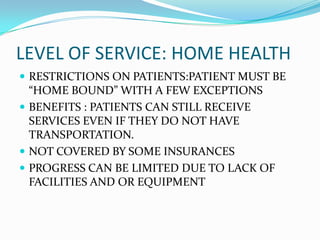
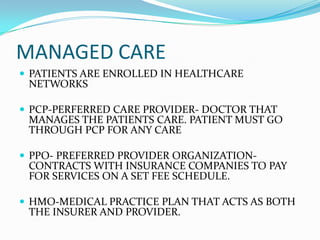
The document discusses different levels of care including acute care in a hospital setting, inpatient rehabilitation, skilled nursing facilities, outpatient care, and home health. It also covers reimbursement topics such as Medicare, Medicaid, managed care networks, and maximizing reimbursement through detailed progress notes. The overall purpose is to outline healthcare services and levels of care as well as payment and documentation best practices.