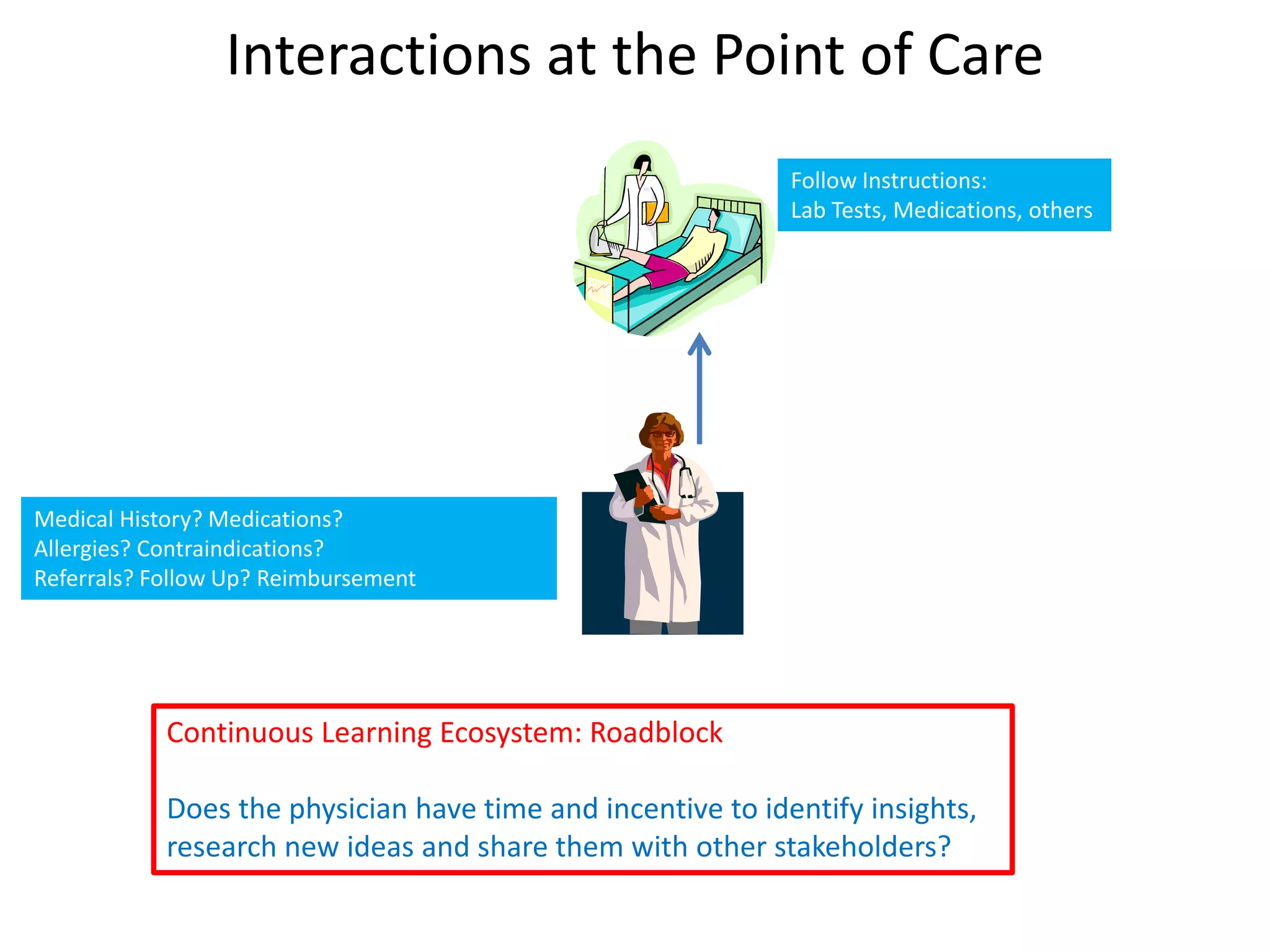
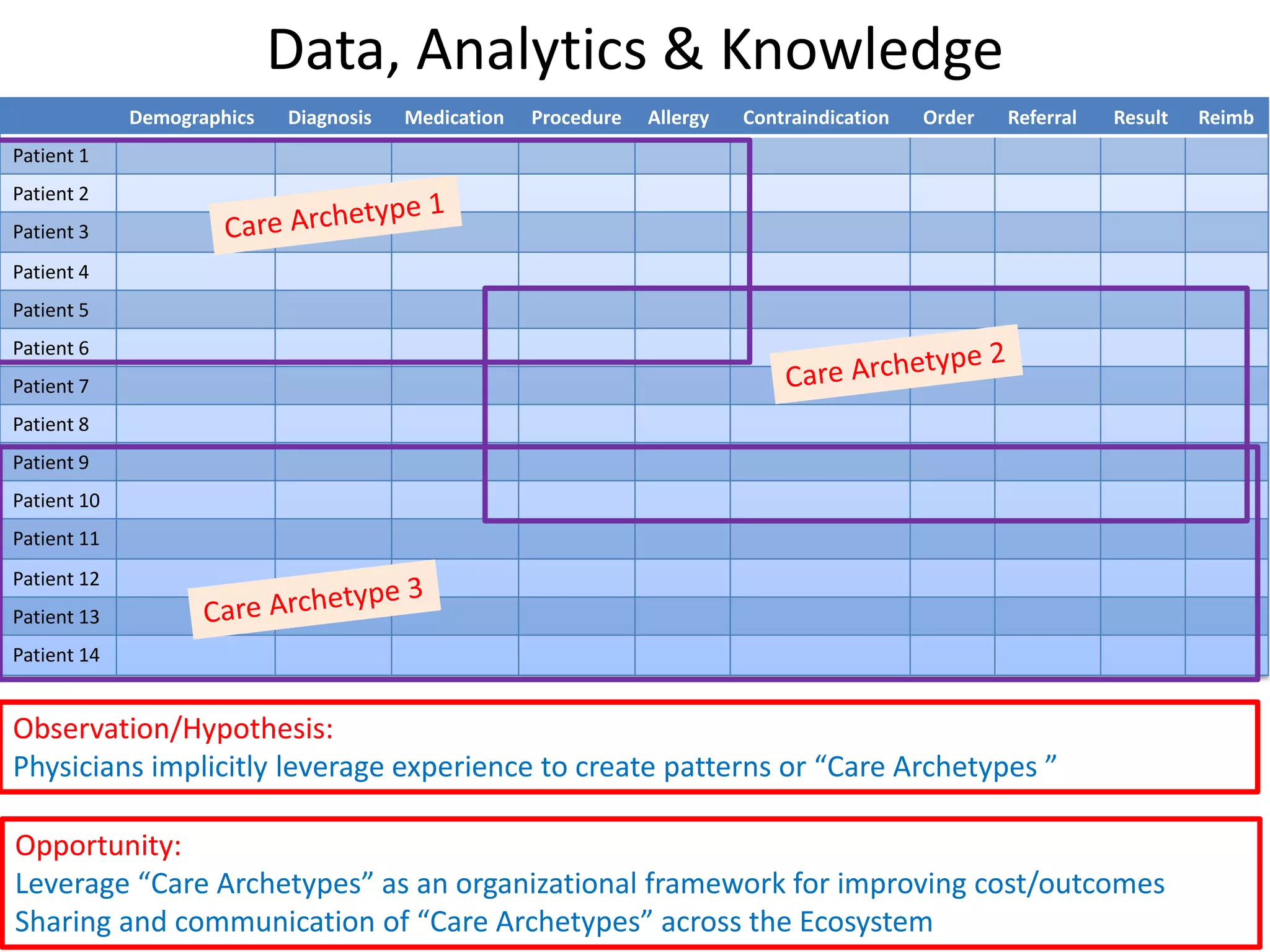
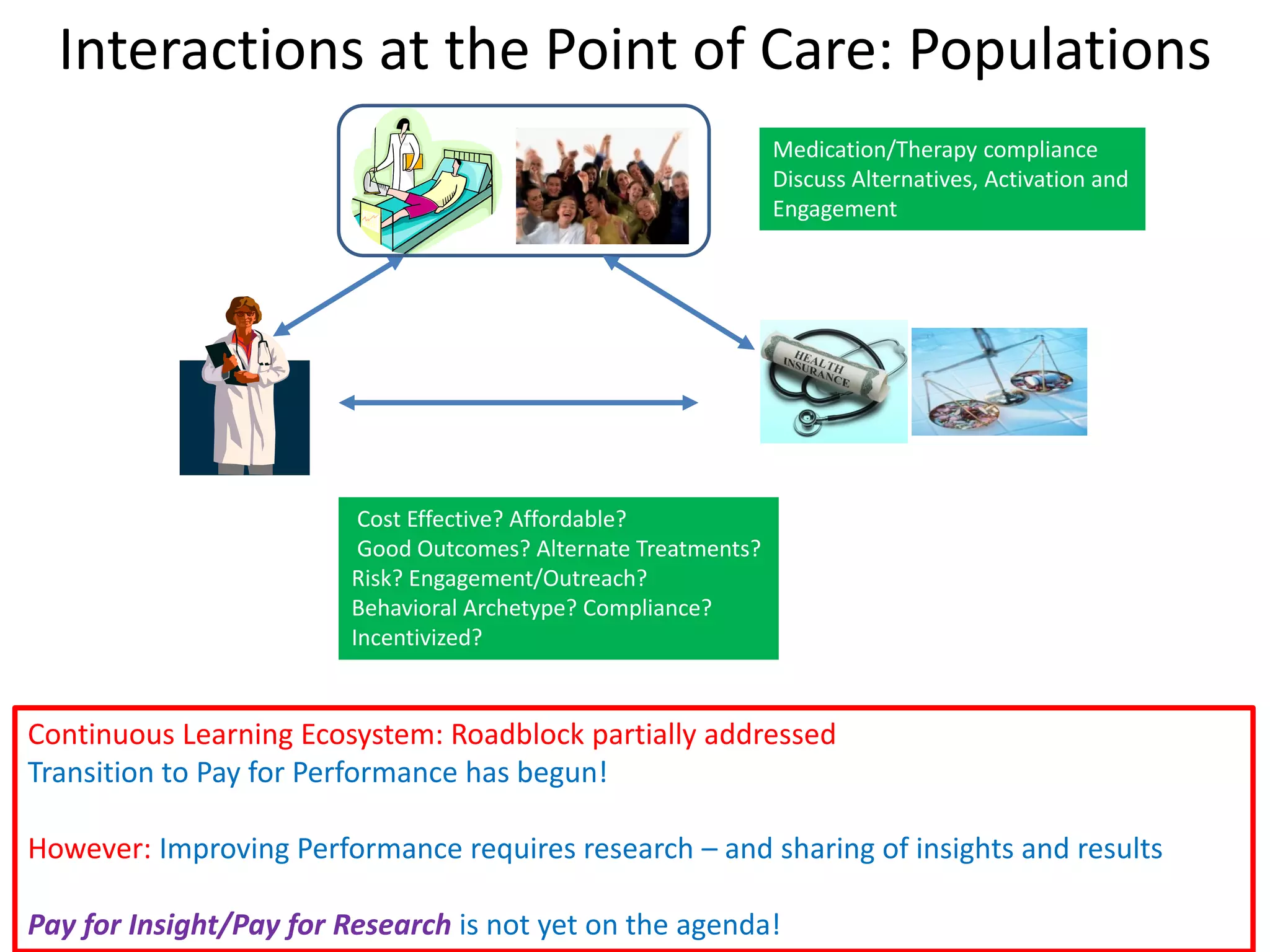
