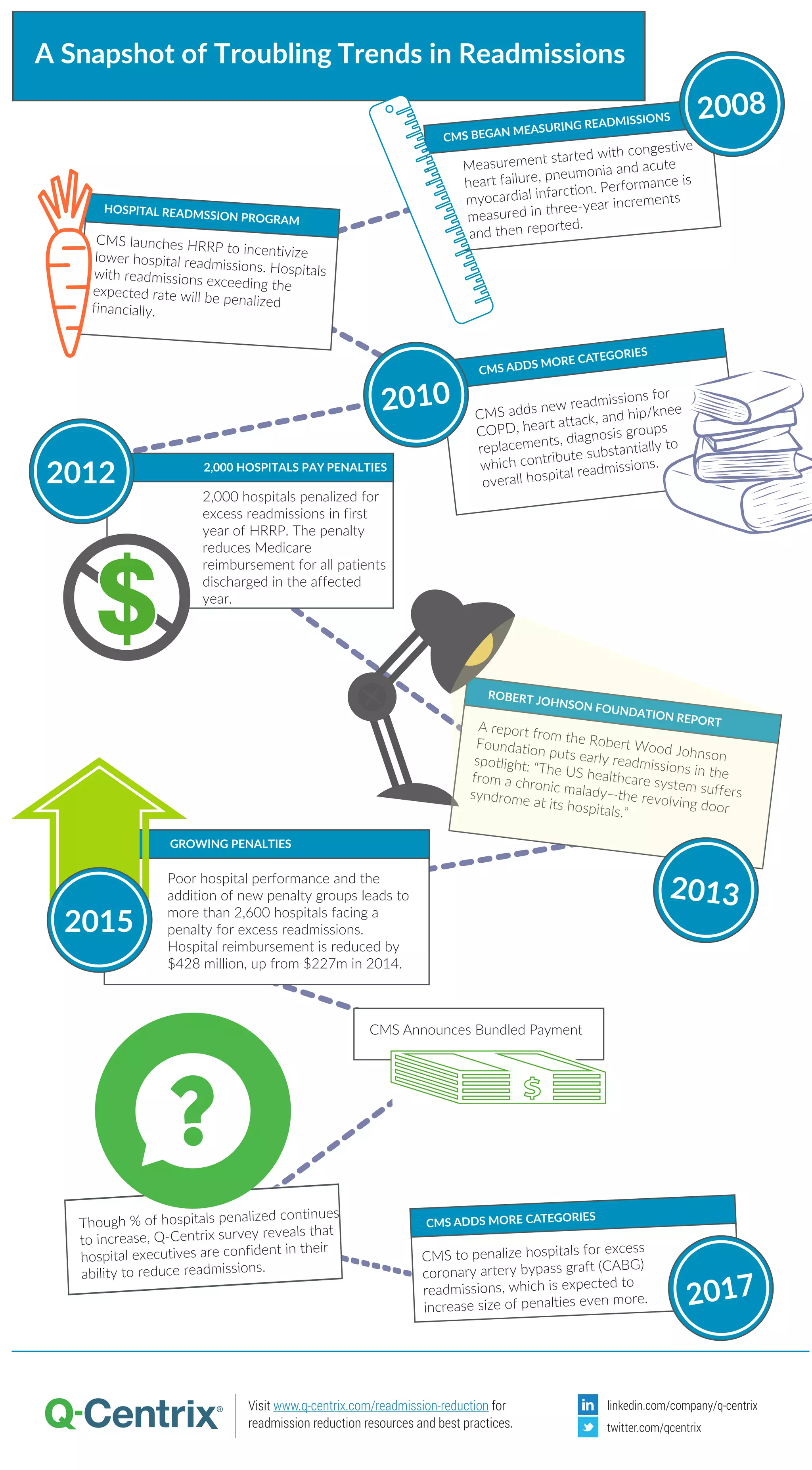
The Robert Wood Johnson Foundation report highlights the issue of hospital readmissions in the U.S., referencing the CMS's Hospital Readmissions Reduction Program (HRRP) which penalizes hospitals for excessive readmissions. Over 2,600 hospitals face financial penalties, with reimbursements reduced by $428 million due to poor performance and the addition of new penalty categories. Despite increasing penalties, a Q-Centrix survey indicates hospital executives remain confident in their ability to reduce readmissions.