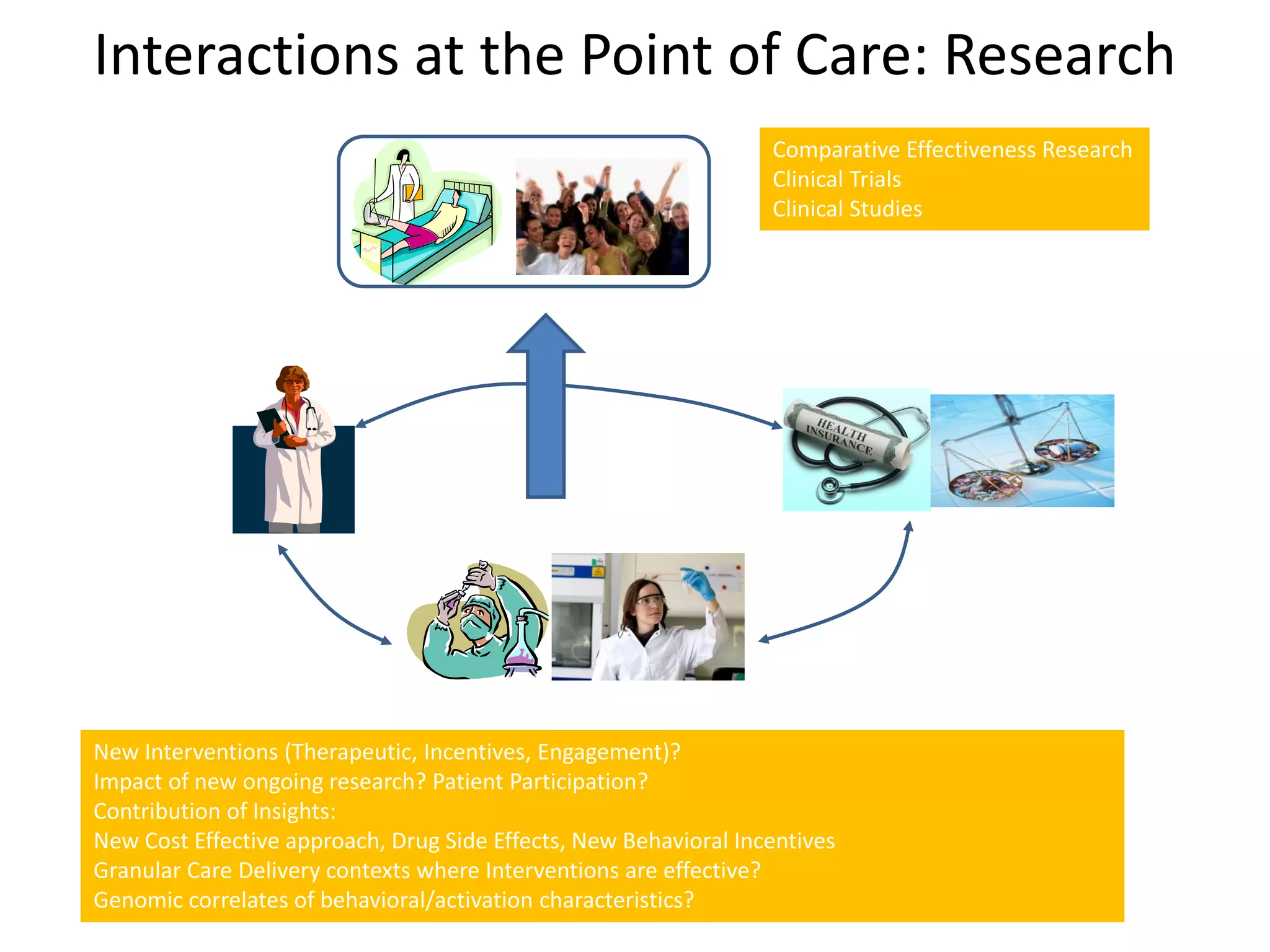
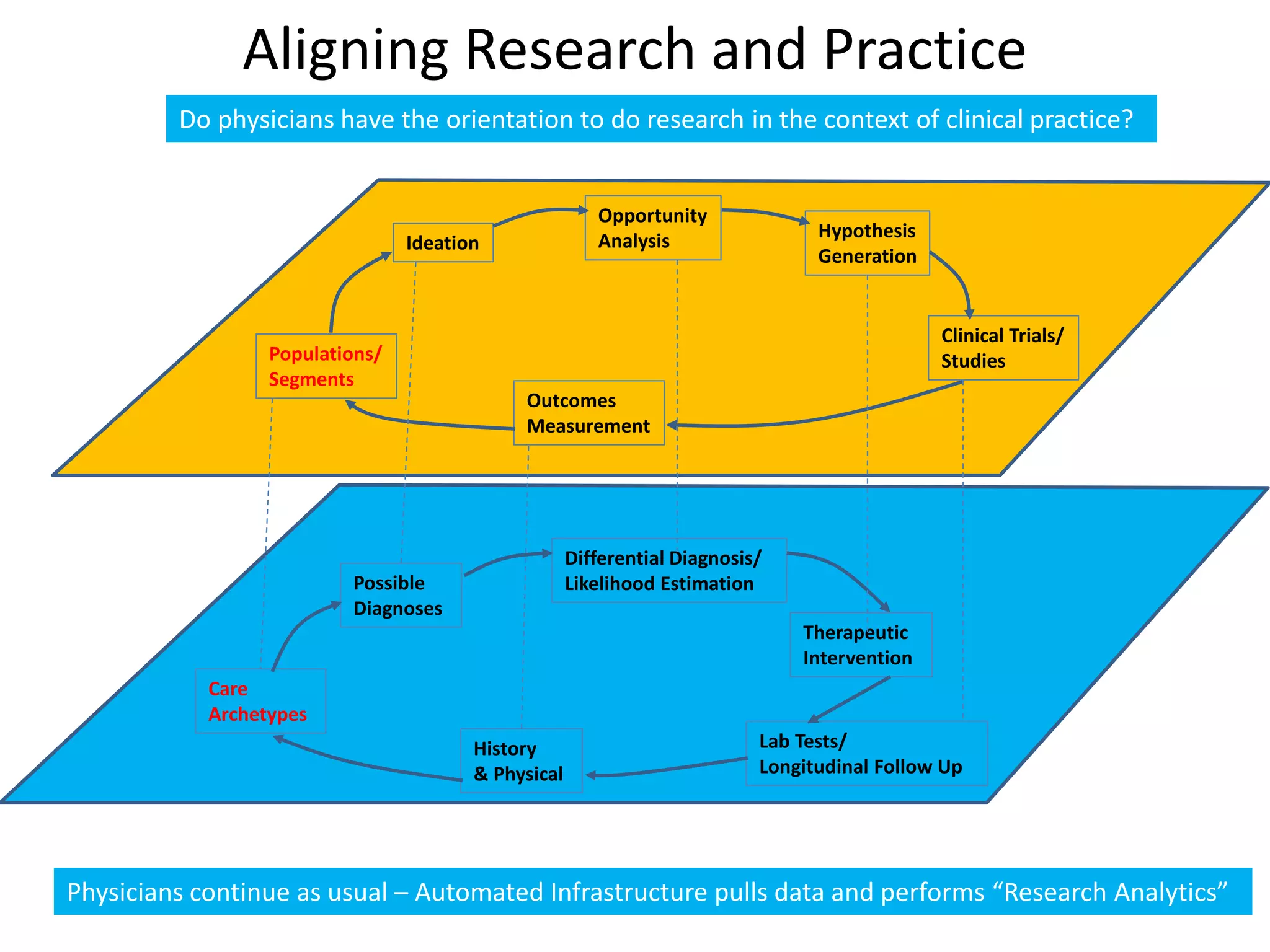
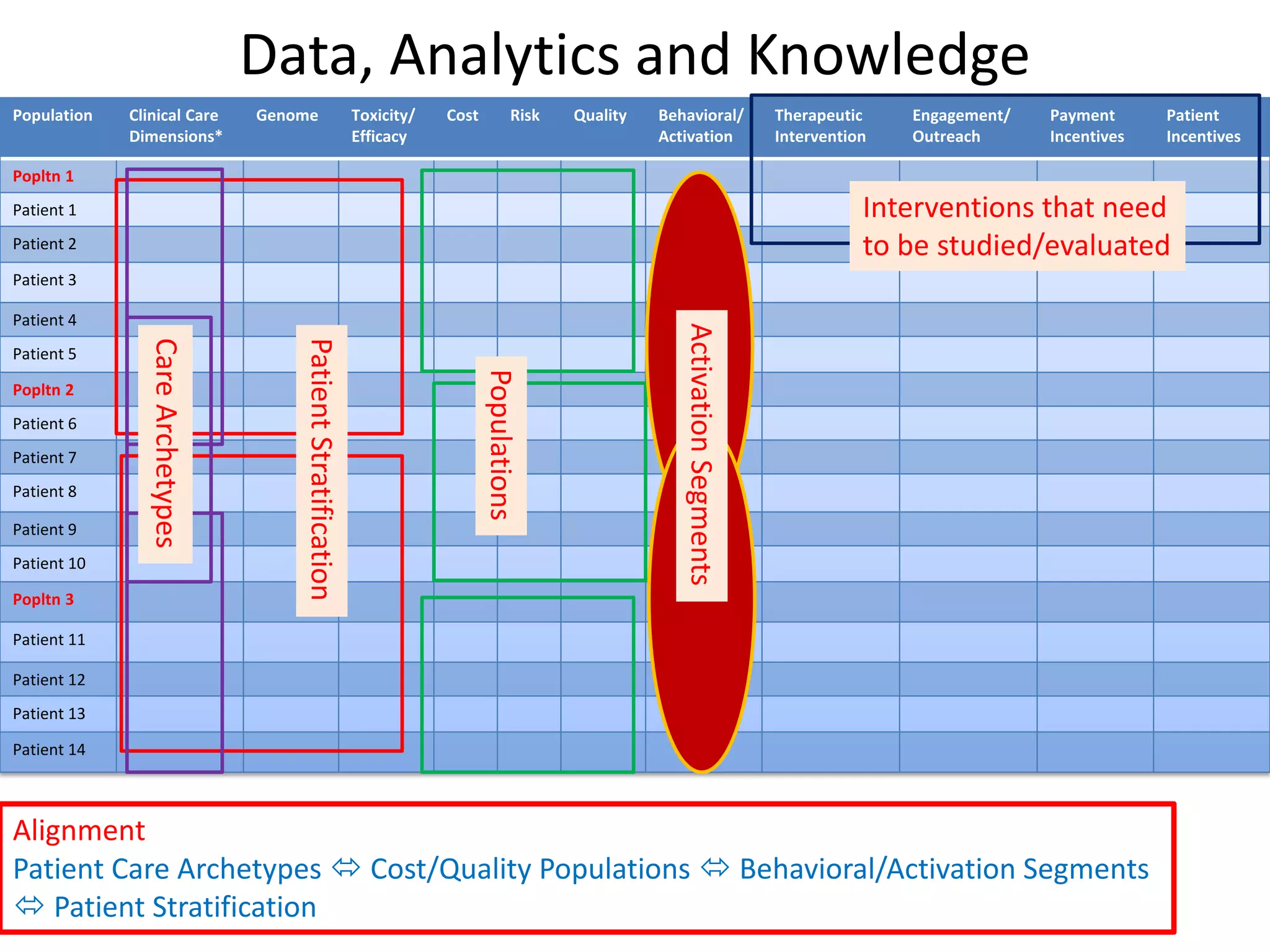
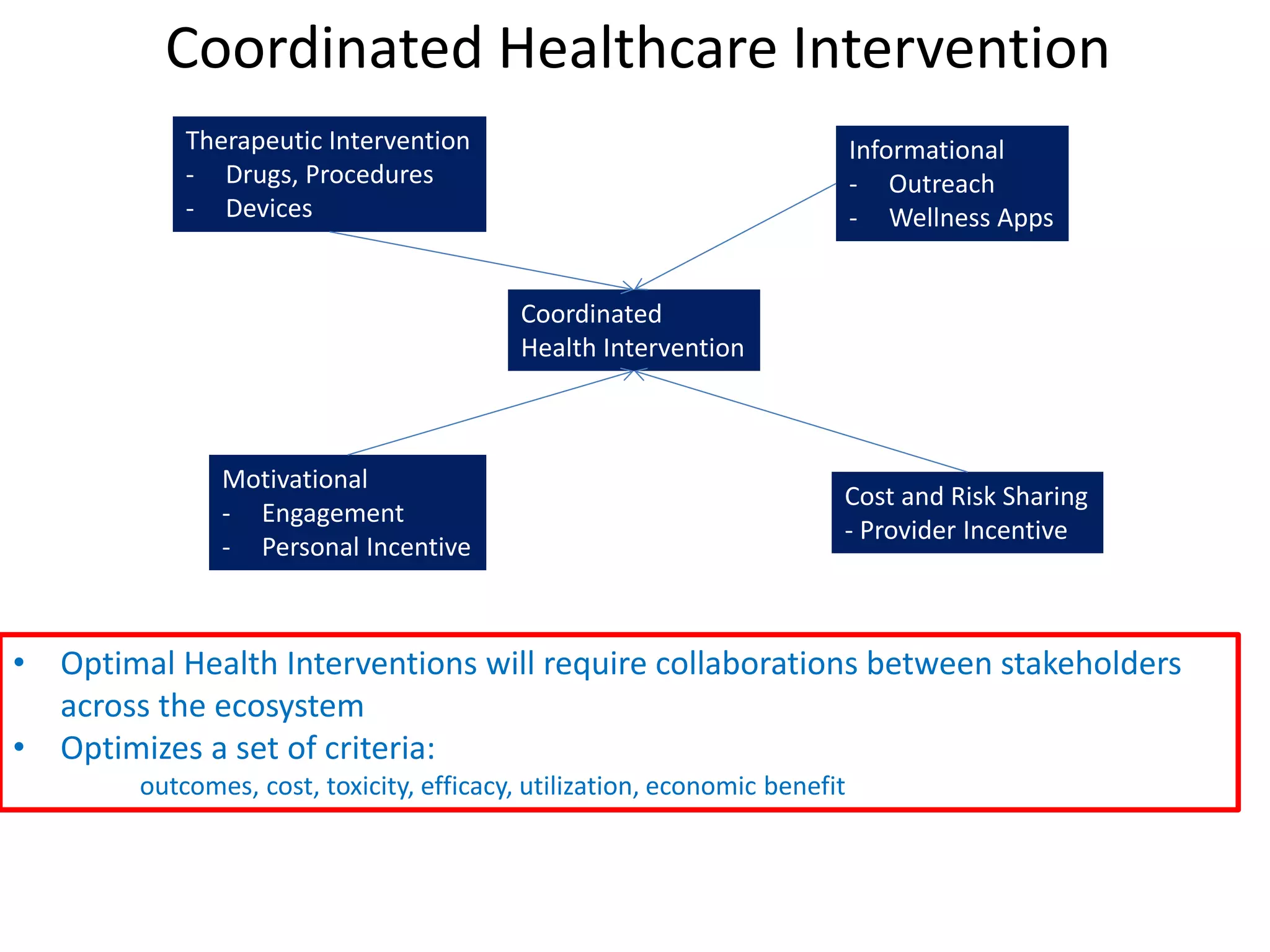
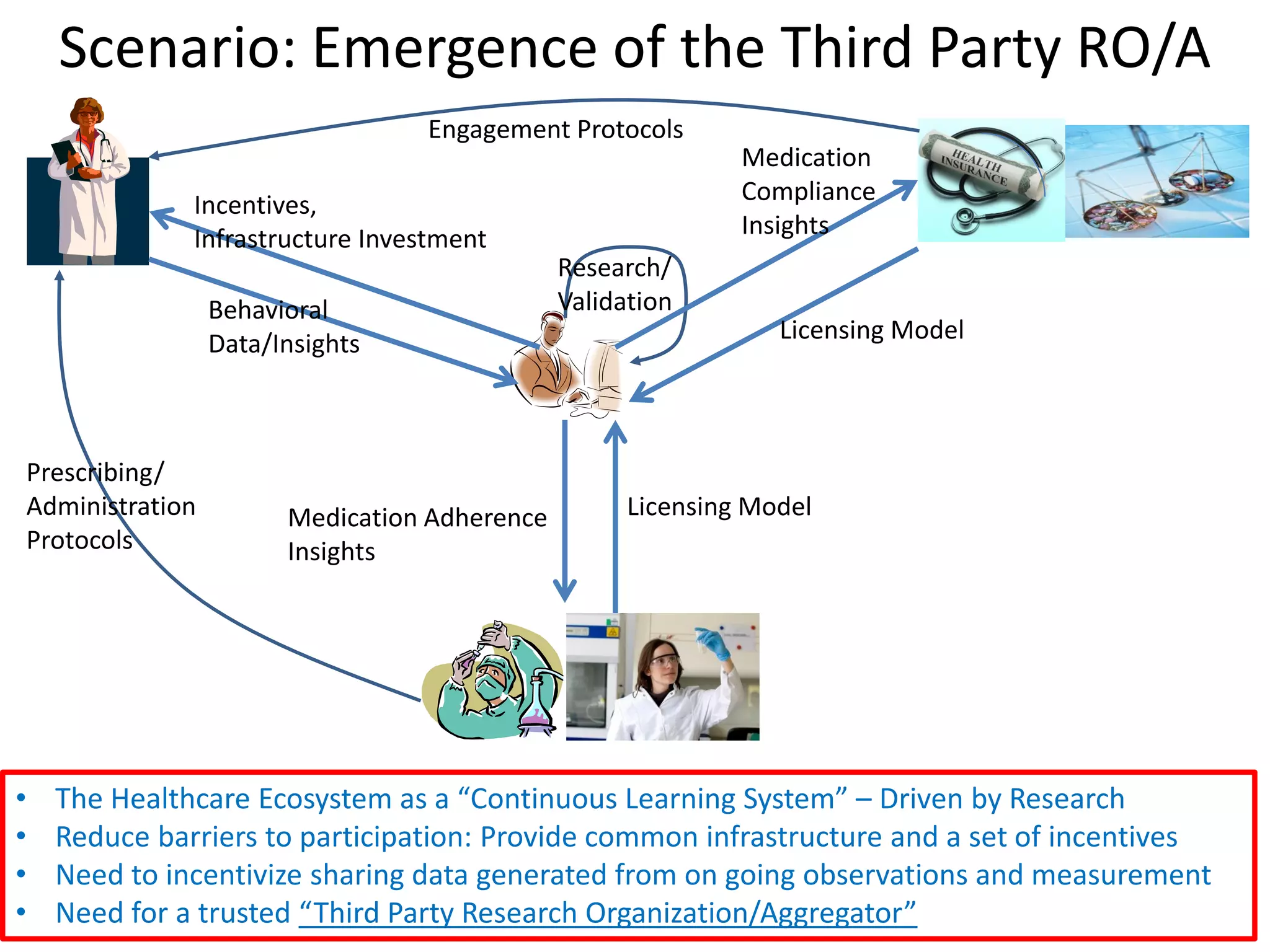
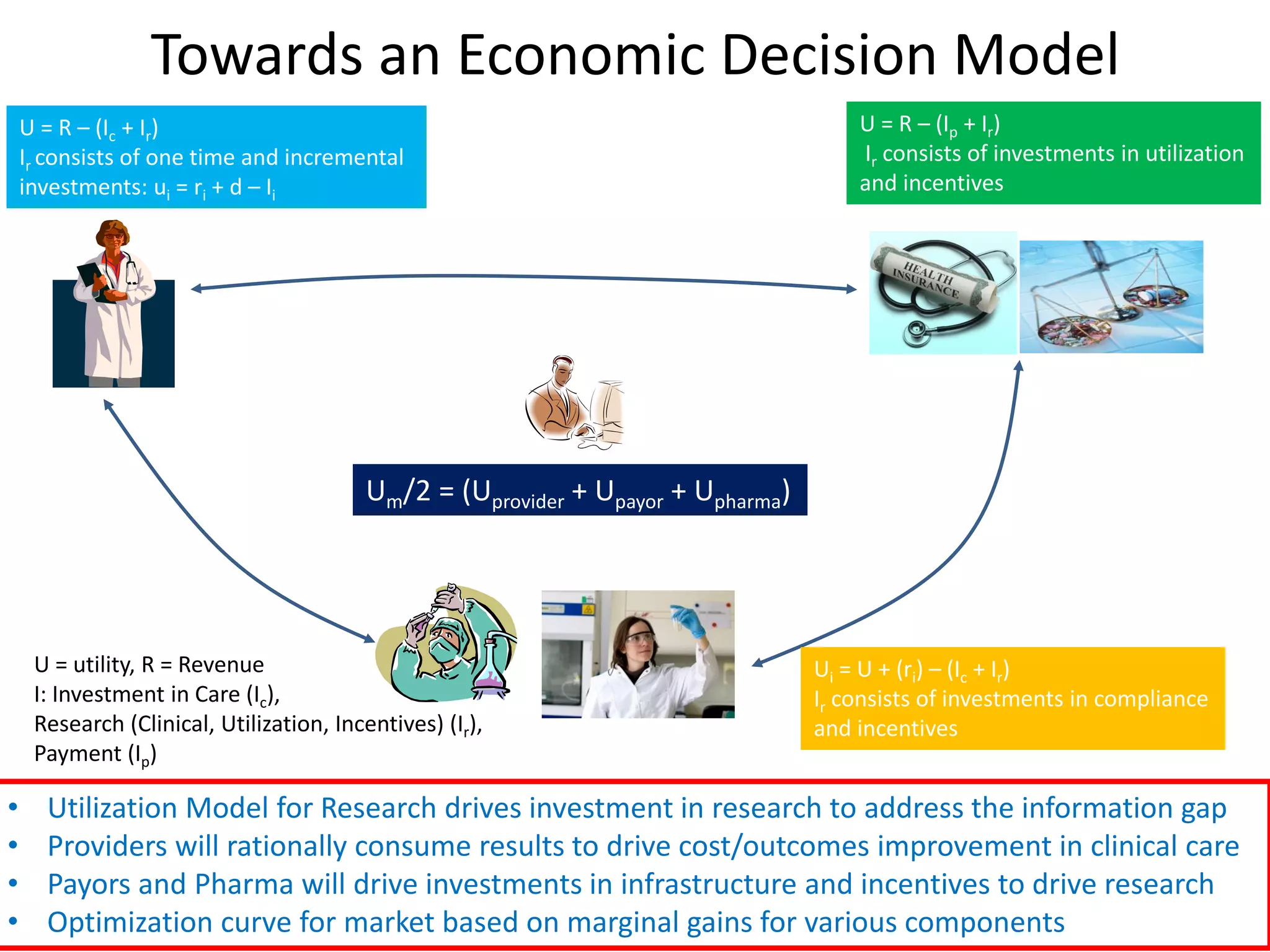
The document discusses the transition from a siloed healthcare ecosystem to a continuous learning ecosystem aimed at improving clinical outcomes and reducing costs through data innovation and collaboration. It emphasizes the need for coordination among stakeholders, the importance of sharing clinical insights, and the necessity of incentivizing research to address barriers in the current system. Conclusively, it proposes the development of an economic decision model and a roadmap to enhance collaboration and information sharing within the healthcare ecosystem.